National Medication Safety Programme Update
advertisement

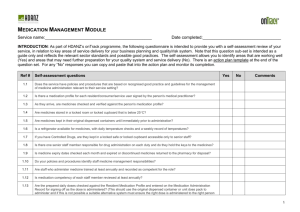
National Medication Safety Programme Update August 2012 Welcome to the third update from the National Medication Safety Programme. In this issue you can read about: the review of the national medication chart and design changes the national chart being developed for the aged residential care sector how junior doctor chart audits are contributing to a drop in medication errors at Wairarapa Hospital development of a measurement and evaluation framework for electronic medicine management initiatives the Partners in Care project Medication Safety Expert Advisory Group Chair Dwayne Crombie’s thoughts on medication safety new National Programme Director eMedicines, Anton Venter the New Zealand Universal List of Medicines the launch of the New Zealand Formulary the latest on the Go for Gold programme achieving targets for medicine reconciliation at admission. National medication chart – review and design changes In February 2011, West Coast District Health Board (DHB) became the first DHB to implement the national medication chart. Twelve months later, a review of the seven-day chart design began. The final design sought to balance the needs of all clinicians (ie, prescribers, administrators and dispensers) and the needs of all patient populations (ie, medical, surgical, mental health) while maintaining the medication safety principles on which the original chart design had been based. The review was based on feedback received from clinicians: via the electronic change register during the year from DHBs via email or in person during the long-stay chart pilot focus groups undertaken in four DHBs. 1 The review was also an opportunity to incorporate the paediatric charting requirements, after a separate consultation on paediatric requirements was conducted in February 2012. One of the recurring themes in the electronic change register was the need for a long-stay chart to reduce the re-prescribing required on long-stay wards and the possible transcription errors that could result. The long-stay chart pilot was conducted in four DHBs during 2011 and the feedback from the focus groups and the available audit results were used to inform the design of the new 16-day chart. The main changes to the chart design are: simplified front page requirements, ie, ‘Yes’ boxes taken out of the allergies and adverse reaction, special care required and supplementary chart sections addition of a barcode and a perforated cutting line for hospitals that need to scan the chart for document storage purposes the number of days has been increased from seven to eight to facilitate represcribing at weekly team meetings the introduction of a 16-day chart the number of medicines on a page has been increased in response to change requests that highlighted a difficulty in reviewing medicines when multiple pages had to be viewed the number of medicines on the ‘as required (PRN) medicine page’ has been increased in response to the needs of some surgical patients the number of administration time intervals has been reduced to create the space for the extra medicine lines a venous thromboembolism (VTE) prevention section has been included at the top of the regular prescribing page in response to requests from both the national VTE working party and individual DHBs paediatric requirements have been incorporated, ie, space to document the medicine dose calculation, ie, mg/kg/dose, an extra space to record weight, space for body surface area and gestational age the dose box design has been changed to clearly indicate where dose ranges should be prescribed and to highlight the figures before and after the decimal point. The Medication Safety Expert Advisory Group has agreed that a short-stay/one-day chart should be added to the suite of national medication charts. It is planned to have this chart available by the end of 2012. Each DHB has a lead who coordinates ordering medication charts. If your organisation would like to start using the charts, please discuss this with your medication safety team. National chart being developed for the aged residential care sector The team leading the project to develop a national medication chart for the aged residential care sector has met with a wide range of stakeholders since the beginning of April 2012. These meetings have provided useful information about the medication management issues faced by aged residential care multidisciplinary teams. 2 Currently, charts are used for prescribing and dispensing, and separate signing sheets are used to record administration of medicines. The following issues are being considered in designing a national chart for the aged residential care sector that covers prescribing, dispensing and administration of medicines: the work involved in charting medicines and maintaining the resident’s chart to avoid error-prone time-saving short-cuts reducing the potential for medication errors at all stages of the medication management process adopting as many of the safety features of the national medication chart as possible, given the differences between the aged care and hospital environments – particularly the way doses and instructions are recorded making the medication chart the main information resource for managing the resident's medication-related care considering the transfer of information about a resident's medicines between the primary and secondary care practitioners providing care to that resident. There will be a consultation phase in September when the draft design of the proposed medication chart for the aged care sector will be available for feedback. The design will be updated to reflect this feedback. The resulting chart will be used as part of a four-month pilot and the project team is seeking interested aged residential care facilities wanting to participate. For more information please contact Emma Forbes. Junior doctor chart audits contribute to medication error drop Junior doctors at Wairarapa Hospital are helping to reduce medication errors by auditing all the hospital’s medication charts. Each junior doctor audits around 60 charts for a week at both the beginning and end of their three-month rotation at the hospital. It’s one of a range of measures the hospital brought in before the national medication chart was introduced in September last year, to stop poor prescribing habits being carried over with the introduction of the new chart. Wairarapa DHB Chief Medical Officer, Alan Shirley, and Clinical Nurse Educator Lucy McLaren. Lucy is wearing the prescribing ‘reminder card’. Clinical Nurse Educator, Lucy McLaren, says the audits are done when the junior doctors’ workload eases in the early hours of the morning. “They’re looking for errors like illegible handwriting, numbers written incorrectly, allergies not being ticked and lack of signatures.” 3 Mrs McLaren says the national medication chart means everyone is now working to the same standard. “We’re seeing the benefit of that here and, hopefully they’re seeing it when junior doctors go back to their bigger hospitals as well. “We’re on our third group of junior doctors since the national medication chart came in, and because they’re also auditing each other, there’s an attitude of ‘don’t let the team down’ when they’re writing their own charts.” Mrs McLaren also regularly checks all the medication charts and follows up any prescribers of concern with Chief Medical Officer, Alan Shirley. “We’re definitely seeing an improvement in practice. Last week I could only find one error and that was from a consultant, so the junior doctors are doing really well. “According to our quality team, our medication error rate is dropping, and we’ve had some months with no errors.” Other measures introduced by Wairarapa DHB to improve prescribing habits included ensuring nurses felt supported to challenge poor prescribing. Prescribing ‘reminder cards’ listing the 10 key points from the national standards for prescribing were printed for nurses to wear on lanyards to help them check charts were complete and as a reminder to all staff to ensure charts were correct. A square of red duct tape has been placed on the floor by the controlled drugs cabinet in the busy medical surgical ward. When two nurses stand inside the square, it’s a signal to their colleagues that they are not to be disturbed because they are focussed on checking controlled medication before it’s given to a patient. “It’s a matter of constantly keeping a foot on the accelerator and the focus on patient safety,” says Mrs McLaren. Wairarapa DHB is also developing medication administration standards, which will review the common practice of nurses asking a colleague to check routine medication before it’s administered. “Research is starting to show that double checking is not that effective in reducing the number of medication errors, and can delay the medication getting to the patient.” Measurement and evaluation framework being developed The Commission is leading the development of a measurement and evaluation framework for the National Medication Safety Programme, with an initial emphasis on electronic medicines management (eMM) initiatives. The objective is to evaluate the roll-out of electronic prescribing and administration (ePA) and electronic medicine reconciliation (eMR) systems in four DHB sites. The DHBs participating in the roll out are Counties Manukau, Taranaki, Southern and Waitemata. Progress to date includes: the development of a draft overall evaluation framework and indicator set. This will be progressively refined based on feedback from experts, stakeholders and DHB site visits. 4 The key dimensions in the framework span the objectives of the Triple Aim and are: safety (harm reduction); cost effectiveness; effectiveness; system implementation and system design. Detailed indicators for the two initiatives are being developed that populate each of these elements visits to three of the DHBs have been completed, with a visit to the remaining site scheduled. The purpose of these initial visits is to document the pre-intervention state, describe the initiatives that will be implemented, and discuss the most suitable evaluation approach for the site. In the course of these visits, the team has also made useful observations about the experience with implementation to date. Learnings will inform subsequent DHB roll-out of the eMM initiatives. One of the challenges is the ability to collect accurate and timely data to support the agreed indicators and framework. As with any newly introduced electronic system, the reporting features and decision support functionality require considerable development and testing. The next steps for the measurement and evaluation project are: the finalisation of the evaluation approach for each of the DHB sites formulation of the methodology and agreeing the indicator set collection of baseline data by DHBs, against which the impacts of the eMM initiatives will be evaluated and which will also inform the Commission’s quality and safety marker workstream. Concurrently, the Commission is encouraging and supporting DHBs to adopt the Global Trigger Tool/ADE Trigger Tool methodology to identify where patient harm may be occurring and use the analysis of this information to initiate quality improvements at a local DHB level. The next steps for the measurement and evaluation project are: the finalisation of the evaluation approach for each of the DHB sites formulation of the methodology and agreeing the indicator set collection of baseline data by DHBs, against which the impacts of the eMM initiatives will be evaluated and which will also inform the Commission’s quality and safety marker workstream. Medication Safety Partners in Care project on consumer insulin information Partners in Care is a Commission-sponsored initiative, designed to provide two-person teams of a consumer and a clinician with the knowledge and skills to lead a consumer engagement project within a health and disability organisation. The Medication Safety Programme is represented by a team undertaking a project that aims to identify the information needs of adult insulin-dependent diabetics for the safe use of insulin. Key to the project is talking to patients about their experience when they were told – either in hospital or in a community setting – that they needed to use insulin. Input will be sought from clinicians in both primary and secondary care; and consumers and providers will be brought together to plan for the future. 5 The team will also partner with others working on diabetes and insulin projects, to ensure ‘safe use of insulin’ messages within the sector are consistent. More information about the Partners in Care project can be found on the Consumer Engagement section of the Commission’s website. Expert Advisory Group chair on the challenges of medication safety Medication Safety Expert Advisory Group chair, Dwayne Crombie, enjoys the challenge of setting ambitious goals for improvement and engaging people to reach those goals. Dr Crombie is Managing Director at BUPA, a health care provider that offers a range of care options including retirement villages, personal alarms and care homes. For eight years prior to this, he was Chief Executive of Waitemata DHB, where he helped create the first collaboration between DHBs on medication safety – resulting in the establishment of the Safe and Quality Use of Medicines Group (SQM). He sees medication safety as an area with great harm reduction potential. Dwayne Crombie ‘Medication is the commonest form of treatment, so mistakes can have wide reaching impacts and affect many people.” He says, before SQM, most of the collaboration on medication safety was within professional groups or within a specific institution. “At that time, DHBs were looking for ways to collaborate and medication safety was identified as a worthwhile, high profile topic. “SQM developed a national safe and quality use of medicines strategy, which led to conversations with the Ministry of Health, which in turn led to a proposal for funding a safe medicines management programme.” Dr Crombie says creating a connected information system which allows for a ‘single source of truth’ is one of the biggest challenges for the Medication Safety Programme. “There are two powerful forces involved in improving safety – creating an integrated technological system and increasing consumer understanding and participation. “The intricacies are mindboggling – some DHBs use electronic systems, some use printed material, and there are many different layers of information people have access to. “There is also human error to add to the mix. Some people may not take their medicines or may decide to take someone else’s, or add complementary products as well. “I believe there is a good understanding of the challenges and what’s required to meet them – and that means we’re a quarter of the way there.” 6 He believes the key is increased collaboration between everyone involved in the improvement process – clinicians, technology experts and consumers – and establishing the building blocks and platforms that can help to underpin this new way of working. “In a country this small, connecting people and their efforts is the most important thing.” About the Medication Safety Expert Advisory Group The Medication Safety Expert Advisory Group provides expert technical and clinical advice to the National Medication Safety Programme. It replaces the Safe and Quality Use of Medicines Group and aspects of the Safe Medication Management Programme Steering Group and is accountable to the Medication Safety Strategic Governance Group. See the April 2012 issue of this newsletter for a full list of group members. Welcome to Anton Venter – National Programme Director eMedicines The Commission and National Health IT Board welcome Anton Venter, who has been appointed to the role of National Programme Director eMedicines, within the National Medication Safety Programme. Anton – a registered pharmacist – will lead the introduction of electronic medicines management within New Zealand hospitals. One of his key tasks will be implementing the Go for Gold campaign. Commission CEO, Dr Janice Wilson, says Anton has a strong background in leading the development and implementation of information technology to improve the delivery of health care services. Anton Venter “Anton brings a wide range of skills to this role, including an understanding of clinical needs, and technical requirements and standards. He has strong networks in the health IT sector, and will ensure clinicians are kept engaged as electronic medicines management is implemented.” National Health IT Board Director, Graeme Osborne, says Anton Venter is a clinical leader who can motivate people to work differently. “We are very pleased to have his energy and insight engaged in the National Medication Safety Programme.” Anton is based at the National Health IT Board, and comes to his new role from Healthcare of New Zealand, where he was National Manager, Integrated Care. He can be contacted on 04 816 2068, 021 832 260, or anton_venter@health.govt.nz 7 What’s new in the New Zealand Universal List of Medicines? The New Zealand Universal List of Medicines (NZULM) combines standardised medicine descriptions from the New Zealand Medicines Terminology (NZMT) with information from Medsafe and the PHARMAC Pharmaceutical Schedule to form an easily accessible one-stop shop for medicines information. NZULM is one of the foundations for improving safe and quality use of medicines. The standardised descriptions provided by the NZMT are designed to promote safe medicines use through clear, unambiguous naming and the NZMT’s system of describing the strength of a medicine avoids known risk factors which can lead to dosage mistakes. As the various clinical management systems adopt the NZULM as their medicines information source, the benefits of these descriptions flow into every day clinical practice. July 2012 marked a year since the NZULM was released for general use. It is being used more and more by clinicians across the sector. NZULM information can be accessed through the website, via smart phone apps on Android, iPhone and Windows 7 phones; is increasingly being embedded in clinical management systems for general practitioners, community pharmacists, hospital doctors and hospital pharmacists; and is powering the New Zealand Formulary and the NZ ePrescription service. Over the last year the NZULM team has introduced a series of improvements to the NZULM. These include: all listed medicines are now identified by their WHO ATC (Anatomical Therapeutic Classification) code. This allows clinicians to identify medicines with similar characteristics when making therapeutic decisions. To experience the advantages of searching for medicines information in this way, click here all listed medicines now have prescribing terms for their generic and trade names. This will make it easy for clinicians to select medicines either generically or by trade name when prescribing or dispensing using their practice management software all medicine listings now provide structured information about their active ingredients. This will allow vendors to provide alternate ways to document a prescription and to provide enhanced decision support Medsafe now uses NZMT descriptions and identifiers to manage applications for new and changed medicines. This means that from now on information about these medicines will be more easily and safely incorporated in clinical and management systems (over 1000 new or changed medicine products were listed in the NZULM in the last year). What’s next? The current focus is very much on further adoption of the NZULM in clinical and management systems. Enhancements planned include improvements to the website search, barcode information to support computer-aided product identification, Tall Man Lettering to further reduce the risk of medicines with similar names being confused, and 8 providing information about the other non-medicinally active constituents in medicines to improve sensitivity and allergy checking. For more information about the NZULM and to apply for a new NZULM medicine listing please see the website. The New Zealand Formulary launched Around 130 key stakeholders and health professionals gathered in Wellington on 19 July to celebrate the launch of the New Zealand Formulary (NZF). The NZF (based on the British National Formulary and specifically adapted for New Zealand) provides robust clinical information about the use of medicines in one place, alongside PHARMAC and Medsafe information. It is a onestop shop for health professionals looking for high quality and up-to-date information about medicines that are used in New Zealand. Associate Minister of Health, Hon Peter Dunne, said the need for a coherent approach to the use of medicines was one of the drivers for the establishment of the New Zealand Medicines Strategy and the reason why Actioning Medicines New Zealand (the action plan for the New Zealand medicines strategy) committed to the development of a medicines formulary in 2007. Mr Dunne talked about a future in which health professionals could access the NZF via an eReader or smart phone. He said the NZF would have “extra value when incorporated into clinical health IT systems”. The NZF was adapted for New Zealand use by BPACnz, BPACinc and the UK-based Royal Pharmaceutical Society, under the leadership of Professor Murray Tilyard. Having this information available at the point of care will promote consistency of practice across New Zealand, reduce medication errors and promote safer and more appropriate medicines management. The NZF is built on the NZULM and coded using standardised medicines terminology. This allows for a fully interoperable medications management system across the continuums of care. The sector is already showing its readiness for the NZF. Auckland University’s School of Pharmacy has begun incorporating the NZF into its teaching programme, and the team at Health Pathways is looking at ways to incorporate the NZF into its referral pathways for Canterbury, South Canterbury, West Coast, Nelson Marlborough, and Hutt Valley DHBs. A number of hospitals and health-related software vendors are also looking to utilise the NZF. The NZF is available free of charge to all health professionals via the website and a downloadable eBook. 9 IN BRIEF Going for Gold Phase two of the roll out of electronic medicine reconciliation (eMR) and electronic prescribing and administration (ePA) is continuing. On 9 July, Taranaki DHB went live with ePA in its first ward – one of three wards (120 beds) aiming to roll out ePA by early next year. It is the second DHB to go live with ePA after Southern, which completed its ePA pilot in two wards in October last year. Waitemata DHB is preparing to go live with ePA in November. eMR is currently carried out at Counties Manukau, Waitemata and Taranaki DHBs and is expected to go live in Auckland DHB later this year. Dr Chris Hopkins, Dr Anna Mearns and clinical pharmacist and trainer Tracey Watson. Chris and Anna are wearing ‘Naki’ scarves to support Go for Gold and ‘go-live’ day Taranaki DHB has also integrated ePA with its pharmacy system and its Pyxis system for automated drug dispensing. By early next year the DHB is hoping to have added eMR and ePA integration to the mix, which will see it having a first stage end-to-end integrated electronic medicines management system in use. This would mean there would be no need for manual transcription of information from the prescribing system into the pharmacy system and Pyxis system or into the eMR and electronic discharge summary system. Transcription is error prone and therefore potentially unsafe but also inefficient. Under the Go for Gold programme, DHBs are encouraged to have achieved ‘gold’ level medication management by the end of 2014, with the aim of having all DHBs participating in the eMM programme from 2012. There are bronze, silver and gold levels of medication management: bronze: paper-based national medication chart and paper-based medicine reconciliation process silver: transition to eMR and ePA gold: eMR and ePA throughout the hospital. Achieving targets for medicine reconciliation at admission While the Commission has a role in leading and driving the quality and safety agenda, we can only make progress by working in co-operation and co-ordination with the wider sector. As part of this collaboration, we are looking to DHBs to set and drive their own achievement targets around medicine reconciliation for 2012/2013 and the out years. The Commission will be engaging directly with each DHB on this matter. The expectation is for DHBs to steadily increase the number of patients who have medicine reconciliation (MR) on admission (whether electronic or paper-based) towards 100 percent 10 of all prioritised patients based on a local or national prioritisation criteria. Of course, some DHBs may prefer to aim for all patients having medication reconciliation at admission. We are aware DHBs are continually expanding their medicine reconciliation services and would like to capture this achievement. While there is currently no national tool available to determine priority patients for medicine reconciliation, this does not need to hinder the reporting of current progress being made by the sector. Counties Manukau DHB has started to validate its tool, which identifies patients at most risk of medication-related harm. An expected output of this validation is the identification of the individual components of greatest value in determining a patient at most risk, that could be used nationally. Contact If you have any comments or queries related to the National Medication Safety Programme, please email info@hqsc.govt.nz. Further information about the programme is available on the Health Quality & Safety Commission’s website; and the National Health IT Board’s website. 11