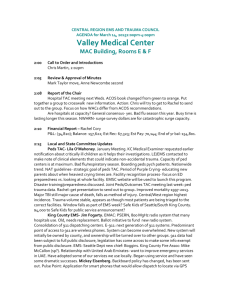
final 2013 - emergency preparedness and healthcare
advertisement

EMERGENCY PREPAREDNESS AND HEALTHCARE PLAN Introduction NAME The organization will be known as Northeast Texas Regional Advisory Council. (NETRAC). NETRAC represents Trauma Service Area F (TSA-F), as designated by the Texas Department of Health (TDH). TSA-F includes the following counties: Bowie County, Texas Cass County, Texas Delta County, Texas Hopkins County, Texas Lamar County, Texas Miller County, Arkansas Morris County, Texas Titus County, Texas Red River County, Texas MISSION STATEMENT Provide a comprehensive continuum of quality health care for all victims of disasters, trauma, and acute care in TSA-F without regard to age, race, sex, color, national, origin, disability, religion, or ability to pay. Provide disaster preparedness, trauma, and acute care prevention activities and education to professionals and the public within TSA-F. PRINCIPAL OFFICE The principal office of the Corporation in the State of Texas shall be located at 4090 Summerhill Square - Texarkana, Texas. The Corporation may have such other offices, either in Texas or elsewhere, as the General Assembly may determine. The General Assembly may change the location of any office of the Corporation. REGISTERED OFFICE AND REGISTERED AGENT The Corporation shall comply with the requirements of the Act and maintain an office and registered agent in Texas. The principal office of the Corporation may, but need not be, in the State of Texas. The General Assembly may change the main office or principal place of business and the registered agent as provided in the Act. Texas Trauma Service Area F consists of 9 counties. Although there are eight (8) hospitals serving these 9 counties, only five (5) have bed capacity exceeding 100. As of July 1, 2012 , the following TSA-F hospital Level 1: None Level 2: None Lead Level 3: Titus Regional Medical Center – Mt Pleasant, Texas (Titus County) Level 3: Wadley Regional Medical Center – Texarkana, Texas (Bowie County) Level 4: East Texas Medical Center – Clarksville, Texas (Red River County) Good Shepherd Medical Center – Linden, Texas (Cass County) Hopkins County Memorial Hospital – Sulphur Springs, Texas (Hopkins County) Non-designated CHRISTUS – St. Michaels – Texarkana, Texas (Bowie County) Paris Regional Medical Center – Paris, Texas (Lamar County) The original trauma plan for TSA-F was distributed July 13, 1999 to the Regional Advisory Committee members in preliminary form. The plan and suggested modifications were voted upon. The plan in final form was signed by the Chairperson of NETRAC and forwarded to the Texas Department of Health for approval. The Trauma Plan for Trauma Service F will be reviewed annually by the Board of Directors and changes will be presented to the membership at the next scheduled meeting. This Trauma Plan incorporates major trauma triage criteria to identify those persons to be transported to a trauma center. The Plan also establishes a formal evaluation mechanism to determine whether trauma patients receive appropriate care. These mechanisms encompass data recording and collection, evaluation and analysis of data, and incorporation of needed changes as recommended by various quality assurance and improvement monitors. The collection, evaluation and improvement actions will be a cooperative process among physicians, prehospital, and hospital personnel. RAC Executive Officers and Board Members NETRAC OFFICERS 2012 - 2013 Chair: Chair Elect: Chair Past/Vice: Executive Director: Treasurer: Assistant Treasurer: Secretary: Russell VanBibber Elected 10/09 Robin Gage Mark Mallory Shae Watson Norman Prewitt Meagan Beauchamp Vornetta Compton NETRAC OFFICERS AND BOARD MEMBERS 2012-2013 Chair: Chair Elect: Chair Past/Vice: Executive Director: Treasurer: Assistant Treasurer: Secretary: Russell VanBibber Elected 10/09 Robin Gage Mark Mallory Shae Watson Norman Prewitt Meagan Beauchamp Vornetta Compton Education: EMS/Aeromedical: Hospital: Nurse: At-Large: Rehab: Physician: Response Partner: Blaine Jones Brent Smith Mark Mallory Bertha Evans Connie Stauter Scott Reid Elected 10/11 Elected 10/11 Elected 10/11 Elected 10/10 Elected 10/11 Elected 10/10 Mary Beth Rudel Elected 10/10 System Plan Participation It is crucial that each involved entity be accountable for participation within the Regional Advisory Council for TSA-F to remain in compliance with standards set forth by the Texas Department of Health. Only with collective participation, can an effective and efficient trauma system plan function on a region-wide basis. Regional Advisory Council meeting notices are published on the NETRAC Website and are emailed to the following, but not limited to: Health Care Facilities, i.e., Hospitals Emergency Medical Services (EMS) Physicians from various specialties Emergency Response Parnters County and/or City Clinics NETRAC Executive Board Members NETRAC Committee Chairs and Committee Members Non-profit community health and safety agencies At each RAC meeting, a general roster is placed for each attendee to sign-in by name and representing facility. These rosters serve as the identifiable means of tracking what facilities/agencies have been represented and are considered to be participating in the RAC. General sign-in rosters are also kept by individual committee chairs and serve as further tracking information of what facilities are represented and participating in various committee-planning stages. Participation is defined as individuals or entity representation actively pursing interest and involvement in the priorities and goals set forth by the Regional Advisory Council for TSA-F as defined by each committee RAC approved mission statement and plans. To confirm the above, individuals or entity representatives must be accounted for by attending three or more RAC meetings per year, AND, individuals or entity representatives must attend two or more committee meetings of their choice, AND, entities must be in compliance of the Regional Advisory Council Emergency Preparedness and HealthCare plan for TSA-F within the guidelines set forth by the Texas Department of State Health Services. Persons involved in system planning are as follows but not limited to... Health Care Facilities, i.e., Hospitals Emergency Nurses Association and members Physicians from various specialties EMS Agencies County and/or City Clinics NETRAC Executive Board Members NETRAC Disaster Preparedness Committee Chairs and Committee Members Mobile Medical Unit: Communications: Northeast Texas Regional Medical Operations Center (NETMOC): Symposium Committee: Mobile Medical Unit Committee Members: Shae Watson Robin Gage Karen Stephens Bertha Evans Russell VanBibber Mark Mallory Meagan Beauchamp Russell Thrasher Brent Smith Wade Cannon Sarah Campbell Frank Williams Vornetta Compton Norman Prewitt Kent Klinkerman Greg Friesen Jeff Nichols Dave Dutton Beckie Lewis JJ Vaughan Scott Reid Keith Kelley Sandra Jeffrey Danny Wilburn Mike Western Bruce Bushee Gloria Cooper Alasha Williams LeighAnnScates Dr. Michael Williams Robin Gage, Chair Karen Stephens, Chair Mark Mallory, Chair Shae Watson, Chair Shae Watson, Chair Communications Members: Shae Watson Mark Mallory Russell VanBibber Russell Thrasher Kent Klinkerman Brent Smith Scott Conway Scott Reid NETMOC Committee Members: Shae Watson Mark Mallory Norman Prewitt Meagan Beauchamp Russell Thrasher Bertha Evans Karen Stephens Vornetta Compton Drills/Exercise Committee Members: Shae Watson Norman Prewitt Bertha Evans Blaine Jones Keith Kelley Mary Beth Rudel Vornetta Compton Symposium Committee Members: Shae Watson Robin Gage Vornetta Compton Bertha Evans Meagan Beauchamp Liberty Bailey Russell VanBibber Russell Thrasher Blaine Jones Dave Dutton Carol Slider NETRAC Trauma/Acute Care Committee Chairs and Committee Members Acute Care: EMS/Aeromedical: Hospital/Registry/Quality Improvement: Injury Prevention/Pediatrics/Education: Acute Care Committee Members: Kathy Griffis Dr. Khalid Malik Dr. Nancy Griffin Denise Dowell SherFomby Cyndi Chamblee EMS/Aeromedical Committee: Brent Smith Danny Wilburn Mark Mallory Russell Thrasher Brent Smith Kent Klinkerman Ricky Draper Dave Dutton Jim Spier Scott Miller Denis Roach Patrick Barkley Stephanie Jackson Hospital/Registry/QI Committee: Keith Kelley Vornetta Compton Bertha Evans Dr. Morney Sorenson Leigh Ann Scates Meagan Beauchamp BeckieCressionnie Louise Thornell Liberty Bailey Jeff Nichols Kathy Griffis, Chair Brent Smith, Chair Keith Kelley, Chair Blaine Jones, Chair Injury Prevention/Pedi/Education Committee: Blaine Jones Robin Gage Russell VanBibber Melissa Granberry Shannon Cox EMERGENCY PREPAREDNESS Northeast Texas Preparedness Coalition(NETPC) The Northeast Texas Regional Advisory Council(NETRAC) Board of Directors(Board) and Ark-Tex Council of Governments (ATCOG) recognizes the Northeast Texas Preparedness Coalition (NETPC) as the Preparedness Coalition for the geographic area encompassing Trauma Service Area F (TSA-F) and ATCOG and as a Standing Committee of the NETRAC Board, with the authority, responsibilities and specific duties as described in this Charter. Definition: For the purposes of this instrument, Charter shall be defined as: “A written instrument given as evidence of agreement.” Composition of the NETPC Governance Board: The NETPC Governance Board shall consist of the following: Voting Members: 3 - Hospital Representatives (1 Lead Level III Facility; 1 – Level III Facility; 1 – Level IV Facility) 3 - EMS Representatives(1 Large EMS Agency; 1 – Medium EMS Agency; 1 – Small EMS Agency) 1 - City Emergency Management Representative; 1 - County Emergency Management Representative; 1 - Public Health Representative; 1 - Response Partner Representative; 1 - At Large Position chosen by NETRAC Board Chair; Non-Voting Members: NETRAC Executive Director NETRAC Chair Hospital Planning Group Chair NETRAC Treasurer ATCOG Homeland Security Manager NETPC Governance Board Membership Votes: Voting: All members of the NETPC Governance Board shall have voting rights with the exception of the NETRAC Executive Director and the ATCOG Homeland Security Manager. No employee of these two organizations shall have voting rights in the NETPC. Non-Voting: Invited guests and any employee(s) of the two organizations, including, but not limited to, the organization’s Executive Director. NETPC Coalition Membership: The NETPC Coalition should be made up of the following members: Primary Members: Participating NETRAC Hospitals and Healthcare organizations Participating NETRAC EMS Agencies Participating NETRAC Colleges/Universities Participating ATCOG Public Safety Agencies Elected Officials Essential Partners Members: Emergency Management/Public Safety Department of State Health Services (DSHS) Emergency Medical Task Force (EMTF) Long-term care providers Mental/Behavior health providers Private entities associated with healthcare (e.g., Hospital Associations) Specialty service providers (e.g., dialysis, pediatrics, woman’s health, stand-alone surgery, urgent care) Support service providers (e.g., laboratories, pharmacies, blood banks, poison control) Primary care providers Community health centers Local/Public health Tribal healthcare Federal entities (e.g., National Disaster Medical System (NDMS), Veteran’s Affairs (VA) hospitals, Indian Health Services (IHS) facilities, Department of Defense facilities) Additional Healthcare Coalition partnerships/memberships: Local and state law enforcement and fire services Public Works Private organizations Non-governmental organizations Non-profit organizations Volunteer Organizations Active in Disaster (VOAD) Faith-based Organizations (FBOs) Community-based Organizations (CBOs) Volunteer medical organizations (e.g., American Red Cross, Medical Reserve Corp, CanHelp 211) Others partnerships as relevant Mission and Scope: The mission and scope of the NTCP Coalition is to encourage collaborative healthcare community planning and emergency preparedness planning to natural and man-made disasters affecting the NETRAC and ATCOG region by providing an aligned forum for persons, businesses, healthcare entities, and public safety agencies within or surrounding the geographic boundaries of NETRAC and ATCOG. Responsibilities, include, but are not limited to, the following: 1. 2. 3. 4. 5. 6. 7. 8. Coordinate with local, regional and state officials/jurisdictions in planning efforts for the healthcare community and emergency preparedness community. Identify and determine gaps in planning, resources, education, or training and develop action plans to support educational and process refinement. Facilitate integration with local, regional and state response partners. Assist in development and execution of exercises and drills based on identified needs/issues, formulate corrective action plans, and perform follow-up measures to ensure best practices have been instituted. Ensure sustainment of medical coordination through support of the Northeast Texas Medical Operations Center. Coordinate planning with response partners for unique needs of special medical populations/at-risk individuals. Disseminate planning and response initiatives. Provide and receive guidance and recommendations to/from the NETRAC Board, ATCOG and other committees, including ad hoc committees, on planning initiatives, program development and grant expenditures. The NETPC Coalition may establish subcommittees as part of the committee structure designated to accomplish these responsibilities. REPORTING STRUCTURE: The NETPC Governance Board reports each meeting to the NETRAC Executive Board and ATCOG. CHAIR: The Chair of the NETPC Governance Board will be appointed by the NETRAC Chair and will serve a two year term. TERM: NETPC Governance Board Members will be appointed for a term of two years unless representation is positiondesignated by the NETRAC Executive Board. ROLE OF NETPC CHAIR: The Chair of the NETPC is responsible for the following: Working with the NETRAC Executive Director and ATCOG Homeland Security Manager on setting the agenda and ensuring that agenda items are addressed. Facilitating achievement of committee priorities. Communicating the activities of the NETPC to the NETRAC and ATCOG Board of Directors and following up on issues identified. Identifying planning gaps within the purview of the NETPC and addressing those issues in an appropriate manner. Referring planning gaps or concerns outside the purview of the NETPC to the appropriate committees/departments ATTENDANCE: Members of the NETPC Coalition are expected to attend (75%) of all meetings annually and actively participate in all meetings. If an NETPC member is unable to attend, this should be communicated in advance to the NETPC Chair, NETRAC Executive Director, or the ATCOG Homeland Security Manager. Annually, the Northeast Texas Regional Advisory Council (NETRAC) – Hospital Preparedness Group reviews the regional Hazardous Assessment. This assessment aids in annual planning for our region. Figure 1: NORTHEAST TEXAS HAZARD MATRIX HAZARD TYPE: FREQUENCY WARNING TIME SEVERITY RISK PRIORITY Unlikely Minimal Catastrophic Low Highly Likely 6-12 hours Limited High Likely 24+ hours Limited Medium Unlikely 24+ hours Negligible Low TORNADO Highly Likely Minimal Catastrophic High WILDFIRE Likely Minimal Critical Low WINTER STORM Likely 24+ hours Catastrophic Medium Possible 24 + hours Critical High Possible Minimal Critical Medium NATURAL EARTHQUAKE FLASH FLOODING FLOODING (RIVER OR TIDAL) HURRICANE ENDEMIC/PANDEMIC MAN-MADE CHEMICAL/HAZARDOUS MATERIALS DAM FAILURE Unlikely Minimal Critical Low Likely Minimal Limited Medium Unlikely Minimal Catastrophic Low FREQUENCY WARNING TIME SEVERITY RISK PRIORITY Highly Likely Minimal Critical Medium Possible 6-12 Hours Critical Low Highly Likely Minimal Limited High CIVIL DISORDER Unlikely 6-12 Hours Negligible Possible EXPLOSION Possible Minimal Limited Low WEAPONS ASSAULT Possible Minimal Limited Low TERRORISM - CHEMICAL Possible Minimal Catastrophic Low TERRORISM - BIOLOGICAL Possible Minimal Catastrophic Low TERRORISM - RADIOLOGICAL Possible Minimal Catastrophic Low TERRORISM - NUCLEAR Unlikely Minimal Catastrophic Low TERRORISM - EXPLOSIVES Possible Minimal Catastrophic Low FIRE NUCLEAR FACILITY INCIDENT HAZARD TYPE: POWER OUTAGE WATER SYSTEM FAILURE ACCIDENTS (TRANSPORTATION) TERRORISM – COMMUNICATIONS FAILURE Possible Minimal Critical Medium MOBILE MEDICAL UNIT (MMU): In 2006, NETRAC purchased a 28-bed field deployable tentage system. NETRAC also purchased supplies and equipment to care for patients within our region. The MMU use the ICS Structure for operations. Northeast Texas Regional Medical Operations Center (NETMOC): During the event of a disaster or hazardous event within our region, the NETMOC will act as the Health and Medical Component for regional Emergency Operations Centers, and the District Disaster Centers. “Mission Statement” “To aid and provide assistance by coordinating regional assets and resources during the time of disasters.” NETMOC POLICY AND PROCEDURE: LOCATION OF ACTIVATION Location of Activation: Set-up at and with the MACC at the ATCOG – 4808 Elizabeth Street - Texarkana, TX 75501 NETMOC can also become a Mobile MOC to be deployed within the region NETMOC POLICY AND PROCEDURE: ACTIVATION CRITERIA Activation Criteria: Any local disaster that exceeds the resources of the local Emergency Operations Center Upon request of the State SOC and State DDC Upon request of the Mobile Medical Asset needs NETMOC POLICY AND PROCEDURE: ACTIVATION AUTHORITY Activation Authority – the following have activation authority MACC RAC Chair Executive Director Executive Board Members NETMOC POLICY AND PROCEDURE: STAFFING Address Staffing: Shifts will be 12 hours Minimum of 1 person per entity per 12 hour shift Must have ICS 100, 200, 700, and 800 NETMOC PROCESS FLOW AT THE MACC (NETMOC duties: Assign patients To hospitals in/out of RAC; EMS Deployment; Resources Deployment) NETMOC EOC Medical Incident Commander needs to be the 1st Responder on the scene (Identifies patients as: Red, Yellow, Green, or Black) MEDICAL INCIDENT COMMANDER COMMANDER MOBILE MEDICAL UNIT (MMU) COMMITTEE: The NETRAC MMU Committee provides oversight for all the NETRAC MMU operations, to include planning, staffing, transportation efforts for deployment. NORTHEAST TEXAS REGIONAL MEDICAL OPERATIONS CENTER (NETMOC) COMMITTEE: The NETRAC NETMOC Committee provides health and medical directions for regional response partners, Disaster District Chairs, and State Medical Operations Center during the effort or a disaster. COMMUNICATIONS COMMITTEE: The NETRAC Communications Committee provides oversight for all the NETRAC Communications Systems. The committees focus is to ensure our region has interoperable communications and can demonstrate vertical and horizontal communications with all RAC agencies and Regional Response Partners. NETRAC Communications Systems consist of the following: WebEOC: WebEOC is the original web-enabled crisis information management system and provides secure real-time information sharing to help managers make sound decisions quickly. Originally developed for public safety and emergency management officials, WebEOC is now also used also for routine operations in private corporations, public utilities, domestic and international airlines, healthcare associations, and universities, as well as by government at every level---city, county and state agencies nationwide and NASA, EPA, and other federal agencies within the Departments of Defense, Energy, Agriculture, and Health & Human Services. EMSystems: Internet based system that captures Hospital Bed availability and EMS availability. Immediate Response Information System (IRIS): Regional communications call down system for Mass Notification. IRIS, the Immediate Response Information System, is a system for broadcasting alerts to multiple communication devices simultaneously via a secure web-based administrator interface, designed and developed by TechRadium, Inc. Alerts are delivered according to organization and/or individual user preferences including multilingual translations. IRIS has multiple options for message creation including text-to-speech, a method for recording voice and saved alerts. Two other key components of the system are the user data management module and the system reporting module. Texas Disaster Volunteer Registry (TDVR): – statewide system using for credentialing licensed personnel, i.e. Physicians, Nurses, Paramedics, EMT’s, Physicians Assistants, Nurse Practioners, and Lay-persons. DRILLS/EXERCISE TEAM/COMMITTEE: The NETRAC Drills and Exercise Committee is responsible for aiding the Executive Director with planning and scheduling or regional disaster preparedness courses/education, regional drills and exercises. SYMPOSIUM COMMITTEE: The NETRAC Symposium Committee is responsible for aiding the Executive Director in planning efforts for our Annual Disaster Preparedness and Healthcare Symposium. EMERGENCY MANAGEMENT TASK FORCE (EMTF): The Emergency Management Task Force is a state project with a team goalto work together to provide a well coordinated response in offering rapid professional medical assistance to support emergency medical operation systems during disaster events or incidences. The EMTF Team is made up of four components: RN Nurse Strike Teams, Mobile Medical Unit Teams, Ambulance Strike Teams, and Ambus. NORTHEAST TEXAS PREPAREDNESS COALITION: The Northeast Texas Preparedness Coalition is collaboration and co-chaired by the NETRAC and Ark-Tex Council of Governments. The committee is made up of regional response partners and works to collaborate all disaster preparedness efforts and planning. TRAUMA AND ACUTE CARE HEALTHCARE SYSTEMS The NETRAC General Assembly is made up of four committees: Hospital/Registry/Quality Improvement; Education/Injury Prevention/Pediatric; Acute Care; EMS/Aeromedical HOSPITAL/REGISTRY/QUALITY IMPROVEMENT COMMITTEE: The NETRAC Hospital/Registry/Quality Improvement is responsible for aiding in the implementation of regional hospitals policies and procedures as it relates to Trauma/Acute Care and Disaster Preparedness. The committee helps in the development of the Regional Trauma Registry Programs, development of Registry Reports, and Performance Improvement. This committee also assist the Education Committee by supplying registry information to help develop Regional Injury Prevention Programs. EDUCATION/INJURY PREVENTION/PEDIATRIC COMMITTEE: The NETRAC Education/Injury Prevention/Pediatric Committee is responsible for developing and scheduling Trauma, Acute Care, and Disaster Preparedness educational courses and trainings. The committee works with community partners to promote Injury Prevention activities and pediatric educational activities. ACUTE CARE COMMITTEE: The Acute Care committee is responsible for the development of regional plans, policies and procedures, protocols as it relates to acute care. The committee has developed the NETRAC regional Stroke Plan (adopted by all NETRAC Hospitals). This committee has also been tasked with working on Cardiac/Stemi and Burns. The Acute Care committee works closely with the EMS/Aeromedical Committee to ensure that the pre-hospital information is incorporated into all acute care plans. EMS/AEROMEDICAL COMMITTEE: The EMS/Aeromedical Committee is responsible for ensuring all NETRAC EMS providers are properly training, and are meeting Performance Improvement Indicators developed by the RAC. System Access Basic 9-1-1 is a regional system providing dedicated trunk lines which allow direct routing of emergency calls. Routing is based on the telephone exchange area, not municipal boundaries. Automatic Number Identification (ANI)is not provided with Basic 9-1-1. There are no basic 9-11 systems within the NETRAC 9-1-1 Emergency Communication System Plan. All systems are enhanced 9-1-1 with different levels of service. Enhanced 9-1-1 Enhanced 9-1-1 is a system which automatically routes emergency calls to a pre-selected answering point based upon geographical location from which the call originated. A 9-1-1 system operates by a caller dialing the digits 9-1-1, then the call is routed to the local telephone company central office or CO; at the CO, the telephone number or ANI is attached to the voice and sent to the Public Safety Answering Point PSAP). With Automatic Location Identification and Selective Routing, the call is sent to the CO and the Computer (9-1 -1 Database) assigns an address to the phone number and routes the call to the designated PSAP. In TSA-F, the primary emergency communication systems for public access is Enhanced 9-1-1. The emergency communication systems were implemented providing citizen’s access to emergency communications to municipalities and counties (incorporated and unincorporated areas) in the TSA-F. ANI is a system capability that enables an automatic display of the seven-digit number of the telephone used to place a 9-1-1 call. This system enables the automatic display of the calling party’s name, address and other information. Alternate Routing (AR) is a selective routing feature which allows 9-1-1 calls to be routed to a designated alternative location if all incoming 9-1-1 lines are busy or the central system (PSAP) closes down for a period of time. Selective Routing (SR) is a telephone system that enables 9-1-1 calls from a defined geographical area to be answered at a pre-designated PSAP. Communications Network The Ark-Tex Council of Governments administers the 9-1-1 Emergency Communications Systems. The communications system includes the following counties: Bowie Cass Morris Titus Red River Franin Lamar Delta Hopkins Miller The contingency plan for the 9-1-1 system includes redundancy of all communications links, with alternate routing capabilities for either system overflow, or evacuation of any of the communications centers. Each center is equipped with an emergency backup power source, and ring down circuits connecting each 9-1-1 answering point. Connectivity is available through the cellular network, as well as radio communications. Strengths Strengths of the current 9-1-1 system include~ Fully enhanced 9-1-1 system which provides ANI information and the appropriate police, fire and EMS agencies that respond to that location. PCs that were provided to the answering point to assist in locating the caller in and AINI level of service areas. All answering points are equipped with voice recording equipment, instant playback capabilities of previous telephone and/or radio conversations. Answering points have access to language line interpretation services, the communication devices for deaf (TDD/TTY), as well as conference call capability. Immediate activation of 9-1-1 with phone calls and break disconnection, even though database information is not current. Weakness Weakness of the current 9-1-1 system includes: 1. Potential average delay for database updates from time of telephone connection (72 hour average). 2. General public awareness and use of the 9-1-1 system. System Access All coin operated telephones in the NETRAC region are programmed to offer free access to 9-11 without depositing coins into coin operated telephones. Communications In TSA-F, LifeNet EMS, Titus Regional Medical Center EMS, and HopkinsCounty Memorial EMS maintain individual emergency medical dispatch systems location in each EMS administrative offices and dispatch for their respective agencies. The City of Paris dispatches EMS calls in LamarCounty. Champion EMS dispatches EMS calls in MorrisCounty and parts of CassCounty. LifeNet EMS dispatches EMS call in Bowie, Red River, and parts of Cass counties. All dispatch personnel in LifeNet, Titus County and Hopkins County are verified by Texas Department of Health as Paramedics and/or Emergency Medical Technicians (EMT) and currently trained in Medical Priority Dispatch for pre-arrival instructions. The EMS dispatch Centers are currently using Dr. Jeff Clawson’s Medical Priority Dispatch PreArrival Instructions. There are high frequency and ultra high frequency radio capabilities throughout TSA-F region. Within the UHF radio band, ten paired sets of frequencies which are reserved for EMS communication have been assigned. Aeromedical communication capabilities are also available. All landing zone communications and assigned to the teams Texas Fire 3 interoperable frequency. Full regional telemetry capability is not available to all EMS agencies. Mobile units can communicate with hospital control console for EMS communications. Outlying areas have access to dispatch operation center through repeater towers. Law Enforcement and fire department frequencies are programmed in all mobile radios. Provisions made for communications with those agencies are for contacting law enforcement and fire agencies in each city or county for coordination during EMS responses. Short Term Goals 1. Develop and implement a standard radio frequency to be used during Disasters and mutual aid assistance within NETRAC. 2. Update Regional Disaster Plan. Long Term Goals 1. Develop and implement a standardized dispatching format to be utilized throughout NETRAC. 2. Insure the delivery of radio communications throughout NETRAC. (No dead spots for communications). Medical Oversight, Medical Direction & Quality Management An essential component of system networking is the presence of strong medical direction (offline/indirect/prospective/retrospective) and available medical control (on-line/direct/immediate) for Pre-hospital EMS service throughout an entire regional trauma system. Texas Trauma Service Area F is both rural and urban. Currently each EMS system and each Hospital have their own Medical Directors which are experienced in emergency medical systems and trauma care, both pre-hospital and hospital. The Physician Advisory and Quality Improvement Committee should be involved in all the critical areas of the Regional Trauma System particularly field triage, pre-hospital and hospital care. The resources of the Physician Advisory and Quality Improvement Committee will also be utilized for trauma prevention, disaster medical care, education and research. Triage, patient delivery decisions, treatment and transfer protocols should be integrated within the system. Field triage is according to the AmericanCollege of Surgeons’ system. Pre-hospital protocols for all levels of EMS personnel are presently in place and revised yearly (refer to Protocol Manual). Any materials introduced in the revisions are taught to the appropriate EMS personnel at multiple sessions, and the material presented should be evaluated by written tests. The Physician Advisory and Quality Improvement Committee should be involved in continuing education and outreach programs. The Committee should also participate in protocol, bypass and diversion decisions and emergency disaster preparedness. On line medical control for EMS personnel utilizes ambulance based radios, regional repeaters and hospital based communications in order to utilize the appropriate resources available for the injured patient. Scene times are evaluated and collected with each run report filed within the respective service. These will be readily available from each entity registry. A standardized data set should be used throughout the region to collect data in Trauma Service Area-F area. These standardized data sets were approved by the Texas Department of Health Services and adopted for usage by all EMS agencies in Trauma Service Area-F counties. TEXEMS Data Points are collected and transmitted to the Texas Department of Health Services. Pre-hospital Triage Criteria Major trauma patients are either categorized as “Critical” or “Urgent” on the Triage Decision Scheme. Refer to attached Triage Decision Scheme; the chart at the bottom of the page identifies the appropriate destination for a patient. It includes recommendations for transfer based on the type of facility which provides initial care. Trauma centers are identified by the type of resources provided by the institution. Triage and transport protocols are based on the resources these hospitals provide. Pediatric patients and patients with burn injuries are addressed specifically in the scheme. Patients with spinal cord injury are identified for appropriate treatment and transfer during the initial assessment. (Vital Signs, determination of the Glasgow Coma Scale and the Revised Trauma Score.) Patients who sustain major injuries may require care at a Level I or Level II trauma center. They may be able to receive initial stabilization at a Level III or Level IV trauma center if the injury occurs in a rural area of the service area. Their clinical needs may include access to rapid transport to a Level I or Level II facility. Demography of the population in the trauma service area is summarized in Appendix C. The trauma service area has six ground EMS services and three air medical services providing emergency care and transport to trauma centers. Appendix D shows the staffing and service level of each of these agencies. Texas Department of Health Services, Bureau of Emergency Services is the regulatory agency for the emergency vehicles, equipment and personnel. The trauma service area utilizes Enhanced 9-1-1 capabilities for accessing the EMS system. Emergency vehicles are dispatched based on the proximity to the injured patient(s). Air medical transport via helicopter or fixed wing is available throughout the region. Ground ambulances follow treatment and transportation guidelines found in the RAC protocol manual. Air Medical Transport treatment and transportation protocols are available through the respective services. All protocols are based on nationally recognized standards. These standards may include Pre-hospital Trauma Life Support (PHTLS), Pediatric Advanced Life Support (PALS), Advanced Cardiac Life Support (ACLS), TNCC and ATLS. Current licensed acute care facilities in the service area are listed in Appendix D. Pre-hospital protocols are reviewed on an annual basis for revisions and refinement. Protocol update classes provide pre-hospital care personnel with information about changes in patient care recommendations. Case reviews should be conducted monthly to analyze and evaluate specific patient care situations and to provide recommendations. Trauma facilities are notified using the field triage decision scheme of incoming patients via radio, cell phone, or telephone from ambulances and aeromedical transportation. The nationally designated radio frequencies are utilized for the transmission of patient information to the hospital (including expected time of arrival at the Emergency Department). Time and distance are extremely important variables to consider when triaging injured patients to local hospitals or trauma centers. Patients who meet the following guidelines and are within twenty (20) minutes transport time to a trauma center should be strongly considered for transport directly to that center. In the rural environment, an injured patient may be at a substantial distance from a trauma center and as such injured patients should ideally be treated initially at the nearest available hospital facility. Patients with major severe injuries should then be secondarily triaged to more distant trauma centers should local resources prove inadequate for continued care. The below criteria are suggestive operating guidelines. The time frame set is a collective guideline set by TSA-F members. Agencies should go by their established protocols set by their medical director. Referral To Trauma Center Initial Procedures Upon encountering any injured patient, pre-hospital personnel must make a rapid assessment of the patient pausing as necessary to treat life threatening situations. This assessment includes: 1. Vital signs and breath sounds 2. Glascow Coma Scale Score / Revised Trauma Score. 3. As thorough a secondary survey as the situation permits Trauma Center Referral Any patient presenting with one or more of the following physiological signs or anatomical injuries in a traumatic setting are considered trauma center candidates: 1. Systolic blood pressure less than 90 with clinical evidence of impending shock 2. Respiratory rate less than 10 or greater than 29, with evidence of trauma 3. Total Glascow Score of 12 or less 4. Penetrating injury to chest, abdomen, head, neck or groin 5. Flail Chest NOTE: Patients in cardiac arrest secondary to hypovolemia due to blunt trauma are NOT trauma center candidates due to uniformly poor outcome regardless of treatment. All patients meeting the above criteria are to be directly triaged from the scene to the nearest tertiary care center or regional resource trauma center (if transport time is less than 20 minutes). This assessment/referral is to be made by the EMT/Paramedic (if transport exceeds 20 minutes, call the closest hospital for consultation and advice). The EMT/Paramedic should employ the treatment regiment as outlined in the Pre-hospital trauma protocol while enroute to the trauma center. To expedite field time, medical control does not need to be established until the unit is enroute to the trauma center. Potential Trauma Center Referral Traumatically injured patients not evidencing absolute criteria for trauma center referral may still be candidates if; on the basis of anatomical sites and/or mechanism of injury, the potential exists for the patient to have sustained critical injuries. These considerations include: 1. 2. 3. Two or more proximal large bone fractures. Combination with burns greater than fifteen percent, face or airway Evidence of high impact a. Falls greater than 12 feet or for pediatric patients falls that are two time the patients height. b. Passenger compartment intrusion 18 inches on patient side of car c. Ejection of patient d. Rollover e. Death of same car occupant f. Pedestrian struck at 20 mile per hour or more When presented with trauma patients not meeting triage criteria, but meeting potential triage criteria, the EMT/Paramedic is to contact their medical control, advise the physician (nearest hospital) of a potential trauma center candidate and relay pertinent information and assessment findings. Realizing that patient conditions may alter the order of a typical report, it is necessary to rapidly and briefly, convey essential information. This includes: 1. Brief description of scenario (auto accident, gunshot, etc.) 2. Patient age, sex, class 3. Vital signs, GCS and assessment findings 4. Other information, including estimated times for transit and/or extrication NOTE: If pre-hospital personnel are unable to directly relay the patient assessment to the physician, they may relay the assessment via other on-scene personnel/dispatcher. If trauma center referral is directed by the physician, transport to the nearest designated trauma center should proceed. Radio contact with the trauma center should be established if possible and maintained throughout the transport. If radio contact with trauma center is not possible, the local command hospital should maintain communication and this hospital should call the trauma center via telephone to relay patient information. Transportation should be expeditious and uninterrupted. For patients not meeting trauma center referral criteria or for patients directed by medical control physician to be transported to the local hospital, the EMT and EMT Paramedic will proceed with BLS and/or ALS treatment as appropriate and transport to the nearest hospital. It must be remembered that transportation of trauma patients is a high priority. On the scene treatment should be limited only to those techniques to stabilize life threatening injuries. Once enroute, further splinting, bandaging, and IV therapy should be initiated and/or continued. Trauma Helicopter Service Multiple factors are involved in determining the most expedient method of transportation to the trauma center. In some cases, the most expedient means may be via a helicopter service. The following are guidelines to be utilized in determining ground vs air transportation. Utilize land transport to nearest regional or regional resource trauma center when: 1. 2. Patient is non-entrapped, or extricated and time from scene to trauma center (by land) is 20 minutes or less. Helicopter is not available to fly Consider air transport to nearest regional or regional resource trauma center when: 1. 2. Patient is entrapped, helicopter can arrive at scene prior to extrication, and scene-totrauma center time can be considerably shortened by utilizing helicopter. Patient is non-entrapped or extricated and land transport time to the nearest trauma center is greater than 20 minutes. In this case, transport to a rendezvous landing zone should be employed. Radio/Communication Failure When communications cannot be established, or once established are interrupted, the decision to triage potential trauma center candidates to a trauma center must be made by the EMIT/Paramedic. The decision of the EMT or paramedic to “by-pass” a local hospital for a trauma center is expected to be made with the patients best interest in mind and in accordance with the trauma referral criteria. Section VI of this policy is to be applied only in bonafide situation of communication failure where multiple attempts to reach medical command have been unsuccessful. Description Of Triage Decision Scheme The Trauma Triage Scheme was a collaboration of the American College of Surgeons and American College of Emergency Physicians guidelines. The Triage Decision Scheme was a collaborative effort of the Bypass/Diversion Committee. This scheme was to serve as a model for TSA-F to incorporate hospitals from Levels I to IV. The Triage Decision Scheme is an algorhythm approach to differentiating patient categories as well as a mechanism for activation of Trauma Team Alerts in Facilities. Patient Categories--The Triage Decision Scheme defines patient categories as critical and urgent. Critical patients meet criteria for instability of hemodynamic and neurologic functions, as well as specific anatomical injuries patterns that place them at a high suspicion for significant risk. Urgent categorized patients are those that are evaluated for evidence of mechanism of injury, high-energy impact and age or disease specific history. Facility Triage Action Plan The facility triage action plan is included within the Triage Decision Scheme to assist facilities in determining where a trauma patient should be transferred. It includes the service that should admit the patients, the Level to be transferred to and stabilization and transport. Guidelines for aeromedical transport are included within this to assist facilities in assuring “the right patient, to the right facility, in the right amount of time.” When in Doubt, Patient should be taken to a Trauma Center Consider Air Transport for all Critical and Urgent Patients Inter-Hospital Transfers All interhospital transfers must comply with current Federal and State regulations, with appropriate transfer memoranda and patient data accompanying the patient. Inpatient to inpatient transfers are accomplished directly from transferring attending to receiving attending physician, and from transferring hospital administration to receiving hospital administration. Trauma patients requiring specialized treatment or specialized care are identified via the Triage Decision Scheme and transfer to an appropriate facility is based on this criteria. Written transfer agreements are available to the major tertiary care facilities within the region. These agreements may be broad in nature or specific, i.e., burn or pediatric. PLAN FOR DESIGNATION OF TRAUMA FACILITIES The purpose of designation is to allow healthcare facilities to determine the level of trauma care they wish to provide. Designation affords healthcare providers a means of recognizing the various levels of service capabilities, within their own institutions and other facilities, thus allowing them to make informed decisions as to the care and treatment of their injured patients. In urban areas, designation may assist with determining patient destination. Designation is not intended to provide a means of determining hospital capabilities by the lay public. Level I The Level I facility is a regional resource trauma center that is a tertiary care facility central to the trauma care system. This facility must have the capability of providing leadership and total care for every aspect of injury, from prevention through rehabilitation. In the Trauma Service Area F, currently we do not have any facilities seeking designation as a Level I trauma facility. Level II The Level II trauma center is a hospital that is also expected to provide initial definitive trauma care, regardless of the severity of injury. Depending on geographic location, patient volume, personnel, and resources, however, the Level II trauma center may not be able to provide the same comprehensive care as a Level I trauma center. Therefore, patients with more complex injuries may have to be transferred to a Level I center. If a Level I center does not exist the Level II center should take on the responsibility for education and system leadership. In the Trauma Service Area F, currently we do not have any facilities seeking designation as a Level II trauma facility. Level III The Level III trauma center serves communities that do not have immediate access to a Level I or II institution. Level III trauma centers can provide prompt assessment, resuscitation, emergency operations, and stabilization and arrange for possible transfer to a facility that can provide definitive trauma care. Currently Titus Regional Medical Center is the only designated Lead Level III trauma center in the Trauma Service Area F (NETRAC) region. Wadley Regional Medical Center – Texarkana, Texas is designated as a Level III Facility in Trauma Service Area F (NETRAC) region Level IV Level IV trauma facilities provide advanced trauma life support prior to patient transfer in remote areas where no higher level of care is not available. Such a facility may or may not have a physician available. Because of geographic isolation, however, the Level IV trauma facility is the de facto primary care provider. If willing to make the commitment to provide optimal care, given its resources, the Level IV trauma facility should be an integral part of the inclusive trauma care system. In Trauma Service Area F (NETRAC), currently we have (four) Level IV trauma centers. Atlanta Memorial Hospital – Atlanta, TX; East Texas Medical Center – Clarksville, TX; Good Shepherd Medical Center – Linden, and Hopkins County Memorial Hospital – Sulphur Springs, TX NETRAC actively encourages and works to facilitate trauma center designation in the region. Facility RAC participation and trauma center designation are encouraged through individual contacts and through prevention programs as well as physician contacts. System Quality Management Program Mission Statement To get the “right patient” to the “right place” in the “right time”. Trauma Service Area F is dedicated to the provision of quality healthcare for the community and the surrounding region. It provides accessible, comprehensive, compassionate, high quality healthcare to all disaster, trauma, and acute patients regardless of age, race, religion, sex, nationality, ability to pay, diagnosis or prognosis, to assure that all patients receive the optimal level of care. The purpose of continuous quality management is to provide ongoing quality assessment and improvement activities designed to objectively and systematically monitor and evaluate the quality of patient care through system analysis, to identify and pursue opportunities to improve patient care, and sustain improvement over time and ultimately to improve survival and reduce morbidity from injury. By participating in the TSA-F RAC, all member organizations embrace the guiding principles for Trauma System QI outlined by the Texas Department of Health. Goals/Objectives The Trauma Service Area F quality management plan is designed to achieve the following goals: 1. To facilitate continuous quality improvement in patient care and services provided, by establishing mechanisms to identify opportunities to improve. This can be achieved by evaluation of clinical processes which may affect patient outcomes and clinical aspects of care or services which are key function activities. 2. To provide a framework for a planned, systematic, ongoing approach for the objective monitoring and evaluation of the quality, appropriateness and effectiveness of trauma patient services provided within the region. 3. To pursue opportunities for improving patient care by evaluating systems and addressing educational issues. Actions will be taken to rectify identified issues. 4. To centralize the flow of information through the organized committee structure, to prevent duplication of effort and to facilitate early awareness of opportunities for improvement. 5. To create an organizational structure which will provide for the coordination, integration and accountability of quality management activities commensurate with established standards. 6. Mandatory participation in the QI process by all member organizations, both hospitals (designated and non-designated facilities) and EMS Systems. 7. To achieve a 5% decrease in trauma morbidity/mortality within TSA-F over the next five years. 8. To identify and recommend corrective action for components of the trauma system which will significantly decrease delays in meeting our mission of getting patients to tertiary care within the “golden hour” for optimum outcomes. 9. Develop a data base through continuous quality improvement activities that will allow identification of trends and/or significant events. 10. Develop and utilize tools for continuous quality improvement review throughout the region, which will serve to identify areas for improvement within the trauma care delivery system. 11. To assist in developing guidelines and standards of care in TSA-F through identification of educational needs via system continuous quality improvement activities. Functional Authority: The final authority and ultimate responsibility for a flexible, comprehensive and integrated quality management plan shall rest with the Northeast Texas Regional Advisory Council. Program Evaluation The effectiveness of the Quality Management Plan will be evaluated on an annual basis and revised as deemed appropriate. Confidentiality All documents generated concerning quality management activities within the region shall be confidential and used only in the exercise of designated functions of the Quality Management Plan. Conflict of Interest No practitioner or other individual involved in quality management activities shall be required to review any case in which they are professionally involved but shall be given the opportunity to participate in the review. Membership Membership of the Quality Improvement Committee is recommended as follows but not limited to: One Representative (Trauma Coordinator, QI representative, or ED Medical Director) from each hospital; EMS Medical Director or EMS Director from each EMS agency; Committee Chair - Quality Improvement The Quality Improvement Committee is involved in all critical areas of the regional trauma system, including field triage, pre-hospital care and hospital care. The resources of the committee will also be used in trauma prevention activities, disaster medical care, and education. Recommendations are made from the Quality Improvement Committee to the Executive Board. System Management Indicators System management indicators should include financial indicators, injury prevention indicators, and outcome indicators. It is essential that the overall financial impact of the trauma care system be analyzed, including the cost of the system and its impact on direct and indirect costs of decreased morbidity and mortality. While specific financial indicators for NETRAC system performance have not been precisely defined at the present time, research into these areas is ongoing. Similarly, injury prevention and control is a critical area where NETRAC can have a major impact on lessening the injury and morbidity in our region. As this area becomes better defined, more specific injury control indicators will be developed. The majority of the system management indicators focus on outcome evaluation. At an absolute minimum, all patients who expire must be identified. Pre-hospital Indicators Pre-hospital care and treatment of trauma patients continually undergoes significant scrutiny. NETRAC will monitor areas such as access to the system, response time, and efficacy of field therapy, triage, transport decisions, scene time, and transport time. EMS Audit Filters 1. Ambulance scene time> 20 minutes (system filter) 2. Trauma patient (GCS 8) leaving the ED or arriving at the ED without a definitive airway (endotracheal tube or surgical airway). Hospital Audit Filters 1. Time of arrival to ED until admission, death, or transfer to another facility. 2. Patient transferred from a higher Level designation to a lower Level designation. System Audit Filters NETRAC serves in an advisory capacity only, with authority to make recommendations and develop standard of care guidelines for TSA-F. Authority for peer review activities rests with the Quality Improvement Committee, and shall be for educational purposes. This authority may be delegated in individual situations to the Executive Board or other standing committee(s) as appropriate. Pre-hospital quality improvement activities are delegated to the EMS Medical Advisory Committee, with mutual reporting and recommendations as appropriate. All peer review activities conducted under the auspices of the NETRAC shall be kept strictly confidential under Texas legal requirements for peer review activities. Authority and responsibility for any disciplinary action rests exclusively with the individual member entities in regard to their employees/medical staff Any liability arising from decisions by individual member entities not to abide by the standard of care developed for TSA-F and approved by the Texas Department of Health shall rest entirely with those member entities. Confidentiality Agreement The purpose of the Northeast Texas Advisory Council Quality Improvement Committee is: 1. To conduct case review and peer review of trauma cases; 2. To make recommendations for improvement in trauma system processes and/or education of trauma providers in the TSA-F region; 3. Through the above processes to establish a standard of trauma care within the region. In order to assure a review that fully addresses all relevant data, including historical information and opportunities for trauma system improvement, full disclosure by all involved parties is required. This information is protected from disclosure by law, especially medical information and potential medical/legal liability issues. Therefore, team reviews are closed to the public and cannot be lawfully discussed unless the public is excluded. In NO CASE should any team member or designee disclose any information regarding team discussion/decisions outside the team, other than pursuant to team confidentiality guidelines? Failure to observe this procedure may violate various confidentiality statutes that contain penalty. Team Operating Procedures Regarding Confidentiality 1. Records acquired by the team to conduct a review are exempt from disclosure under the Open Records Law, Chapter 552 of the Government Code. 2. Data collected and information regarding a review team meeting is confidential. 3. A report or statistical compilation of a review team is a public record subject to the Open Records Law, Chapter 522 of the Government Code IF it does not permit the identification of an individual or HIPAA relevant policies 4. A team member may not disclose any information that is confidential. 5. Information, documents and records of the team are confidential and are not subject to subpoena or discovery and may not be introduced into evidence in any civil or criminal proceedings. 6. Information that would otherwise be available from other sources is immune because they were included in a review team meeting. Confidentiality Agreement The confidentiality agreement pertains to all members and guests of the NETRAC Quality Improvement Committee meeting. It is not considered a breach of confidentiality when: 1.A team member invites a guest, who has information on a case to be reviewed, to a meeting. 2.Information is shared by a team member or guest with the agency that members represents, provided no identifying information is given, in order to change policy, or to carry out prevention issues identified by the team. 3. A team member or guest shares information which that member brought to the meeting, and no mention is made that the case was reviewed at the NETRAC Quality Improvement Committee meeting. It is considered a breach of confidentiality information when: 1. A team member or guest shares identifying information for any reason outside the NETRAC Quality Improvement Committee meeting. 2. Information is shared with any media without the expressed direction of the NETRAC Quality Improvement Committee or the presiding officer. This does not apply to information of which the member had knowledge before the meeting occurred. 3. A team member or guest shares an opinion of anyone present or any facility represented at the NETRAC Quality Improvement Committee meeting outside of such a meeting. 4. A team member or guest expresses an opinion (outside of meeting) which was formed at or derived from a meeting of the NETRAC Quality Improvement Committee regarding a case that was reviewed. Rehabilitation Rehabilitation resource information is included in the hospital needs assessment survey a found in the appendix. Currently HealthSouth Rehabilitation Hospital. Education/Prevention Plan The trauma education/prevention committee has identified three major areas of focus: 1. Education of Pre-hospital personnel. 2. Education of hospital-based personnel. 3. Education of the public, particularly in the area of injury prevention. Pre-hospital Personnel Education Goals All emergency medical services personnel involved in Pre-hospital care of injured patients in Trauma Service Area F will have access to initial and continuing education necessary to developing and maintaining proficiency in trauma care. Immediate Objectives for new Pre-Hospital Agencies 1. Within 90 days, an information packet explaining the purpose of the Regional Advisory Council and the Regional Trauma Care System will be distributed to new Regional EMS providers and personnel. In cooperation with other RAC Committees, an attempt will be made to identify questions which are likely to arise and provide answers to these questions. 2. Within 180 days, a workshop will be conducted to educate new Regional EMS personnel on the scope and function of the Regional Trauma Care System. Intermediate Objectives 1. Initial Education - All basic, intermediate, and advanced EMS students will adhere to the requirements set forth by the Department of Transportation’s National Standard Curriculum, which will include the following: a. Pediatric Trauma b. Adult Trauma c. HazMat Recognition & Identification d. Burn Management e. Aeromedical landing zone safety procedures f. Incident command g. Regional Trauma Care System h. EMS Dispatch Systems i. Regional Communication Systems j. Survival Training k. Street Safety 2. Continuing Education: a. b. All basic, intermediate, and advanced EMS personnel will participate in continuing education which may include PEP, PALS, PHTLS, BTLS, ACLS, and review the Department of Transportation’s National Standard’s Curriculum. A NETRAC Training calendar will be published on an as needed basis. The calendar will be expanded to incorporate information about hospital based training/education, training/education available through all schools and departments at local community colleges, and relevant training/education available through other Regional organizations. Long Range Objectives 1. On an on-going basis, data from the Trauma Registry and the Regional quality improvement process will be used to target specific areas of the initial and continuing education programs for revision and improvement. 2. Intermediate-range objectives for Pre-hospital personnel training will be reviewed and revised on an annual basis. Hospital Personnel Education Goal All hospital personnel involved in care of injured patients in Trauma Service Area F will have access to education necessary to developing and maintaining proficiency in trauma care. Intermediate Objectives 1. Advanced Cardiac Life Support Courses will continue to be offered by the American Heart Association approved ACLS training centers. Every effort will be made to provide courses for personnel from Regional hospitals who must obtain ACLS provider recognition to enable their facility to apply for trauma center designation. 2. Trauma Nurse Core Curriculum will be offered at least twice annually. The Pediatric Emergency Nurse Pediatric Course will be offered at least twice. 3. The ATLS courses will be available for audit by nurses and paramedics. 4. A NETRAC Training calendar will be published on the NETRAC Website. The calendar will be expanded to incorporate information about relevant hospital-based training/education and training/education. 5. To the greatest extent possible, every hospital in the Region will open its staff development activities to personnel from every other hospital and to Pre-hospital personnel. 6. To provide familiarization with Pre-hospital procedures and to promote integration of Pre-hospital and hospital disaster response procedures, representatives of Regional hospitals will be invited and encouraged to participate in the Regional Major EMS Incident Plan review and update sessions. 7. As the Mutual Aid and Disaster Planning Committee and the Education Committee conduct table-top exercises throughout the Region, representatives of local health care facilities will be invited and encouraged to participate to promote integration of Prehospital and hospital disaster response procedures. Long Range Objectives 1. Hospital personnel need education on the roles and capabilities of EMS personnel. To the greatest extent possible, all training/education activities will move toward being: interdisciplinary to encourage personnel to interact, to be aware one another’s capabilities, and to learn to work together more effectively. 2. On an on-going basis, data from the Trauma Registry and the Regional quality improvement process will be made available to hospital staff development coordinators to target specific areas of the initial and continuing education programs for revision and improvement. 3. As the Mutual Aid and Disaster Planning Committee and the Education Committee begin to conduct small and large full-scale exercises of the Regional Major EMS Incident Plan, Regional health care facilities will be invited and encouraged to participate by conducting simultaneous exercises of their in-house disaster plans. 4. Intermediate-range Objectives for hospital personnel training will be reviewed and revised on an annual basis Although the initial focus of trauma system education for hospital personnel will be on individuals who provide care immediately following arrival of the patient in the emergency department, as the system develops, educational efforts will necessarily have to expand to include personnel providing care to trauma patients in the operating room, the intensive care areas, and the rehabilitation units. Physician Education Goal All physicians involved in care of injured patients in TSA-F will have access to education necessary to developing and maintaining proficiency in trauma care. Trauma Prevention & Education Goal Activities which increase public understanding of the trauma care system and which encourage the prevention and reduction of injuries through education of the public and through legislation will be identified and supported, both in Trauma Service Area F and in cooperation with other Trauma Service Areas and the Texas Department of Health, on a statewide basis. Immediate Objectives 1. An expanded Trauma Prevention network of county based coalitions will be established. This network will coordinate safety/injury prevention efforts to avoid duplication of efforts and to target groups with special needs. 2. Involve school systems in the bicycle helmet program through working with PTAs and school administrators to provide bicycle safety education and fit helmets at our costs (or through grants) to students. Intermediate Objectives 1. Trauma prevention programs already being conducted by area organizations will continue. These programs include: a. DWI Awareness. Conducted by NETRAC E.N.C.A.R.E. instructors, this is a grassroots alcohol-awareness slide program developed by emergency nurses in 1982, and presented by professional emergency personnel on a volunteer basis to middle schools, high schools, colleges, parents, and concerned civic groups. The program graphically depicts the dangers associated with drinking and driving, as well as safety-belt noncompliance. b. Think Child Safety programs already being conducted throughout TSA-F region. c. Facilitate increased use of seat belts and child safety seats throughout ~NETRAC region through surveys, public education, car safety checks, and provisions of loaner car seats. 2. The Regional Advisory Council will sponsor a general education program. 3. Bookmarks and book covers with trauma prevention information and referrals to organizations which address specific areas of prevention will be distributed. The possibility of doing media PSA’s should also be evaluated. The objective will be to after the public perception that accidents are chance events that ‘just happen.” 4. A master index of trauma prevention education programs in the Trauma Care System area will be developed. Needs of regional communities for trauma prevention programs will be evaluated as will resources available to meet these needs. 5. Local EMS organizations and hospitals will be provided with resources to promote the incorporation of prevention education materials into the public school curricula in their communities. Local EMS organizations and hospitals will be encouraged and supported in efforts to become American Heart Association CPR Training Centers. The possibility of local EMS organizations and hospitals providing first aid training to the community will also be explored. When a community is served by both an EMS organization and a hospital, cooperative efforts in providing CPR and first aid training to the community will be encouraged. Long-Range Objectives 1. A program will be developed to assist local EMS organizations in conducting home/business safety inspections in their communities. The rationale for this program is similar to the rationale for fire departments preventing fires rather than extinguishing them. This program will have the added benefit of enhancing the public image and visibility of EMS in the Regional communities. 2. In cooperation with the Mutual Aid and Disaster Planning Committee, a program will be developed to involve Regional EMS, fire~-department, and hospital personnel in training Citizen Disaster Response Teams. Based on a concept originally developed by the Los Angeles City Fire Department, Citizen Disaster Response Teams consist of private citizens who have received training in first aid, basic triage, basic fire suppression, light structural rescue, and personal disaster preparedness. During a disaster, when the resources of the local emergency services organizations are stretched to their limits, these citizen responders are able to help their neighbors until professionals arrive. They are also able to act in support of public safety professionals, expanding the community’s resources rapidly. 3. Initial and continuing trauma education programs for Pre-hospital and hospital-based health care personnel will include information on the role of substance abuse as a contributing factor in many types of trauma. The impact of early intervention and counseling with patients in mitigating the consequences of these behaviors will be stressed. 4. Initial and continuing trauma education programs for Pre-hospital and hospital-based health care personnel will stress the importance of active participation in injury prevention programs through: a. role modeling safe practices and health behaviors in the home and work settings. b. counseling activities with patients in the Pre-hospital, hospital, and other healthcare settings. c. participation in political activities to support prevention legislation. d. collaborative participation with other disciplines in injury prevention activities. e. participation in school and community education programs. 5. On an on-going basis, information from the Trauma Registry will be used to evaluate effectiveness of prevention programs, to target areas that need specific programs, and to support legislative efforts. 6. Based on data from the Trauma Registry, the Regional Advisory Council will identify areas of specific concern in which new legislation or revision of existing legislation could reduce or prevent traumatic injuries. Either independently, or in cooperation with the Texas Department of Health and other Regional Advisory Councils, appropriate legislative initiatives will be pursued or supported. Trauma Policy For Inter-Hospital Patient Transfer Goal The following list is to be utilized as guideline for the transfer of trauma patients between a local hospital and a tertiary care center. The list identifies patients at a particular high risk of dying from multiple and severe injuries. Ideally, such patients should be treated at a trauma center where continuing exposure to such problems by team systems may afford a patient an optimum outcome. Such patients should be considered for transfer to a Level I or a Level II whenever possible. 1. Central nervous system a. Central nervous system, head injury: b. Penetrating injury c. Depressed skull fracture d. Open injury e. CSF leak f. Severe coma (GCS less than 10) g. Deterioration in GCS of two points or more h. Lateralizing signs. i. Central nervous system, spinal cord injury Chest a. Wide superior mediastinum b. Major chest wall injury c. Cardiac injury d. Patients who may require protracted ventilation Pelvis a. Pelvic ring disruption with shock b. Pelvic injury with more than five units transfusion c. Evidence of continued pelvic hemorrhage d. Compound (open) pelvic injury e. Pelvic visceral injury Multiple system injury a. Severe injury to two or more body regions Secondary Deterioration (Late sequelae) a. Patient requiring mechanical ventilation b. Sepsis c. Single or, multiple organ system failure (deterioration in CNS, cardiac, pulmonary, hepatic, renal or coagulation systems) d. Osteomyelitis Responsibility for Transfer 1. Shared by referring and receiving physicians. (Referring physician should establish direct communication with the receiving physician. This should not be delegated to hospital clinical or administrative staff). 2. Referring facility responsible for requesting appropriately trained and equipped air or ground transportation resources. 3. Receiving physician should be consulted regarding arrangements and details of the transfer, including transportation. 4. Referring physician is responsible for briefing the transferring EMS crew (Advanced Life Support, hospital staff and/or helicopter crew) on the patient’s condition/vital signs and special care/equipment needed during the transfer. 5. To be done prior to transfer: a. Resuscitate patient and attempt to stabilize patient condition using the following as guidelines: i. Respiratory management 1. Insert an airway or endotracheal tube (if needed) 2. Determine rate and method of oxygen administration 3. Provide suction (if needed) 4. Provide mechanical ventilation (if needed) 5. Insert chest tube (if needed) 6. Insert a nasogastric tube to prevent aspiration ii. Shock Management 1. Control external bleeding 2. Establish patient IV lines using large bore catheters 3. Replace blood volume - or begin such replacement and continue replacement during transfer (consider MAST) iii. Insert Foley catheter and connect to closed system iv. Central nervous system 1. Proper hyperventilation in head injury 2. Mannitol load (if needed) 3. Immobilize all head injuries for possible spinal injuries v. Diagnostic studies 1. Referring and receiving physicians should consult about the appropriate lab studies and x-ray prior to transfer vi. Wound care 1. Clean and dress wounds (Do Not Delay Transport) 2. Tetanus toxoid (when indicated) 3. Antibiotics (when indicated) vii. Fracture management 1. Utilize appropriate splinting and traction 2. Utilize long backboard (when indicated) 6. Management during transport a. Advanced Life Support Level of care necessary b. Continued support of cardio-pulmonary system c. Continued blood volume replacement d. Frequent monitoring of vital signs e. Use of appropriate medications as ordered by physician or as provided by written medical protocol f. Maintain communication with the receiving physician(s) during transfer g. Update and maintain accurate records during the transfer Patient Records and Reports The referring hospital is responsible for sending a complete copy of the patient record or chart from the Emergency Department with appropriate transfer format and copies of the Basic and/or Advance Life Support pre-hospital report form(s) with the patient. Transfer agreements have been in established and in place within TSA-F. Criteria for transfers are utilized and appropriate communication between entities is expected. Facility Diversion Policy Goal To establish a recommended NETRAC wide policy for facility diversion. Aside from the RAC approved diversion policy each hospital is responsible to develop a diversion policy/procedure. Policy Diversion of ambulance traffic will occur only by prearrangement. Facilities may request diversion for 2, 4, or 12 hour periods of time. In order to implement the diversion period, as well as to extend the period, the facility must have a person in authority (house supervisor, administrative representative, or emergency physician) contact the appropriate communications communication systems (9-1-1 communications center, lead facility, etc.) identify him/herself, and request this stand-down status. The lead Trauma facility should not be on diversion unless under severe crisis such as those specified below. All such diversions by these facilities or any facility are subject to review by the Texas Department of Health. The categories of diversions are: Neurosurgical Diversion: All potential neurosurgical patients would be diverted, except prearranged, direct hospital admissions. The neurosurgeon will be notified of such in advance. Critical Care Diversion: If no critical beds are available, all emergency traffic would be diverted to other facilities until beds are available. Full Diversion: All ambulance traffic except direct admissions would be diverted due to emergency and/or operative facilities being overwhelmed with patients. In the event that multiple facilities request simultaneous diversion status, then ambulances would rotate delivery of patients among the city’s facilities until a facility is off diversion status. EMS personnel will be notified of facility status via the communications centers. Diversion status automatically expires at the end of the allotted time period (see above). However, a facility can request to be taken off diversion status in the same manner as the request is made to be placed on diversion. Recommended Guidelines For Diversion Protocol Under the present system each facility will designate a person (ED Physician, Administrative representative, etc.) to be responsible for decisions regarding diversion. 1. Each facility will develop a procedure for their facility to be put on diversion status. These procedures shall be put in writing and presented to the RAC Hospital Care and Management Committee. 2. Reasons for facilities to be put on diversion status: a. Trauma Surgeon is not available *Internal disaster b. Specialty Surgeon (Neuro, Ortho) is not available c. Or Specialty equipment (CT scanner, MIRI is not available) 3. Each facility must have records showing why they were put on diversion. 4. Each facility must have policies and procedures for plans to open up critical-care beds. 5. Each facility must have a Mass Casualty protocol and know how to access other resources within TSA-F region. 7. Level II, III, and IV facilities must notify all EMS communication centers within their service area whenever a facility goes on or off diversion. Facility Bypass Policy Goal Trauma patients who are medically unstable, unconscious, or at high risk of multiple and/or severe injuries will be quickly identified and transported to the appropriate trauma system hospital. Guidelines for facility bypass protocols When developing bypass protocols, each individual entity should consider the capabilities of Pre-hospital firms and facility emergency resources within Trauma Service Area-F. Transport protocols must ensure that patients who meet triage criteria for activation of the regional EMS/trauma system plan will be transported directly to an appropriate trauma facility rather than to the nearest hospital except under the following circumstances: 1. If unable to establish and/or maintain an adequate airway, or in the case of traumatic cardiac arrest, the patient should be taken to the nearest acute care facility for stabilization. 2. A General facility may be appropriate if the expected transport time to the lead trauma facility is excessive. * 3. A Basic facility may be appropriate for immediate evaluation and stabilization if the expected transport time to the lead facility is excessive. * 4. Medical Control may wish to order bypass in any of the above situations as appropriate, such as when a facility is unable to meet hospital resource criteria or when there are patients in need of specialty care. 5. If expected transport time is excessive * or if a lengthy extrication time* is expected, medical control may consider activating air transportation resources if they are available within TSA-F. 6. NOTE: If there should be any question regarding whether or not to bypass a facility, online medical control should be consulted for the final decision. * Exact time should be specified, and will be determined by geography, mode of transportation, patient condition, and other issues as deemed necessary by NETRAC. Air Ambulance Usage Policy Goal To establish the guideline for access to and dispatch of helicopter emergency care services to achieve, effective, efficient and coordinated responses to emergencies involving major trauma victims. Helicopter Capabilities Must be equipped to meet all the standards of an Advanced Life Support Unit (without using ground unit’s equipment). It is recommended that the pilot have experience in EMS flying. Flight crew must have at least two allied medical personnel capable of providing Advance Life Support in Texas (not including ground personnel). Policy Helicopter services may be utilized for the care and transport of major trauma victims according to the Texas Trauma Service-F Guidelines, under the following circumstances. 1. Scenes involving major trauma victims where treatment or transport will be delayed and this delay may impact patient outcome. 2. When helicopter services can respond and deliver the major trauma victims to a trauma center more rapidly than land transportation, i.e., ground transportation time is greater than 25 minutes. In prolonged extrication, call medical control as per trauma protocol. 3. Scenes inaccessible by ground routes. Dispatch All dispatch and coordination of helicopter services shall be accomplished through the responding helicopter communication system. Communication All helicopter communication will be conducted on frequency 155.340, unless otherwise advised by the responding helicopter or the landing zone coordinator. Helicopter Stand-By Helicopter services may be placed on the stand-by mode by police, fire, and EMS personnel. The stand-by mechanism is a means of alerting the helicopter personnel of a possible call and assist in shortening the response time by allowing the pilot to locate the accident and coordinates from appropriate maps. Stand-By Procedure The agency requesting helicopter stand-by should acquire the following information regarding the incident, and contact the local EMS dispatch center (if applicable) or the helicopter service for the request. 1. City 2. Accident location 3. Nearest landing site 4. Requesting units name and unit number 5. Nature of the incident 6. Frequency to communicate 7. Unit name and number that is setting up landing site. Dispatch Procedure EMS personnel on scene may request helicopter services for dispatch. 1. Contact responding unit dispatch center and request a helicopter dispatch. 2. Advise the dispatch of the following information: a. City (if not already given) b. Accident location (if not already given) c. Nearest landing site (if not already given) d. Requesting units name and unit number (if not already given) e. Nature of the incident (if not already given) f. Frequency to communicate (if not already given) g. Unit name and number that will set up landing site (if not already given) h. Number of patients (if not already given) 3. 4. 5. 6. Vital signs (only if available) Level of consciousness (only if available) Specific injuries (only if available) If patients are trapped NOTE: If unable to give vital signs and/or specific injuries, then give a brief explanation why helicopter service is requested (i.e., care overturned, accident with entrapment). An Fire Departments should be dispatched to the designated landing site to prepare landing zone and communicate with the helicopter during landing and takeoff. Safety Rules All personnel working with or around helicopter service will adhere to the following safety rules: 1. Never approach the helicopter until signaled to do so by the flight crew. 2. Always approach the helicopter from the front. 3. NO ONE is permitted near the tail rotor of the helicopter at any time. 4. No smoking or running and avoid placing loose objects around the helicopter. 5. Do not assist the flight crew in opening or closing the helicopter doors. 6. The flight crew will assist, direct the loading and unloading of patients and equipment. 7. Crowds MUST be kept back 150 feet from the helicopter at all times. Charting In the event that helicopter services are used a patient care report will be completed by the helicopter crew and a copy left at the receiving medical facility. Landing Zone A minimum area of 100 X 100 feet, a red light or marker at each corner, clear of wires, trees, brush, bush, large rocks, emergency vehicles, signs and loose objects is required. The pilot will, at all times, be the final authority on determining the appropriateness of the landing site and all matters concerning the aircraft and safety of the aircraft. Criteria For the Consideration Of Air Medical Transport Of Trauma Patients 1. Lengthy extrication of the patient at the scene and the severity of the patient’s injury requires delivery of a critical care team to the scene. 2. Criteria for consideration of Air Medical transport is as allows but not limited to the following: a. the patient was ejected from the vehicle; b. another person in the same vehicle died; c. the patient was a pedestrian struck by a vehicle traveling more than 20 mph; d. the patient was not wearing a safety belt in a car which was overturned; e. the patient was thrown from a motorcycle traveling more than 20 mph; f. the front bumper of the vehicle was displaced to the rear by more than 30 inches, or the front axle was displaced to the rear. 3. The patient fell from a height of greater than 20 feet. 4. The patient experienced a penetrating injury between the mid-thigh and the head. 5. The patient experienced an amputation or near amputation and required timely evaluation for possible reimplantation. 6. The patient experienced a scalping or degloving injury. 7. The patient experienced a severe hemorrhage. Included are those patients with a systolic blood pressure of less than 90 mmHg after initial volume resuscitation and those requiring ongoing blood transfusions to maintain a stable blood pressure. 8. The patient experienced 2nd-3rd degree burns of the skin greater than 15 percent of the body surface, or major burns of the face, hands, feet, perineum, or associated with an airway or inhalation injury. 9. The patient experienced, or had great potential to experience, injury to the spinal cord, spinal column, or neurologic deficit. 10. The patient suffered injuries to the face or neck which might result in an unstable or potentially unstable airway and might require invasive procedures (such as endotracheal or nasotracheal intubation, tracheotomy, cricothyroidotomy) to stabilize the airway. 11. The patient had a score from an objective ranking system for trauma (such as the Trauma Score, Revised Trauma Score, Glasgow Coma Scale, etc.) at the scene or at the referring hospital’s emergency department which indicated a severe injury. 12. The patient is a child less than five years of age with multiple traumatic injuries. 13. The patient is greater than 55 years of age and has multiple traumatic injuries, whether with or without preexisting illness, such as diabetes mellitus, coronary artery disease, chronic obstructive lung disease or chronic renal failure. 14. The patient is an adult with respiratory rate of less than 10 or greater than 30 breaths per minute, or a heart rate of less than 60 or greater than 120 beats per minute End of Day 1 Regional Facility Triage Criteria Policy Goal Purpose The purposes of the Regional Facility Triage Criteria scheme are: a. To categorize patients for determination for facility transport and/or transfer b. To specify facility action plans for transfer of patients c. To include pediatric and burn criteria for patient transport and/or transfer Policy Trauma patients should be placed into one of the following categories by the attending physician based upon the severity of their injuries. Interhospital transfer should then be initiated as appropriate according to the Regional Trauma System’s Facility Triage Decision Scheme. Category I Patients Central Nervous System: Neurological injuries producing prolonged loss of consciousness, posturing, paralysis, or lateralizing sign Spinal injuries with or without neurological deficit Deterioration of the neurological status as indicated by Glascow Coma Scale of <10. Open, penetrating, or depressed skull fracture CSF leak Deterioration of GCS of 2 or more Chest Major chest wall injury Suspected great vessel or cardiac injuries Patients who may require protracted mechanical ventilation Respiratory distress with a rate> 35 or < 10 Penetrating thoracic wound Pelvis Pelvic ring disruption with shock requiring more than five units transfusion ‘-Evidence of continued hemorrhage Compound/open pelvic injury or pelvic visceral injury Blunt abdominal trauma with hypotension or penetrating abdominal wound Multiple System Injury Severe injury to two or more body regions Specialized Problems Second or third degree burns greater than 10% of body surface area or involving airway Baratrauma Uncontrolled hemorrhage Severe maxillofacial or neck injuries Revised Trauma Score of 11 or less Open fractures Second/third trimester of pregnancy Secondary Deterioration Patients requiring mechanical ventilation Sepsis Organ system(s) failure (deterioration in CNS, cardiac, pulmonary, hepatic, renal, or coagulation) Osteomyelitis Category II Patients Patients who are hemodynamically and physiologically stable whose injuries may include: Central Nervous System Transient loss of consciousness Chest Injuries not producing respiratory distress Rib fractures without flail segments Abdomen Blunt trauma not producing hypotension (should also be managed by trauma service) Specialized Problems Closed fractures Soft tissue injuries with controlled hemorrhage Second/third trimester of pregnancy Category III Patients Patients who are continually stable but whose injuries may include: Closed fracture without neurological deficit Normotensive and/or hemodynamically stable Soft tissue injuries of moderate degree EMS Disaster Response Policy Goal To establish a plan for RAC EMS response in case of MCI or disaster Policy Activation Protocol TDH-Tyler will act as central notification site. Once an agency has determined that local resources have been exhausted they should contact the RAC. The requesting agency should in their initial request, at a minimum, describe the task to be performed, number of units needed, supplies needed, how quickly the units will be needed and for how long. TDH-Tyler will then determine the NETRAC EMS agencies to be alerted and request support. Responder will advise the requesting party of an approximate ETA of the unit(s) that may be responding Upon request by TDH-Tyler, each agency will commit one ambulance and crew to respond to the effected area for a minimum of 24 hours. Standard Operating Procedures Unless advised otherwise the following operating procedures will be followed: 1. All units will report to requesting agency’s main base of operation. 2. On arrival the agency’s crew will combine their staff with the requesting agency’s staff with the paramedic staying with his vehicle and practicing under his own set of medical protocols. 3. Each responding agency’s paramedic will provide patient care as set forth by their agency’s medical protocols. 4. All dispatch and radio communications will utilize 155.340. 5. The agency requesting aid will act as the EMS commander and the responding agency crews will report to him/her. 6. The requesting agency will be responsible for providing food, housing, and any additional supplies to responding agency units. Affidavit Acknowledging Participation in RAC NETRAC EMS Response Plan Provider: License #: County of Licensure: Counties of Operations: Level of Service: The RAC NETRAC EMS are collectively referred to as the “Agencies.” The Agencies are desirous of entering into this RAC NETRAC EMS Response Plan whereby the Agencies agree to provide back-up ambulance service to one another under the conditions and pursuant to the terms specified in this Plan. We as the Administrator and Medical Director for agree: To provide ambulance service within requesting agency’s service area when requested to do so by TDH except when agency’s units are unavailable. This RAC NETRAC EMS Response Plan includes, but is not limited to, responding to each agency’s service area when requested to respond to manmade or natural disaster, periods of unusual call volume, sudden unit or equipment mechanical failure, or other extraordinary situations, unless the agency is unable to do so because its personnel and ambulances are providing services elsewhere. To participate in mutual disaster preparedness drills and training sessions, given reasonable notice and availability of personnel, equipment and units. To operate an ambulance that is specifically designed, constructed and equipped to be used for and maintained or operated for the transportation of Patients (such vehicles hereinafter sometimes referred to as an “ambulance”). That agency is in good standing with the State of Texas and has the necessary authority to perform its requirements under these guidelines and to perform the services described herein. To assume all responsibility and liability for medical direction to its own medical service personnel. Each agency assumes no responsibility or liability for payment to each other for services rendered under the terms of this guideline, and the agencies agree to hold each other harmless for payment for any and all services provided to individuals or organizations under the terms of this guideline. That agency participating in the RAC NETRAC EMS Response Plan are independent contractors and not agents, servants, employees, partners or joint ventures of or with each other. That agency shall be responsible for any claims, demands, losses, costs, damages, suits, judgments, penalties, expenses and liabilities of any kind or nature arising directly or indirectly out of or in connection with agency’s activities wherein the agency is negligent. Administrator (Printed Name) Administrator (Signature) Medical Director (Printed Name) Medical Director (Signature) Appendix Appendix A: Map of Texas Trauma Service Areas Appendix B: Northeast Texas Regional Advisory Council “F” - Map Appendix C: List of TSA-F Hospitals HOSPITAL INFORMATION Name: Christus St. Michael Health System Address: 2600 St. Michael Drive Texarkana, TX 75503 Telephone: 903-614-1000 Please list the names of facilities /entities Administrators: CEO: Chris Karam CFO: Thomas Harvey CNO: Nancy Keenan Other Administrator: COO Jason Rounds (Effective 11/7/11) Designation Level: Number of Licensed Beds: Acute Care 312 HGP Representative: Contact Number: Norman Prewitt 903 614-2760 HGP Representative – Alternate: Contact Number: Ray Hervey 903 614-2799 Voting Member: Contact Number: Liberty Bailey 903 614-5558 Alternate Voting Member: Louise Thornell Contact Number: 903 614-2027 Trauma Registrar: Contact Number: Liberty Bailey 903 614-5558 Name: East Texas Medical Center - Clarksville Address: 3000 West Main PO Box 1270 Clarksville, TX 75426 Telephone: 903-427-6400 Please list the names of facilities /entities Administrators: CEO: John Hart CFO: Jim Hines CNO: Rhonda Strate Other Administrator: Designation Level: IV Number of Licensed Beds: 49 HGP Representative: Contact Number: Jeff Nichols 903-427-6487 HGP Representative – Alternate: Contact Number: Rhonda Strate 903-427-6588 Voting Member: Contact Number: Jeff Nichols 903-427-6487 Alternate Voting Member: Rhonda Strate Contact Number: 903-427-6588 Trauma Registrar: Contact Number: Jeff Nichols 903-427-6487 Name: Good Shepherd Medical Center - Linden Address: 404 North Kaufman Linden, TX 75563 Telephone: 903-756-5561 Please list the names of facilities /entities Administrators: CEO: Carla Roadcap CFO: CNO: Other Administrator: Designation Level: IV Number of Licensed Beds: 25 HGP Representative: Contact Number: Bertha Evans 903-756-9859 HGP Representative – Alternate: Contact Number: Karen Stephens 903-756-5561 Voting Member: Contact Number: Bertha Evans 903-756-9859 Alternate Voting Member: Karen Stephens Contact Number: 903-756-5561 Trauma Registrar: Contact Number: Bertha Evans 903-756-9859 Name: HealthSouth Rehab Hospital Address: 515 W 12th Texarkana, TX 75501 Telephone: 903-735-5000 Please list the names of facilities /entities Administrators: CEO: Jerry Jasper CFO:Phylis Buck CNO: Carla Hogde Other Administrator: Designation Level: N/A Number of Licensed Beds: 50 HGP Representative: Contact Number: Scott Reid 903-735-5028 HGP Representative – Alternate: Contact Number: Vornetta Compton 903-735-5057 Voting Member: Contact Number: Scott Reid 903-735-5028 Alternate Voting Member: Contact Number: Vornetta Compton 903-735-5028 Trauma Registrar: Contact Number: Vornetta Compton 903-735-5028 Name: Hopkins County Memorial Hospital Address: 115 Airport Drive Sulphur Springs, TX 75482 Telephone: 903-885-7671 Please list the names of facilities /entities Administrators: CEO: Michael McAndrew CFO: Donna Wallace CNO: Terri Bunch Other Administrator: Designation Level: IV Number of Licensed Beds: 96 HGP Representative: Contact Number: Stuart Cody, RN 903-439-4089 HGP Representative – Alternate: Contact Number: Cheryl Pierce 903-439-2847 Voting Member: Contact Number: Stuart Cody, RN 903-439-4089 Alternate Voting Member: Cheryl Pierce Contact Number: 903-439-2847 Trauma Registrar: Contact Number: Stuart Cody, RN 903-439-4089 Name: Paris Regional Medical Center Address: 820 Clarksville Street Paris, TX 75421 Telephone: 903-737-4521 Please list the names of facilities /entities Administrators: CEO: Bill Porter CFO: Ken Miller CNO: Connie Murchinson Other Administrator: Rita Conder, ACNO Carole Grant, Risk Manager Designation Level: None Number of Licensed Beds: 364 HGP Representative: Contact Number: Scott Conway 903-737-3100 HGP Representative – Alternate: Contact Number: Don Garrison 903-249-6551 Voting Member: Contact Number: Carolyn Kain 903-737-3100 Alternate Voting Member: Byron Prince Contact Number: 903-249-6551 Trauma Registrar: Contact Number: Carolyn Kain 903-737-3100 Name: Titus Regional Medical Center Address: 2001 North Jefferson Ave Mt. Pleasant, TX 75455 Telephone: 903-577-6000 Please list the names of facilities /entities Administrators: CEO: Ron Davis CFO: Duane Shafer CNO: Carol Slider Other Administrator: Designation Level: Lead Level III Number of Licensed Beds: 164 HGP Representative: Contact Number: Mark Mallory 903-577-6362 HGP Representative – Alternate: Contact Number: Robin Gage 903-577-6276 Voting Member: Contact Number: Robin Gage 903-577-6276 Alternate Voting Member: Contact Number: Trauma Registrar: Contact Number: Robin Gage 903-577-6276 Name: Wadley Regional Medical Center Address: 1000 Pine Street Texarkana, TX 75501 Telephone: 903-798-8000 Please list the names of facilities /entities Administrators: CEO: Thomas Gilbert CFO: Steve Winegart CNO: Jeanette Akin Other Administrator: Designation Level: None Number of Licensed Beds: 370 HGP Representative: Contact Number: David Ryther 903-798-8761 HGP Representative – Alternate: Contact Number: LeighAnnScates 903-798-8860 Voting Member: Contact Number: David Ryther 903-798-8761 Alternate Voting Member: LeighAnnScates Contact Number: 903-798-8860 Trauma Registrar: Contact Number: LeighAnnScates 903-798-8860 Appendix D: List of TSA-F EMS Agencies Champion EMS do Arnie Spier Longview, TX 903-291-2504 Emergency Number: E91 1 Number of Vehicles - 4 Type of Service - Hospital - Non Profit Level of Service - MICU County Served – Morris & Cass Square Miles Covered - 1219 Medical Director - Dr. Chris Dunnahoo City of Atlanta Fire Dept. EMS do Robin Betts P.O. Box 669 Atlanta, TX 75551 903-799-4062 Emergency Number ~ E9 11 Number of Vehicles -2/0 backup Type of Service - Public - FD Level of Service - BLS w/ MICU Capability County Served - Cass Square Miles Covered - 1000 Medical Director - Tim O’Kelly, MD City of Paris - EMS do Kent Klinkerman, EMT-P P.O. Box 9037 Paris, TX 75460 903-785-7511 Emergency Number E91 1 Number of Vehicles - 7 Type of Service - Public Level of Service - MICU County Served - Lamar Square Miles Covered - 930 Medical Director – Sharon Malone, MI) Hopkins County EMS do Brent Smith 115 Airport Drive Sulphur Springs, TX 75482 903-885-7671 Emergency Number - E91 1 Number of Vehicles - 7 Type of Service - Public - Hospital District Level of Service - MICU County Served – Hopkins/Delta Square Miles Covered - 1046 Medical Director – Sandra Deniz, M.D. LifeNet do Darren Higgs 6225 St. Michael Drive Texarkana, TX 75503 903-832-8531 Emergency Number E911 Number of Vehicles - 24 Type of Service - Private - Non Profit Level of Service - MICU County Served - Red River, Bowie, Cass, Little River, and Miller Co., ARK. Square Miles Covered - 3232 Medical Director – Matthew Young, MD, FACEP LifeNet EMS Air do Darren Higgs 6225 St. Michael Drive Texarkana, TX 75503 903-832-8531 Emergency Number - 1-800-582-5433 Number of Vehicles - 1 Type of Vehicles - Bell 407 Helicopter Type of Service - Private Non Profit Level of Service - MICU Titus Regional Medical Center EMS do Mark Mallory, RN, LP, MS 2001 N. Jefferson Mt. Pleasant, TX 75455 903-577-6362 Emergency Number E911 Number of Vehicles - 6 Type of Service - Public - Hospital District Level of Service - MICU County Served - Titus Square Miles Covered - 500 Medical Director – Harris Hollingsworth, M.D. Appendix E: List of TSA -F First Responder Organizations Sugarhill VFD do Chief Jerry Clark 60 County Road 3925 Mt. Pleasant, TX 78455 903-563-3100 Emergency Number - E91 1 Number of Vehicles -1 Rescue Level of Service - BLS County Served - Titus Square Miles Covered Authorizing EMS Agency – Titus Regional Medical Center EMS Mount Pleasant Fire Department do Chief Larry McRae 728 E. Ferguson Road Mt. Pleasant, TX 78455 903-575-4144 Emergency Number - E91 1 Number of Vehicles -1 Rescue Truck, Several Additional Trucks Level of Service - BLS County Served - Titus Square Miles Covered Authorizing EMS Agency – Titus Regional Medical Center EMS Talco VFD do Randy Carroll 400 West Broad Talco, TX 78487 903-379-3731 Emergency Number – E911 Number of Vehicles – 1 Rescue Level of Service – BLS County Served - Titus Square Miles Covered – Authorizing EMS Agency – Titus Regional Medical Center - EMS Avery VFD do Chief Gary Tucek P.O. Box 7 Avery,TX 75554 903-684-3361 Emergency Number - E91 1 Number of Vehicles -3 Fire Trucks Level of Service - BLS County Served - Bowie Square Miles Covered - 100 Authorizing EMS Agency - LifeNet EMS Bogata Fire and Rescue do Chief Jerry Hutson P.O. Box 488 Bogata, TX 75417 903-632-5234 Emergency Number - E91 1 Number of Vehicles -4 Fire Trucks, 1 Tanker, Rescue w rescue tools and AED Level of Service - BLS w/AED County Served - Red River Square Miles Covered - 150 Authorizing EMS Agency - LifeNet EMS Boxelder VED do Chief Glen Floyd P.O. Box 109 Annona,TX 75550 903-697-3524 Emergency Number - E91 I Number of Vehicles - 2 Fire Trucks Level of Service - BLS County Served - Red River Square Miles Covered - 100 Authorizing EMS Agency - LifeNet EMS C-S - Redlick/Leary VFD do Chief Greg Liles P.O. Box 1132 Nash, TX 75569 903-831-7900 Emergency Number - E911 Number of Vehicles- I Rescue Level of Service - BLS County Served - Bowie Square Miles Covered - 50 Authorizing EMS Agency - LifeNet EMS Cass County EDS #2 do Chief Chuck Weerts P.O. Box 157 Queen City, TX 75572 903-796-9101 Emergency Number - E911 Number of Vehicles Level of Service - BLS County Served - Cass Square Miles Covered Authorizing EMS Agency - LifeNet EMS Clarksville VFD do FRO Coordinator – Wesley Patrick 300 N. Pecan Clarksville, TX 75426 903-427-3836 Emergency Number - E911 Number of Vehicles Level of Service - BLS County Served –Red River Square Miles Covered Authorizing EMS Agency - LifeNet EMS Cuthand VFD do Chief Phillip Andrews 3705 FM 1487 Bogota, TX 75417 903-249-5668 Emergency Number - E911 Number of Vehicles Level of Service - BLS County Served –Red River Square Miles Covered Authorizing EMS Agency - LifeNet EMS DeKalb VFD do Chief Robby Barrett 110 E. Grizzly St. DeKalb, TX 75559 903-667-3846 Emergency Number - E911 Number of Vehicles Level of Service - BLS County Served - Bowie Square Miles Covered Authorizing EMS Agency - LifeNet EMS Hooks First Responders do Michael Western P.O. Box 37 Hooks, TX 75561 903-547-2250 Emergency Number - E911 Number of Vehicles: 2 – Fire Trucks, 1 Rescue Level of Service - BLS County Served - Bowie Square Miles Covered - 60 Authorizing EMS Agency - LifeNet EMS Liberty-Eylau doChief David Wesselholf 7675 Eylau Loop Rd. Texarkana, TX 75501 903-832-1874 Emergency Number - E91 1 Number of Vehicles - 5 Fire Trucks Level of Service - BLS County Served - Bowie Square Miles Covered - 60 Authorizing EMS Agency - LifeNet Nash VFD doChief Steve Rogers P.O. Box 520 Nash, TX 75569 903-832-7071 Emergency Number - E9 11 Number of Vehicles - 3 Fire Trucks Level of Service - BLS County Served - Bowie Square Miles Covered -30 Authorizing EMS Agency - LifeNet EMS Maud VFD do Roy Beckett P.O. Box 123 Maud, TX 75576 903-585-5813 Emergency Number - E9 11 Number of Vehicles - 1 Rescue Level of Service - BLS County Served – Bowie 4 Square Miles Covered -30 Authorizing EMS Agency - LifeNet EMS Pleasant Grove VFD do Chief Josh Kurtz P.O. Box 4968 Texarkana, TX 75501 903-831-7123 Emergency Number - E911 Number of Vehicles - 2 Level of Service - BLS County Served - Bowie Square Miles Covered - 70 Authorizing EMS Agency - LifeNet EMS Simms VFD doChief Chris Taillon P.O. Box 87 Simms, TX 75574 903-543-2032 Emergency Number - E9 11 Number of Vehicles – 2 Rescue Truck Level of Service - BLS County Served – Bowie 4 Square Miles Covered -80 Authorizing EMS Agency - LifeNet EMS Redwater VFD doChief Merle Luster P.O. Box 316 Redwater, TX 75573 903-671-2688 Emergency Number - E91 I Number of Vehicles -2 Rescue Level of Service - BLS County Served – Bowie 4 Square Miles Covered - 80 Authorizing EMS Agency - LifeNet EMS Wake Village VFD doChief James Guyton 551 Redwater Rd. WakeVillage,TX 75501 903-838-0515 Emergency Number - E91 1 Number of Vehicles - I Rescue, 2 Pumpers Level of Service - BLS County Served - Bowie Square Miles Covered - 40 Authorizing EMS Agency - LifeNet EMS Texarkana Texas Fire Department do Chief Kenneth Copeland 3124 Texas Blvd Texarkana, TX 75501 903-798-3994 Emergency Number E91 I Number of Vehicles Level of Service - BLS County Served - Bowie Square Miles Covered Authorizing EMS Agency - LifeNet EMS Brinker Fire Dept. do Andy Endsley 1415 FM 69 South Sulphur Springs, TX 75482 903-348-8337 Emergency Number - E91 1 Number of Vehicles - 1 Level of Service - BLS County Served - Hopkins Square Miles Covered - 100 Authorizing EMS Agency - Hopkins County EMS Dike VFD do A.G. Sandifeer 1057 CR 3525 Dike, TX 75437 903-945-2061 Emergency Number - E91 1 Number of Vehicles - 1 Level of Service - BLS County Served - Hopkins Square Miles Covered - 100 Authorizing EMS Agency - Hopkins County EMS Hopkins County Fire/Rescue do Carl Nix P.O. Box 288 Sulphur Springs, TX 75482 903-438-4024 Emergency Number - E91 1 Number of Vehicles - 1 Level of Service - BLS County Served - Hopkins Square Miles Covered - 100 Authorizing EMS Agency - Hopkins County EMS Klondike VFD do Janet Currin P.O. Box 489 Klondike, TX 75448 903-517-4057 Emergency Number - E91 1 Number of Vehicles - 1 Level of Service - BLS County Served - Delta Square Miles Covered - 100 Authorizing EMS Agency - Hopkins County EMS North Hopkins VFD do Craig Morgan 111 County RD 4796 Sulphur Springs, TX 75482 Emergency Number - E91 1 Number of Vehicles - 1 Level of Service - BLS County Served - Hopkins Square Miles Covered - 100 Authorizing EMS Agency - Hopkins County EMS Peerless VFD do Jim Rich Box 239 CR 4754 Sulphur Springs, TX 75482 903-945-2267 Emergency Number - E91 1 Number of Vehicles - 1 Level of Service - BLS County Served - Hopkins Square Miles Covered - 100 Authorizing EMS Agency - Hopkins County EMS Pickton-Pine Forest VFD do Mark Sustaire 5308 FM 269 Pickton, TX 75471 903-866-3101 Emergency Number - E91 1 Number of Vehicles - 1 Level of Service - BLS County Served - Hopkins Square Miles Covered - 100 Authorizing EMS Agency - Hopkins County EMS Saltillo FD do Dutch Vallaster 412 CR 3350 Saltillo, TX 75478 903-537-2617 Emergency Number - E91 1 Number of Vehicles - 1 Level of Service - BLS County Served - Hopkins Square Miles Covered - 100 Authorizing EMS Agency - Hopkins County EMS Sulphur Springs FD do Asst. Chief Tim Vaughn 627 Church Street Sulphur Springs, TX 75482 903-885-7548 Emergency Number - E91 1 Number of Vehicles Level of Service - BLS County Served - Hopkins Square Miles Covered - 100 Authorizing EMS Agency - Hopkins County EMS Biardstown VFD do Spencer Eppler 164 CR 13685 Paris, TX 75462 903-783-0404 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Blossom VFD do Sam Cullum P.O. Box 201 Blossom, TX 75416 903-982-5400 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Brookston VFD do Bruce Ary P.O. Box 246 Brookston, TX 75421 903-785-2221 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Campbell Soup E.R.T. do Nancy Whitten 500 N.W. Loop 286 Paris, TX 75460 903-737-2285 Emergency Number Number of Vehicles – 0 Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Chicota VFD do Debbie Lambert P.O. Box 63 Chicota, TX 75425 903-732-3359 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Cunningham VFD do Pat Norwood P.O. Box 36 Cunningham, TX 75434 903-652-2672 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Deport VFD doNanalee Nichols P.O. Box 498 Deport, TX 75435 903-652-5823 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS East Post Oak VFD doVerlon Vaught 1011 CR 44750 Blossom TX 75416 903-982-6463 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Faught VFD do Rick Browning 197 CR 43420 Paris, TX 75462 903-785-9490 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Kimberly-Clark First Responders do Sherry Williams 2466 FM 137 Paris, TX 75460 903-737-5667 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Northwest First Responders do David Edelhauser Rt 1 box 271B Paris, TX 75460 903-785-3003 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS NOVICE VFD do Chris Shoemate 13834 FM 195 Paris, TX 75462 903-784-1148 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Pairs Fire Department do Ronnie Grooms P.O. Box 9037 Paris, TX 75461 903-784-9208 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS PattonvilleVFD do Chet Downs 212 FM 196 Pattonville, TX 75435 903-652-3668 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Powderly VFD do Jack Steed P.O. Box 188 Powderly TX 75473 903-732-4488 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Reno VFD do Leslie Watkins 185 Bybee Street Paris, TX 75462 903-785-4502 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS RoxtonVFD do Paul Helms Box 156 Roxton, TX 75477 903-346-3292 Emergency Number Number of Vehicles – 1 Medical Vehicle Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS Siligan First RespondersVFD do George Rhodes 500 N.W. Loop 286 Paris, TX 75460 903-739-9104 Emergency Number Number of Vehicles – 0 Level of Service - BLS County Served - Lamar Square Miles Covered Authorizing EMS Agency – City of Paris - EMS REGIONAL PLANS REGIONAL MASS FATALITY PLAN FOR TRAUMA SERVICE AREA-F (SERVING BOWIE, CASS, DELTA, HOPKINS, LAMAR, MORRIS, REDRIVER, TITUS, AND MILLER, AR COUNTIES) Northeast Texas Regional Mass Fatality Plan Table of Contents I. Purpose………………………………………………………………………………………….……..4 II. Explanation of Terms……………………………………………………………………….………...4 III. Situations and Assumptions……………………………………………………….……………...….4-5 IV. Mass Fatality Response Plan………………………………………………….………...……………5 V. Evaluation & Assessment……………………………………………………….…….………..…….5-6 VI. Concept of Operations……………………………………………………………....….….…………6 VII. Incident Management Structure…………………………………………….….………………..….7 VIII. Organization and Assignment of Responsibilities…………………………………………...…..…8-10 IX. Resource Management……………………………………………………………..……..………….10 X. Resource Management Flow Chart ..………………………………………….………………….…11 XI. Plan Review………………………………………………………………………….……...………...11 XII. Reference…………………………………………………………………………………….……….12 Regional Mass Fatality Plan I. PURPOSE The purpose of this plan is to identify actions to be taken during the regional response of a mass fatality event. This plan defines a concept of operations for the fulfillment of NIMS compliant organizational roles and responsibilities for a coordinated regional response effort. Primary objectives in mass fatality management include handling human remains in a dignified, respectful, timely, methodical, and safe manner; accomplishing the identification of victims and the certification of cause and manner of death; and advancing to the final disposition of remains according to the wishes of the next of kin, whenever possible. Management of the overall disaster is accomplished using the Incident Command System as codified by the NIMS. The primary functions of command, operations, planning, logistics, and administration/finance are the foundation of a scalable platform that can expand or contract as the scope of the disaster dictates. The Justice of Peace role in an incident is to function in concert with the overall Incident Commander. II. EXPLANATION OF TERMS A. ACRONYMS EOC: Emergency Operations Center FAC: Family Assistance Centers JIC: Joint Information Center JIS: Joint Information System MACC: Multi-Agency Coordination Center MOU: Memorandum of Understanding NIMS: National Incident Management System PPE: Personal Protective Equipment RLO: Regional Liaison Officer NETMOC: Northeast Texas Medical Operations Center TDEM: Texas Division of Emergency Management TER: Texas Electronic Registry B. DEFINITION A mass fatality incident is a term used to describe an incident with multiple deaths that exceeds the routine capability of the Coroner/Medical Examiners and Justices of the Peace. III. SITUATIONS AND ASSUMPTIONS A. Situation The region is vulnerable to natural disasters, hazardous materials incidents, transportation accidents, and acts of terrorism. An occurrence could result in multiple deaths that would require a response that could overwhelm local capabilities. Support from neighboring jurisdictions, counties, state agencies, and federal agencies may be required. B. Assumption IV. Mass fatality disasters have the potential to quickly overwhelm a single jurisdiction’s resources depending on the capacity of the facility and the number of fatalities. Offices that are overwhelmed may seek assistance at region, state and federal levels. Jurisdictions within the Northeast Texas Region (Bowie, Cass, Delta, Hopkins, Lamar, Morris, Red River, Titus, and Miller, AR counties) will provide assistance in the necessary acts of recovery, evacuation, sanitation, temporary storage of remains, notification of next of kin, counseling, and release of remains. MASS FATALITY RESPONSE A. Purpose The purpose of the Mass Fatality Response Plan is to define roles and procedures in preparedness, response, and recovery from mass fatality incidents. The plan will provide proper coordination of incident response activities and establishes methods for sensitive and respectful care in handling human remains. The goal of these guidelines is to enhance the ability of the Northeast Texas Region and its healthcare partners to respond V. to and manage a surge in the number of decedents as a result of any disaster, including an influenza pandemic. While the importance of religious and cultural considerations is recognized, it is not addressed here. These guidelines focus on decedent processing for medical and legal reasons. EVALUATION & ASSESSMENT An initial site visit will be conducted by Emergency Responders/Healthcare facilities to establish a legal; pronouncement of death to determine the following: Number of fatalities involved. VI. Condition of the bodies, i.e. burned, dismembered, etc. Difficulties anticipated in the recovery of the bodies and the types of personnel and equipment needed, i.e. search & rescue, heavy equipment, dog teams, etc. Location of the incident as far as the accessibility and difficulties that may be encountered in transporting bodies from the scene. Formulation of a plan for documentation, body recovery, and transportation. Ascertain the types and numbers of personnel needed to staff the recovery site and morgue operations. Try to anticipate what type of facility would be the most useful for the families of the victims as a Family Support Center. Determine the extent of possible chemical, biological, radiological, or other hazards associated with recovery operations. Determine the need for activation of state and/or federal resources. The request will be initiated by the Incident Commander in coordination with the County EOC/NETMOC. CONCEPT OF OPERATIONS A. General The City/County is responsible for developing and maintaining emergency mass fatality plans within the legal authority delegated to the City/County through the State of Texas. Local and regional resources should be used before requesting additional resources through the State of Texas. The City/County prepares and coordinates procedures, personnel, equipment, supplies, and facilities necessary to conduct activities associated with the mass fatality incident, including: a. Provide and test communications equipment. b. Maintain permanent and temporary morgue capability for bodies (Develop MOU with agencies for refrigerated truck availability; pre-identify temporary internment locations, etc). c. Provide identification and appropriate level PPE for all Health/Medical response personnel. d. Maintain current call lists for supplemental resources of equipment, personnel, or other resources. e. Coordinate with the NETMOC as needed. B. Direction and Control a. All mass fatality management decisions regarding response are made at the local jurisdiction level. b. In accordance with a mission assignment and mutual aid agreements resource support organizations assisting will retain administrative control over their resources and personnel but will be under the operational control of the requesting jurisdictions Incident Commander. c. Management of fatality related operations under the direction of the Justice of Peace is coordinated with the Incident Commander. d. Volunteer groups and individuals may also offer services to assist the Incident Commander or Justice of Peace. Traditionally, this includes forensic pathologists from other regions and members of various funeral associations and dental societies. Funeral service personnel can be a valuable asset to provide, at a minimum, additional staff to serve as “trackers” to monitor custody and processing steps for each set of remains through the morgue process. Likewise, dental personnel, even if they possess no forensic experience, can assist forensic odontologists in a number of areas. For such volunteers who are not already pre-registered, the Incident Commander should ensure that each volunteer acknowledges a liability waiver for workrelated injury and registers in for each period of service. e. Regardless of the source of personnel (local, regional, state, federal, or volunteer) detailed time records must be maintained to document the nature and periods of duty for each and every person assisting during the operation. VII. INCIDENT MANAGEMENT STRUCTURE A. Example: Organization Chart for Decedent Operations in a Mass Fatality VIII. ORGANIZATION AND ASSIGNMENT OF RESPONSIBILITIES A. General The County Judge/City Mayor has the overall authority in the event of a Mass Fatality incident. The County Judge/City Mayor will set the incident objectives, manage the incident operations, oversee the application of resources, and has responsibility over all personnel involved in the response. B. Role of the Justice of the Peace The Justice of the Peace assumes custody of the deceased in order to determine identity, document findings, inventory belongings, tracking the deceased, initiate the death investigation, make notification to family and authorities, determine cause and manner of death, issue death certificates, and coordinate disposition of the remains. Resources normally available to the Justice of the Peace may be outweighed by the volume of deceased remains. The Justice of the Peace may request and obtain additional resources by identifying equipment and personnel assets needed to manage the deceased and channeling those requests through the IC or local Emergency Operations Center. This may include specialized assets to assist with decontamination of deceased who were exposed to chemical, radiological, or biological agents. If the Justice of the Peace requests the assistance of the Medical Examiner’s Office that they routinely use for their non-mass disaster autopsy needs, the Medical Examiner’s Office will assist the Justice of the Peace under his/her authority. C. Task Assignments 1. County/City/Emergency Management: Endorse and support a Mass Fatality Response Plan consistent with the City/County Emergency Operations Plan. Cooperate and coordinate with local, MACC, NETMOC, state, and federal mass fatality resources through all phases of the emergency. Identify sites for temporary internment and develop MOUs. Issue a Disaster Declaration. 2. Justice of the Peace: Establish manner and cause of death. The Justice of the Peace may request assistance from the TER for death certificate processing, as needed. 3. Law Enforcement: Provide security and investigation of the scene, and/or security of transportation as needed. Establish security for short-term morgue operations, and other mass fatality operations. 4. Funeral Home/Mortuary Services: Provide morgue capacity, including equipment, supplies, personnel, and PPE. Maintain a sufficient supply of body bags. Facilitate transportation of bodies. Provide family with funeral services 5. Public Information Officer Prepare statements to the media in coordination with the JIC, utilizing the JIS. 6. Public Health Region 4/5N: Assist the jurisdictional medico-legal authority and law enforcement agencies in the tracking and documenting of human remains and associated personal effects. Reduce the hazard presented by chemically, biologically, or radiologically contaminated human remains (when indicted and possible). Assist in the establishment of temporary morgue facilities. Assist in disaster related mortality surveillance. Assist in the collection of antemortem data in a compassionate and culturally competent fashion from authorized individuals. Assist in assessing the threat of vector-borne diseases. Ensure provision of psychosocial support to the families of the deceased 7. Mental Health Provide immediate crisis intervention. Assess the scope of disaster and provide support for first responders and their families. Provide short and long term support for emotional needs. Ensure provision of psychosocial support to the families of the deceased, in conjunction with public health. 8. Hospital: Assist in providing morgue storage space. Assist in providing medical staff for first aid/medication at the mass fatality operations site. 9. EMS: Assist in recovery and transport to care for injured victims. 10. Fire: Assist with evaluation of the incident site/scene safety. Provide life saving operations. Protect property from fire and hazards. Assist with decontamination of remains. Provide guidance regarding hazards at the incident scene and consultation on decontamination. 11. NETMOC: Assist with coordinating the regional health and medical response activities. Locate additional regional health and medical resources (if needed). Assist with requesting additional health and medical resources from the State (in coordination with the County) IX. RESOURCE MANAGEMENT A. Resource Management is the responsibility of the City/County EOC. The NETMOC is available to assist with health and medical resources (including fatality management) if needed; once the County resources have been depleted. X. RESOURCE MANAGEMENT FLOW CHART Loca Local resources Once local Once City Once County should be used first resources are resources are resources are i.e. hospital depleted; then depleted; contact depleted; contact NETMOC or resources. contact the City. the County. Once County resources are depleted; then the NETMOC/MACC and the County will coordinate to request MACC. additional resources from the State. XI. PLAN REVIEW A. The Regional Mass Fatality Workgroup is responsible for maintaining and updating this plan on an annual basis. Reference A. The following should be addressed by the local jurisdiction: Process for notifying the County Judge. The activation of the Regional Mass Fatality Response Plan in coordination with Incident Command. The process for carrying out field operations according to Texas statutes. Procedures for examinations, identification, and notification of next of kin. The use of Funeral Homes for mortuary services. Coordination of a Family Support Center. The use of the NIMS structure for all emergency operations. Completion of an After-Action Report; as well as critique. Coordination of response and recovery teams. Identify temporary internment locations. Regional Trauma Registry Plan Goal To develop and maintain a trauma reporting and analysis system which will meet requirements of the Texas Department of Health for Trauma Registry, including: Identification of major or severe trauma patients within each health care entity in the region. Identification of the amount of uncompensated trauma care expenditures for each fiscal year by health care entity within the region. Collecting trauma patient data within each health care entity and regional emergency medical service within the region. To improve trauma patient care in the region through analysis of data gathered by the Regional Trauma Registry. Strategies For Accomplishing The Goals: Adopt the American College of Surgeons guidelines for identification of trauma patients. Use the Standard Data Set developed by the Texas Department of Health as a basis for collection of—Pre-hospital and hospital patient data. Coordinate and assist the various health care entities with the region to facilitate data collection and reporting. Survey each health care entity within the region to determine (a) present data collection methods and software programs in use (b) availability and location of computers as possible data entry sites. Simplify the process of data submission while maintaining accuracy and sufficient detail to enable analysis, evaluation, and improvement of trauma care. Maintain confidentiality of all records while assisting other RAC committees in evaluation and modification of patient care procedures for an overall improved patient outcome. NETRAC Stroke Transport Plan This Plan has been developed in accordance with generally accepted Stroke guidelines and procedures for implementation of a comprehensive Emergency Medical Services (EMS) and Stroke System plan. This plan does not establish a legal standard of care, but rather is intended as an aid to decision-making in general patient care scenarios. It is not intended to supersede the physician’s prerogative to order treatment. Goal Recognition of a facility’s capability to treat stroke patients within Trauma Service Area F in the state of Texas . Objectives 1. To develop a system by which facilities within Area F may seek RAC recognition of stroke capabilities. Discussion A facility interested in seeking RAC-Recognition as a Stroke Capable Facility must contact the RAC offices and obtain a letter of participation to include in application for designation. To successfully obtain this RAC recognition, the entity must present page two of this plan along with the application. These documents will be reviewed by the acute care committee for possible recommendations. Facilities must meet all essential criterions as described on the NETRAC Recognized Stroke Capable Facility Essential Criteria Summary Sheet. (See form following this section.) A survey of the document will be completed by the RAC Executive Director and Acute Care Committee. Only after review by the NETRAC Acute Care Committee, will any hospital recognition be given. If said hospital meets requirements, the NETRAC Recognized Stroke Capable Facility Essential Criteria Summary Sheet will be signed. A RAC Recognized Stroke Capable Facility should then apply for certification/designation through Joint Commission or DSHS within a reasonable length of time. Stroke designation expires within two years and the facility must reapply using the process described for re-designation/certification. After meeting Stroke Capable Facility Criteria, the hospital has a six month window in which to obtain designation by either Joint Commission or DSHS. If the hospital fails to obtain this designation the RAC Stroke Capable Facility Designation will expire. RAC Recognized Stroke Capable Facilities will cease to exist when the facility successfully passes a formal designation/certification process from either the Joint Commission or DSHS. CRITERIA DEFINED A. PERSONNEL 1. 24/7 PHYSICIANS 2. STROKE COORDINATOR 3. STROKE MEDICAL DIRECTOR B. PROTOCOLS 1. NIH STROKE SCALE PROTOCOL 2. DYSPHAGIA SCREENING TOOL 3. ED ORDER SET 4. TPA CHECKLIST 5.THROMBOLYTIC THERAPY ADMINISTRATION PROTOCOL 6.CHOLESTEROL SCREENING 7. DVT PROPHYLAXIS 8. REHAB EVALUATION C. EQUIPMENT/LAB 1. 24/7 STAT CT 3. 24/7 LABORATORY D. TRANSFER AGREEMENTS 1. TRANSFER AGREEMENT WITH CERTIFIED/DESIGNATED PRIMARYSTROKECENTER(S) 2. EMS TRANSPORT AGREEMENT(S) E. EDUCATION 1. NIH STROKE SCALE 2. CORE STROKE TEAM 3. PHYSICIANS 4. NURSING PERSONNEL 5. OTHER PERSONNEL 6.CINNCINATI STROKE SCALE 7. PATIENT/FAMILY EDUCATION F. STROKE SYSTEM PI G. PUBLIC AWARENESS ESSENTIAL OR DESIRED E E E E D E E E E E E E E E E E E E E E E E E E MEETS DOES NOT MEET COMMENTS Northeast Texas Regional Advisory Council RECOGNIZED STROKE CAPABLE FACILITY ESSENTIAL CRITERIA SUMMARY SHEET FACILITY: _______________________________ STROKE COORDINATOR/CHAMPION: ESSENTIAL CRITERIA MET ESSENTIAL CRITERIA NOT MET _________________________has met / not met the essential criteria requirements as defined by The Northeast Texas Regional Advisory Council to be recognized as a NETRAC Stroke Capable Facility and to seek further leveled stroke designation. RAC Chair _______________________________ Date Stroke Committee Chair____________________ Date Executive Director ______________________ Date____________________ CRITERIA CLARIFICATION PERSONNEL 24/7 Physician – The facility must have a physician in the ED available 24/7. Stroke Coordinator – The facility must have a designated Stroke Coordinator. The Stroke Coordinator must attend NETRAC Stroke Committee meetings. Stroke Medical Director – The facility must have a designated Medical Director for stroke protocols. It is preferred (but not required) that this physician attend NETRAC Stroke Committee Meetings. PROTOCOLS NIH Stroke Scale Protocol – The facility must have a written protocol utilizing the NIH Stroke Scale. Dysphasia Screening Tool – It is desired that the facility must utilize an accepted Dysphasia screening tool as well as a protocol outlining how patients will be screened for Dysphasia. ED Stroke Order Set- It is essential that the facility have in place an ED Stroke order set to expedite quality care of the patient. tPA Checklist – The facility must have a protocol/ policy and checklist in place for the administration of tPA in their facility. Thrombolytic Therapy Administration Protocol – This criterion refers to a facility having a written protocol for administering thrombolytics if the facility will be administering thrombolytics. Cholesterol Screening – It is essential that the institution should include cholesterol screening in an order set to assure that the patient is accurately assessed. DVT Prophylaxis – It is essential that all patients will be assessed and potentially treated for DVT Prophylaxis either in the Emergency Department or upon admission to the hospital. Rehabilitation Evaluation – It is essential that stroke patients be evaluated for potential Rehab placement in a timely manner. EQUIPMENT/LAB 24/7 STAT CT – This criterion is essential. This criterion refers to the ability to have a CT completed and read within 45 minutes of arrival to ED. 24/7 Laboratory – The facility must have laboratory available 24/7 on-site. These labs include but are not limited to PT, PTT, INR, CBC, and CMP. The turn around time for these tests should be < 45 minutes. TRANSFER AGREEMENTS Agreements with Certified Primary Stroke Centers - The facility should have verbal and/or written transfer agreements with Certified or DesignatedPrimaryStrokeCenters. Agreements with EMS Providers – The facility should have at least one verbal and/or written agreement with an EMS Provider allowing stroke patients to be treated as priority one/emergent. EDUCATION NIH Stroke Scale Education - The facility must mandate that their Emergency Room and ICU nurses along with any Specialty Stroke Unit nurses caring for stroke patients be trained in the NIH Stroke Scale. This training should be completed on an annual basis. Core Stroke Team Education - The facility must have a written protocol outlining core stroke team education. A minimum of 8 hours of CE must be completed annually by all personnel on core stroke team. The core stroke team must be a minimum of the Stroke Medical Director and Stroke Coordinator. Additional members are recommended. Physician Education - The facility must have a written protocol outlining physician education. Other Personnel Stroke Education - It is essential that the entity educate other personnel within the facility regarding the signs and symptoms of stroke. Cincinnati Stroke Scale - It is essential that all EMS providers practicing within NETRAC be trained and their competency documented. Patient/Family Education – The program must address the education needs of the participant, including lifestyle changes that support self management regimens. The program involves participants in making decisions about managing their disease or condition. STROKE SYSTEM PI The facility must have a system to PI stroke cases. Additionally, the facility must participate in NETRAC Stroke Committee. PUBLIC AWARENESS/EDUCATION The facility must participate in regional stroke awareness campaigns and other public education activities regarding stroke as required for designation. NETRAC and the Certified or DesignatedPrimaryStrokeCenters within the area will be assisting Support Stroke Centers in meeting this criterion. Goal Patients will be identified, rapidly and accurately assessed, and based on identification of their actual or suspected onset of symptoms, will be transported to the nearest appropriate NETRAC stroke facility. Purpose In order to ensure the prompt availability of medical resources needed for optimal patient care, each patient will be assessed for the presence of abnormal vital signs, Cincinnati Stroke Scale, and concurrent disease/predisposing factors. System Triage Patients with an onset of stroke symptoms < 4.5 hours should always be taken to the closest PrimaryStrokeCenter within the region. The expection to that is when the ground to ED door time is greater than 30 minutes, making a SupportStrokeCenter the first choice. All unstable patients should be taken to the nearest Emergency Department for stabilization and transfer to an appropriate StrokeCenter. If the stabilization process exceeds the 4.5 hour window for IV tPa, a ComprehensiveStrokeCenter should then be considered. If ground transport time to the nearest StrokeCenter is greater than 30 minutes, consider calling for the helicopter transport to meet you at the closest agreed upon landing zone. Unless immediate stabilization (ABC’s, cardiac arrest, etc.) is required, patients in NETRAC with an onset of stroke symptoms > 4.5 hours and < 8 hours shall be taken to the nearest Stroke Facility. At that time the patient will be assessed by the Stroke physician for possible transfer to a center functioning under guidelines set forth for Comprehensive Stroke Care. Certified/Designated Primary Stroke Center bypass may only occur for the following reasons: 1) Patient preference 2) Physician Preference 3) StrokeCenter is on diversion status on EMSystems. 4) Patients with an onset of stroke symptoms > 8 hours should be taken to the closest acute care facility for treatment. Helicopter Activation Goal NETRAC air transport resources will be appropriately utilized in order to reduce delays in providing optimal stroke care. Decision Criteria 1. Helicopter activation/scene response should be considered when it can reduce transportation time for patients with onset of symptoms <4.5 hours. Should there be any question whether or not to activate air transport resources, on-line medical control should be consulted for the final decision. 2. Patients transported via helicopter should be taken to the nearest CertifiedPrimaryStrokeCenter. Facility Diversion Goal NETRAC stroke facilities will communicate “facility diversion” status promptly and clearly to regional EMS and other facilities through EM Systems in order to ensure that stroke patients are transported to the nearest appropriate stroke facility. System Objectives 1. To ensure that stroke patients will be transported to the nearest appropriate NETRAC stroke facility. 2. To develop system protocols for regional facility and stroke diversion status 3. Regional stroke care problems associated with facility diversion will be assessed through the NETRAC Q A Committee. 4. All facilities and pre-hospital providers will use EM Systems to notify and track resource alert Status. Facility Bypass Goal Suspected stroke patients will be safely and rapidly transported to the nearest appropriate stroke facility within Area F. Decision Criteria Regional transport protocols ensure that patients who meet the triage criteria for activation of the NETRAC Regional Stroke Plan will be transported directly to the nearest appropriate stroke facility rather than to the nearest hospital except under the following circumstances: 1. If unable to establish and/or maintain an adequate airway, the patient should be taken to the nearest acute care facility for stabilization. 2. Medical Control may wish to order bypass in any of the above situations as appropriate, such as when a facility is unable to meet hospital resource criteria or when there are patients in need of specialty care. 3. If expected transport time to the nearest appropriate Stroke Facility is excessive, > 30 minutes, medical control or the EMS crew on scene should consider activating air transportation resources. Facility Triage Criteria Goal The goal of establishing and implementing facility triage criteria in Area F is to ensure that all regional hospitals use standard definitions to classify stroke patients in order to ensure uniform patient reporting and facilitate inter-hospital transfer decisions. Objectives 1. To ensure that each stroke patient is identified, rapidly and accurately assessed, and based on identification and classification of their actual or suspected onset of symptoms, transferred to the nearest appropriate NETRAC stroke facility. 2. To ensure the prompt availability of medical resources needed for optimal patient care at the receiving stroke facility. 3. To develop and implement a system of standardized stroke patient classification definitions. Discussion Patients with an onset of stroke symptoms < 4.5 hours will be taken to the closest Recognized Stroke Facility for treatment and evaluation for interventional care. Patients with an onset of stroke symptoms >4.5 hours and < 8 hours should be taken to the nearest Stroke Facility for evaluation. At that time the patient will be assessed by the Stroke physician for possible transfer to a center functioning under guidelines set forth for Comprehensive Stroke Centers Field and Inter-hospital Transport Plan Identification of Stroke Patients & Stroke Transfers - Stroke patients and their treatment requirements for optimal care are identified in the facility triage criteria and pre-hospital triage criteria. Written transfer agreements are available between all hospital facilities,and hospital facilities in adjacent regions. Stroke patients with special needs may be initially transferred to a Certified/Designated Primary Stroke Center for assessment and treatment. When resources beyond its capability are needed, transfer to another stroke designated facility outside Area F should be expedited, (Comprehensive Center). The Area F initialreceiving hospitals may also choose to transfer patients with special needs or patient preference directly to these facilities, bypassing the Designated Primary Stroke Centers when appropriate. Stroke Patient Transport - Stroke patients in NETRAC are transported according to patient need, availability of air transport resources, and environmental conditions. Ground transport via BLS, ALS, or MICU ground ambulance is available throughout the Region. Air Medical transport is also available in this Region. Stroke Patient Rehabilitation – Rehabilitation and continued care of the stroke patient will be a coordinated effort involving but not limited to the stroke patient, the patient’s family, physicians, stroke facility and referring facility. The goal of this region is to provide the best possible care for a stroke survivor. DISASTER PREPAREDNESS APPENDIX Regional Alternate Care Sites: ALTERNATE CARE SITES - LOCATIONS (per Hospital) ATLANTAMEMORIALHOSPITAL: Name of Facility: Address: Contact Person: and Number: Horne Enterprises, Inc. 101 East Pinecrest Drive Atlanta, TX 75551 Jim Horne, M-F 8a-5p, 903-796-4107 Guard at Ft. Horne: Line 1: 903-796-5206 Radio call sign unit 65 AFD & APD Number of Beds: Estimate of 20, facility has an open floor plan; Level of care to be provided or types of patients that can be taken care of : Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites: Institute Chain of Command, we will access PRN Roster and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. Name of Facility: Address: The Mattie Lanier Richey Center #1 Sportplex Drive Atlanta, TX 75551 Contact Person and Number: Chamber of Commerce: 903-796-3296 Bobby Embry: 903-796-8572 903-824-8572 (cell) Judy Nuckels: 903-796-2192 Jennifer Hodges: 903-796-7836 903-824-2279 (cell) Number of Beds: Estimate of 20, facility has an open floor plan; Level of care to be provided or types of patients that can be taken care of : Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites: Institute Chain of Command, we will access PRN Roster and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. CHRISTUS ST. MICHAEL HEALTH SYSTEM: Name of Facility: On Campus Buildings (Fitness Center, Outpatient Rehab, ImagingCenter, RehabilitationHospital) Address: 2600 St. Michael Drive Texarkana, TX 75503 Contact Person and Number: Jesse Buchanan – 903-614-2391 Number of Beds: 100 Level of care to be provided or types of patients that can be taken care of : Non-critical; Critical patients would shelter in the facility until transport and transfer to a comparable facility Summary of plans for staffing, supply and re-supply of sites: Staff will move with patients. Supplies that can be salvaged from hospital will be moved to ALC, Re-supply will deliver to supply staging area located at ALC. EASTTEXASMEDICALCENTER – CLARKSVILLE: Name of Facility: Address: Clarksville Nursing Center 300 E. Baker Clarksville, TX 75460 Name of Facility: Address: Regency at Red River Rehab and Healthcare 2800 W. Main Clarksville, TX 75460 Contact Person and Number: Ruth Brown Number of Beds: Level of care to be provided or types of patients that can be taken care of : Summary of plans for staffing, supply and re-supply of sites: GOOD SHEPHERD MEDICAL CENTER – LINDEN: Name of Facility: Address: Longview Regional Medical Center Longview, TX Contact Person and Number: Jerri Pendarvis 903-315-2000 Number of Beds: 10-25 or what’s available Level of care to be provided or types of patients that can be taken care of : Acute Care Summary of plans for staffing, supply and re-supply of sites: The Linden facility will provide staff and supplies Name of Facility: Address: Jerry Neel - GSMC-Marshall Center Marshall, TX Contact Person and Number: 903-927-6000 Name of Facility: Address: Atlanta Memorial Hospital 1007 S. William Atlanta, TX 75551 Contact Person and Number: Meagan Beauchamp 903-799-3000 Number of Beds: 10 Level of care to be provided or types of patients that can be taken care of : Acute Care Summary of plans for staffing, supply and re-supply of sites: Linden will bring their own staff and supplies HEALTHSOUTH REHABILITATION HOSPITAL: Name of Facility: Address: WRMC 1000 Pine Street Texarkana, TX 75501 Contact Person and Number: Norman Pruitt – 903-798-8047 or Jeanette Akin @ 903-798-8086 Number of Beds: unknown, estimate 10 to 20 Level of care to be provided or types of patients that can be taken care of : Full nursing care, Healthsouth will send nursing with patients. Summary of plans for staffing, supply and re-supply of sites: Call back list for staffing, standing supply for 96 hr sustainability, resupply using MOU’s with vendors for food, medical supplies, water, fuel and laundry Name of Facility: Address: Contact Person and Number: 4-States Fair Ground 3700 E. 50th Street Texarkana, AR 71854 870-773-2941 Number of Beds: unknown, open cot layout Level of care to be provided or types of patients that can be taken care of : minor wounds, bed and meals (basic sheltering) HOPKINS COUNTY MEMORIAL HOSPITAL: Name of Facility: Address: Wesley United Methodist Church Sulphur Springs, TX 75482 Contact Person And Number: Jay Sanders Number of Beds: 200 Level of care to be provided or types of patients that can be taken care of : Minor Care, mostly sheltering Summary of plans for staffing, supply and re-supply of sites: Will utilize our emergency call back list PARIS REGIONAL MEDICAL CENTER: Name of Facility: Address: Love Civic Center 2025 S. Collegiate Dr. Paris, TX75460 Contact Person and Number: 903-739-9912 Number of Beds: Estimate of 150, facility has an open floor plan; Level of care to be provided or types of patients that can be taken care of :Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites: Chain of Command, as instituted in our emergency Plan and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. Name of Facility: Address: Paris Junior College Gymnasium 2400 Clarksville St. Paris, TX75460 Contact Person and Number: 903-782-0218 Number of Beds: Estimate of 50, facility has an open floor plan; Level of care to be provided or types of patients that can be taken care of : Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites:Chain of Command, as instituted in our emergency Plan and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. Name of Facility: Address: Paris High School Gymnasium 2400 Jefferson Rd. Paris, TX75460 Contact Person and Number: Number of Beds: 903-737-7473 Estimate of 30, facility has an open floor plan; Level of care to be provided or types of patients that can be taken care of : Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites: Chain of Command, as instituted in our emergency Plan and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. Name of Facility: Address: North Lamar High School Gymnasium 3201 Lewis Ln. Paris, TX75460 Contact Person and Number: 903-737-2000 Number of Beds: Estimate of 50, facility has an open floor plan Level of care to be provided or types of patients that can be taken care of :Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites:Chain of Command, as instituted in our emergency Plan and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. TITUSREGIONALMEDICALCENTER: Name of Facility: Address: Mount Pleasant Convention Center 1800 N. Jefferson Mt. Pleasant, TX 75455 Contact Person and Number: Bill Luck - 903-575-4190 Number of Beds: 120 Level of care to be provided or types of patients that can be taken care of : Non-acute patients. Limited bathrooms and no on site shower facilities. Summary of plans for staffing, supply and re-supply of sites: Hospital to supply if needed for hospital patients. Local emergency management has cots and blankets. WADLEY REGIONAL MEDICAL CENTER: Name of Facility: Address: Southwest Center 3222 W. 7th Street Texarkana, TX75501 Contact Person: and Number: Robert McDonald – 903-223-3298 Number of Beds: Level of care to be provided or types of patients that can be taken care of : Summary of plans for staffing, supply and re-supply of sites: *****See Attachment Regional Utilities: FY 2012 - 2013 NETRAC REGIONAL UTILITIES AtlantaMemorialHospital Utilities Atlanta Fire/EMS Utilities CASSCOUNTY Water Utilities: Name: Address: Phone Number: Atlanta Utilities P.O. Box 669, 315 N Buckner, Atlanta, Texas75551 903-796-7153, after hours 903-796-7973 Electric/Power Utilities: Name: Address: Phone Number: American Electric Power P.O. Box 24422, Canton, OH44701 1-800-216-3523 Gas Utilities: Name: Address: Phone Number: Center Point P.O. Box 2628, Houston, Tx77252 1-800-752-8036 Phone Utilities: ********NEW CHANGE FROM PREVIOUS REPORT******** Name: Airespring, Total Telecom Solutions of Louisiana Address: P.O. Box 53342, Shreveport, LA71135 Phone: 1-888-389-2899 Food Services: Name: Address: Phone Number: Fax: Contact: Ben. E. Keith Foods 10610 Metric Drive, Suite 191, Dallas, Tx75243 214-388-5411 or 1-800-588-5411 903-223-7955 Brian Strand, cell 903-278-2337 Medical Supplies Name: Address: Phone: Contact: Cardinal 3080 W Interstate 29, Dallas, Tx75052 1-800-964-5227 Linda Ingram, 1-800-724-1111 option 3 Christus St. Michael Health Care System - Hospital Utilities BOWIECOUNTY WATER UTILITIES: Name: Texarkana Water Utilities Address: 801 Wood Street Texarkana, TX75501 Phone Number: 903 798-3800 Contact Person: Patrick Reed ELECTRIC/POWER UTILITIES: Name: AEP Address: 3708 West 7th Texarkana, TX75503 Phone Number: 903 748-2110 Contact Person: John Jones GAS UTILITIES: Name: Centerpoint Energy Address: PO Box 520 Texarkana, TX75504 Phone Number: 870 779-6338 Contact Person: Diane Englekiss TELEPHONE UTILITIES: Name: Windstream Address: 507 Olive St. Texarkana, AR71854 Phone Number: 903 748-5588 Contact Person: Greg Einsberg FOOD SERVICES: Name: Aramark Address: 2600 St. Michael Drive Texarkana, TX75503 Phone Number: 903 614-2093 Contact Person: Malcolm McInnis MEDICAL SUPPLIES: Name: CHRISTUS St. Michael, Material Management Address: 2600 St. Michael Drive Texarkana, TX75503 Phone Number: 903 614-2830 Contact Person: John Morkavich, Director of Material Management East Texas Medical Center - Clarksville - Hospital Utilities REDRIVERCOUNTY WATER UTILITIES: Name: City of Clarksville Address: 800 West Main Street Clarksville, TX75426 Phone Number: 903-427-3834 Contact Person: Penny Hobbs ELECTRIC/POWER UTILITIES: Name: Direct Energy Address: 1001 Liberty Pittsburg, PA15222 Phone Number: 1-888-925-9115 Contact Person: GAS UTILITIES: Name: None Address: Phone Number: Contact Person: TELEPHONE UTILITIES: Name: Address: Windstream Phone Number: 1-800-792-6206 Contact Person: FOOD SERVICES: Name: US Foodservice Address: 950 South Shiloh Rd Garland, TX 75042 Phone Number: 1-800-527-1691 Contact Person: Pete Beswick MEDICAL SUPPLIES: Name: Owens & Minor Address: 1434 Patton Place Carrollton, TX75007 Phone Number: 1-800-726-5599 Contact Person: Bruce Whitley GoodShepherdMedicalCenter - Linden- Hospital Utilities CASSCOUNTY WATER UTILITIES: Name: City of Linden Address: 104 South Main Street Linden, TX 75563 Phone Number: 903-756-7502 Contact Person: Gary Wells (903) 235-2109 ELECTRIC/POWER UTILITIES: Name: AEP Swepco Address: PO Box 24404 Canton, OH 44701-4401 Phone Number: 1-888-216-3523 Contact Person: Gary Wells (903) 235-2109 GAS UTILITIES: Name: Centerpoint Energy Address: PO Box 4981 Houston, TX 77210-4981 Phone Number: 1-800-259-5544 Contact Person: Gary Wells (903) 235-2109 TELEPHONE UTILITIES: Name: Windstream Address: 507 Olive Street Texarkana, TX75501 Phone Number: 1-866-225-8356 Contact Person: Gary Wells (903) 235-2109 FOOD SERVICES: Name: US Food Address: Dallas, TX Phone Number: Doug – 903-244-5215 Contact Person: Jessica Moore - 940-597-7604 (cell); 903-756-5561 MEDICAL SUPPLIES: Name: GoodShepherdMedicalCenter - Longview Address: 700 East Marshall Ave. Longview, TX75601 Phone Number: 903-315-2000 Contact Person: Melanie Nipper HealthSouthRehabHospital- Hospital Utilities BOWIECOUNTY WATER UTILITIES: Name: TEXARKANA WATER UTILITIES Address: 801 WOOD ST. TEXARKANA, TX 75501 Phone Number: 903-798-3800, ENG. – 903-798-3829 Contact Person: ELECTRIC/POWER UTILITIES: Name: SWEPCO __________ Address: Phone Number: Contact Person: 1-888-216-3523, 877-237-2886______ GAS UTILITIES: Name: CENTERPOINT ENERGY Address: Phone Number: 1-800-259-7552, 1-800-259-5544 Contact Person: TELEPHONE UTILITIES: Name: WINDSTREAM Address: 2315 RICHMOND RD STE 101 TEXARKANA, TX. 75501 Phone Number: 1-800-843-9214 Contact Person: FOOD SERVICES: Name: SYSCO FOOD SERVICES (EAST TEXAS, LLC) Address: 4577 ESTES PARKWAY LONGVIEW, TEXAS., 75603 Phone Number: Contact Person: 903-252-6100 MEDICAL SUPPLIES: Name: CARDINAL HEALTH Address: 7000 CADINAL PLACE DUBLIN, OH 43017 Phone Number: 1-800-567-5831 Contact Person: HopkinsCountyMemorialHospital- Hospital Utilities HopkinsCountyEMS Utilities DELTA-HOPKINSCOUNTY WATER UTILITIES: Name: City of Sulphur Springs Address: Sulphur Springs, TX Phone Number: 903-885-7541 Contact Person: ELECTRIC/POWER UTILITIES: Name: OnCore; Texas Power Consult Address: Phone Number: 903-439-4233; 1-888-313-6862; 1-800-223-2133 Contact Person: Victor Davis - 903-533-9953 GAS UTILITIES: Name: Atmos Energy Address: Phone Number: 1-800-817-8090 Contact Person: TELEPHONE UTILITIES: Name: Address: Phone Number: Contact Person: FOOD SERVICES: Name: Address: Phone Number: Contact Person: MEDICAL SUPPLIES: Name: Beacon Medical Address: Phone Number: Contact Person : 1-817-366-1134 Paris Regional Medical Center - Hospital Utilities LAMARCOUNTY WATER UTILITIES: Name: City of Paris Address: 50 West Hickory St. Paris, TX75460 Phone Number: 903-784-9277 or 903-249-5160 Contact Person: Doug Harris ELECTRIC/POWER UTILITIES: Name: Oncor Address: Phone Number: 1-888-313-3747 Contact Person : GAS UTILITIES: Name: Atmos Address: Phone Number : Contact Person: 1-866-322-8667 TELEPHONE UTILITIES: Name: AT&T Address: Phone Number: 1-800-442-9950 (Repairs); 1-800-286-8313 (Circuits) Contact Person: FOOD SERVICES: Name: SYSCO FOOD SERVICES (EAST TEXAS, LLC) Address: 4577 ESTES PARKWAY LONGVIEW, TEXAS., 75603 Phone Number: 903-252-6100 Contact Person: Michael Dewitt MEDICAL SUPPLIES: Name: Owens & Minor Address: 1434 Patton Place Carrollton, TX75007 Phone Number: 972-242-5599 Contact Person: Craig Dabbs TitusRegionalMedicalCenter- Hospital Utilities TitusRegionalMedicalCenter- EMS Utilities TITUSCOUNTY WATER UTILITIES: Name: City of Mt. Pleasant Address: 501 North Madison Ave Mt. Pleasant, TX 75455-3650 Phone Number: 903-575-4000 after hours – 903-575-4132 Contact Person: ELECTRIC/POWER UTILITIES: Name: Swepco Address: PO Box 24422 Canton, OH 44701-4422 Phone Number: 903-748-2110 Contact Person: John James GAS UTILITIES: Name: Centerpoint Energy Address: PO Box 3391 Lawton, OK73502 Phone Number: 580-591-3356 Contact Person: Sam Helton TELEPHONE UTILITIES: Name: AT&T Address: Phone Number: 888-944-0447 Contact Person: FOOD SERVICES: Name: Sysco East Texas Address: 4577 Estes Pkwy Longivew, TX 75603 Phone Number: 903-285-7842; 1-866-959-5184 Contact Person: Mike Pewitt MEDICAL SUPPLIES: Name: Cardinal Health Address: 601 Windsor Pl Tyler, TX 75701 Phone Number: 903-303-8417 (cell); 1-800-964-5227 Contact Person: Kevin Thomas WadleyRegionalMedicalCenter- Hospital Utilities BOWIECOUNTY WATER UTILITIES: Name: TEXARKANA WATER UTILITIES Address: 801 WOOD ST. TEXARKANA, TX 75501 Phone Number: 903-798-3800, ENG. – 903-798-3829 Contact Person : Bill Darby (903) 278-0562 ELECTRIC/POWER UTILITIES: Name: AEP SWEPCO __________ Address: West 7th Street Phone Number: 1-888-216-3523, 877-237-2886______ Contact Person: J R Jones@aep.com (903)748-2110 GAS UTILITIES: Name: CENTERPOINT ENERGY Address: Phone Number: 1-800-259-7552, 1-800-259-5544 Contact Person: Jonathan Dothage (314) 991-7381 TELEPHONE UTILITIES: Name: WINDSTREAM Address: 2315 RICHMOND RD STE 101 TEXARKANA, TX. 75501 Phone Number: 1-800-843-9214; 903-223-4688 Contact Person: FOOD SERVICES: Name: SYSCO FOOD SERVICES Address: 4577 ESTES PARKWAY LONGVIEW, TEXAS., 75603 Phone Number: 903-252-6100 Contact Person: MEDICAL SUPPLIES: Name: Owens and Minor Address: 550 Lakeside ParkwayBldg 200 Flower Mound, TX 75028 Phone Number: 1-800-726-5599 Contact Person: Betty – 972-538-6507 Champion EMS- Utilities MORRISCOUNTY WATER UTILITIES: Name: City of Daingerfield Address: 108 Coffey Daingerfield, TX 75638 Phone Number: 903-645-5511 Contact Person: Name: City of Lone Star Address: PO Box 0218 Lone Star, TX 75668 Phone Number: 903-656-2311 Contact Person: ELECTRIC/POWER UTILITIES: Name: Swepco Address: PO Box 24401 Canton, OH44701-4401 Phone Number: 1-888-216-3523 Contact Person: Name: Bowie Cass Electric Address: PO Box 47 Douglassville, TX75560 Phone Number: Contact Person: 1-800-794-2919 GAS UTILITIES: Name: CenterPoint Energy Address: PO Box 2628 Houston, TX77252-2628 Phone Number: 1-800-259-5544 Contact Person: TELEPHONE UTILITIES: Name: Windstream Address: 1720 Galleria Blvd. Charlotte, NC 28270 Phone Number: 903-645-5978 Contact Person : FOOD SERVICES: Name: Address: Phone Number: Contact Person : MEDICAL SUPPLIES: Name: Boundtree Medical Address: 23537 Network Place Chicago, IL60673 Phone Number: 1-800-533-0523 Contact Person: Elizabeth Woodyard Champion EMS- Utilities CASSCOUNTY WATER UTILITIES: Name: City of Linden Address: PO Box 419 Linden, TX75563 Phone Number: 903-756-7502 Contact Person: ELECTRIC/POWER UTILITIES: Name: Swepco Address: PO Box 24401 Canton, OH44701-4401 Phone Number: Contact Person: 1-888-216-3523 GAS UTILITIES: Name: CenterPoint Energy Address: PO Box 2628 Houston, TX77252-2628 Phone Number: 1-800-259-5544 Contact Person: TELEPHONE UTILITIES: Name: Windstream Address: 1720 Galleria Blvd. Charlotte, NC 28270 Phone Number: 903-645-5978 Contact Person: FOOD SERVICES: Name: Address: Phone Number: Contact Person: MEDICAL SUPPLIES: Name: Boundtree Medical Address: 23537 Network Place Chicago, IL60673 Phone Number: 1-800-533-0523 Contact Person: Elizabeth Woodyard ` City of Paris - EMS- Utilities LAMARCOUNTY WATER UTILITIES: Name: Address: Phone Number: Contact Person: ELECTRIC/POWER UTILITIES: Name: Address: Phone Number: Contact Person: GAS UTILITIES: Name: Address: Phone Number: Contact Person: TELEPHONE UTILITIES: Name: Address: Phone Number: Contact Person: FOOD SERVICES: Name: Address: Phone Number: Contact Person: MEDICAL SUPPLIES: Name: Address: Phone Number: Contact Person: LifeNetEMS – Utilities BOWIECOUNTY WATER UTILITIES: Name: TEXARKANA WATER UTILITIES Address: 801 WOOD ST. TEXARKANA, TX 75501 Phone Number: 903-798-3800, ENG. – 903-798-3829 Contact Person: Bill Darby (903) 278-0562 ELECTRIC/POWER UTILITIES: Name: Bowie Cass Electric Co. Address: HWY 8 N – PO Box 47 __________ Douglasville, TX75560 Phone Number: 903-846-2311 ______ Contact Person : GAS UTILITIES: Name: CENTERPOINT ENERGY Address: PO Box 2628 Houston, TX77252 Phone Number: Contact Person: 1-888-876-5786 TELEPHONE UTILITIES: Name: WINDSTREAM Address: 507 Olive Street TEXARKANA, TX. 75501 Phone Number: 903-792-6226; 1-877-520-5210 Contact Person: Tim Day – 903-791-3765 FOOD SERVICES: Name: Address: Phone Number: Contact Person: MEDICAL SUPPLIES: Name: Boundtree Medical Address: 23537 Network Place Chicago, IL 60673 Phone Number: 1-817-658-4168; 1-800-533-0523 x 5141 Contact Person: Gerald Ramirez Regional Shelters: NETRAC REGIONAL SHELTERS AND ALTERNATE CARE SITES - LOCATIONS (per Hospital) ATLANTAMEMORIALHOSPITAL: Name of Facility: Address: Horne Enterprises, Inc. 101 East Pinecrest Drive Atlanta, TX75551 Contact Person: Jim Horne, M-F 8a-5p, 903-796-4107 and Number: Guard at Ft.Horne: Line 1: 903-796-5206 Radio call sign unit 65 AFD & APD Number of Beds: Estimate of 20, facility has an open floor plan; Level of care to be provided or types of patients that can be taken care of : Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites: Institute Chain of Command, we will access PRN Roster and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. Name of Facility: Address: The Mattie Lanier Richey Center #1 Sportplex Drive Atlanta, TX75551 Contact Person and Number: Chamber of Commerce: 903-796-3296 Bobby Embry: 903-796-8572 903-824-8572 (cell) Judy Nuckels: 903-796-2192 Jennifer Hodges: 903-796-7836 903-824-2279 (cell) Number of Beds: Estimate of 20, facility has an open floor plan; Level of care to be provided or types of patients that can be taken care of : Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites: Institute Chain of Command, we will access PRN Roster and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. CHRISTUS ST. MICHAEL HEALTH SYSTEM: Name of Facility: On Campus Buildings (Fitness Center, Outpatient Rehab, ImagingCenter, RehabilitationHospital) Address: 2600 St. Michael Drive Texarkana, TX75503 Contact Person and Number: Jesse Buchanan – 903-614-2391 Number of Beds: 100 Level of care to be provided or types of patients that can be taken care of : Non-critical; Critical patients would shelter in the facility until transport and transfer to a comparable facility Summary of plans for staffing, supply and re-supply of sites: Staff will move with patients. Supplies that can be salvaged from hospital will be moved to ALC, Re-supply will deliver to supply staging area located at ALC. EASTTEXASMEDICALCENTER – CLARKSVILLE: Name of Facility: Address: Clarksville Nursing Center 300 E. Baker Clarksville, TX75460 Name of Facility: Address: Regency at Red River Rehab and Healthcare 2800 W. Main Clarksville, TX75460 Contact Person and Number: Ruth Brown Number of Beds: Level of care to be provided or types of patients that can be taken care of : Summary of plans for staffing, supply and re-supply of sites: GOODSHEPHERDMEDICALCENTER – LINDEN: Name of Facility: Address: Longview Regional Medical Center Longview, TX Contact Person and Number: Jerri Pendarvis 903-315-2000 Number of Beds: 10-25 or what’s available Level of care to be provided or types of patients that can be taken care of : Acute Care Summary of plans for staffing, supply and re-supply of sites: The Linden facility will provide staff and supplies Name of Facility: Address: Jerry Neel - GSMC-Marshall Center Marshall, TX Contact Person and Number: 903-927-6000 Name of Facility: Address: Atlanta Memorial Hospital 1007 S. William Atlanta, TX75551 Contact Person and Number: Meagan Beauchamp 903-799-3000 Number of Beds: 10 Level of care to be provided or types of patients that can be taken care of : Acute Care Summary of plans for staffing, supply and re-supply of sites: Linden will bring their own staff and supplies HEALTHSOUTH REHABILITATION HOSPITAL: Name of Facility: Address: WRMC 1000 Pine Street Texarkana, TX75501 Contact Person and Number: Norman Pruitt – 903-798-8047 or Jeanette Akin @ 903-798-8086 Number of Beds: unknown, estimate 10 to 20 Level of care to be provided or types of patients that can be taken care of : Full nursing care, Healthsouth will send nursing with patients. Summary of plans for staffing, supply and re-supply of sites: Call back list for staffing, standing supply for 96 hr sustainability, resupply using MOU’s with vendors for food, medical supplies, water, fuel and laundry Name of Facility: Address: Contact Person and Number: Number of Beds: 4-States Fair Ground 3700 E. 50th Street Texarkana, AR71854 870-773-2941 unknown, open cot layout Level of care to be provided or types of patients that can be taken care of : minor wounds, bed and meals (basic sheltering) HOPKINS COUNTY MEMORIAL HOSPITAL: Name of Facility: Address: Wesley United Methodist Church Sulphur Springs, TX 75482 Contact Person And Number: Jay Sanders Number of Beds: 200 Level of care to be provided or types of patients that can be taken care of : Minor Care, mostly sheltering Summary of plans for staffing, supply and re-supply of sites: Will utilize our emergency call back list PARIS REGIONAL MEDICAL CENTER: Name of Facility: Address: Love Civic Center 2025 S. Collegiate Dr. Paris, TX75460 Contact Person and Number: 903-739-9912 Number of Beds: Estimate of 150, facility has an open floor plan; Level of care to be provided or types of patients that can be taken care of :Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites: Chain of Command, as instituted in our emergency Plan and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. Name of Facility: Address: Paris Junior College Gymnasium 2400 Clarksville St. Paris, TX 75460 Contact Person and Number: 903-782-0218 Number of Beds: Estimate of 50, facility has an open floor plan; Level of care to be provided or types of patients that can be taken care of : Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites:Chain of Command, as instituted in our emergency Plan and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. Name of Facility: Address: Paris High School Gymnasium 2400 Jefferson Rd. Paris, TX75460 Contact Person and Number: Number of Beds: 903-737-7473 Estimate of 30, facility has an open floor plan; Level of care to be provided or types of patients that can be taken care of : Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites: Chain of Command, as instituted in our emergency Plan and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. Name of Facility: Address: North Lamar High School Gymnasium 3201 Lewis Ln. Paris, TX75460 Contact Person and Number: 903-737-2000 Number of Beds: Estimate of 50, facility has an open floor plan Level of care to be provided or types of patients that can be taken care of :Non-emergent acute care patients Summary of plans for staffing, supply and re-supply of sites:Chain of Command, as instituted in our emergency Plan and Volunteers for staffing facilities, supplies will be taken from hospital to site and requested on WebEOC for supply and re-supply. TITUSREGIONALMEDICALCENTER: Name of Facility: Address: Mount Pleasant Convention Center 1800 N. Jefferson Mt. Pleasant, TX 75455 Contact Person and Number: Bill Luck - 903-575-4190 Number of Beds: 120 Level of care to be provided or types of patients that can be taken care of : Non-acute patients. Limited bathrooms and no on site shower facilities. Summary of plans for staffing, supply and re-supply of sites: Hospital to supply if needed for hospital patients. Local emergency management has cots and blankets. WADLEY REGIONAL MEDICAL CENTER: Name of Facility: Address: Southwest Center 3222 W. 7th Street Texarkana, TX75501 Contact Person: and Number: Robert McDonald – 903-223-3298 Number of Beds: Level of care to be provided or types of patients that can be taken care of : Summary of plans for staffing, supply and re-supply of sites: *****See Attachment OTHER REGIONAL SHELTERS Bowie: Contact Name: Agency: Address: Phone: Email: Cass: Contact Name: Agency: Address: Phone: Email: Delta: Contact Name: Agency: Address: Phone: Email: Hopkins: Contact Name: Jim Whiteside American Red Cross 903-793-5602 jwhiteside@cableone.net Agency: Address: Phone: Email: Morris: Contact Name: Agency: Address: Phone: Email: Lamar: Contact Name: Agency: Address: Phone: Email: Red River: Contact Name: Agency: Address: Phone: Email: Titus: Contact Name: Agency: Address: Phone: Email: Brad Scott American Red Cross – Lamar Chapter 903-737-4390 Judge Harville County Judge 903-427-2680 Bill Luck 903-575-4190 Regional Nursing Homes: BOWIECOUNTYNURSING HOMES ICF/MR Facilities Evergreen Northwood Community Home 113 Northwood Nash 75569 (903) 831- 4239 New Horizons Elizabeth 4820 Elizabeth St Texarkana75503 (903) 794- 0509 New Horizons Magnolia 4125 Magnolia St Texarkana75503 (903) 794- 0509 New Horizons West 27th St 404 W 27th St Texarkana75503 (903) 794- 0509 Evergreen Cooper Lane Community Home 3312 Cooper Ln Texarkana75503 (903) 831- 4632 Evergreen Fortune Community Home 3002 Fortune Ave Texarkana75503 (903) 838- 5625 Evergreen Maryland Community Home 106 Maryland Texarkana 75501 (903) 831- 4967 Evergreen Meadow Lane Community Home #20 Meadow Ln Texarkana75503 (903) 792- 2529 Evergreen Moores Lane Community Home 3611 Moores Ln Texarkana75503 (903) 832- 2682 Evergreen Pine Knoll Community Home 3603 Pine Knoll Texarkana 75503 (903) 793- 0193 New Horizons Stillwell 2611 Stillwell Dr Texarkana75503 (903) 794- 0509 Nursing facilities that accept Medicaid and/or Medicare Heritage Plaza Nursing Center 600 W 52nd St Texarkana75501 (903) 792- 6700 Christian Care Center 1008 Citizens Trail Texarkana 75501 (903) 838- 9526 Edgewood Manor 4925 Elizabeth St Texarkana75503 (903) 793- 4645 Mshc The Waterton At Cowhorn Creek LLC 5524 Cowhorn Creek Texarkana 75503 (903) 223- 1188 Reunion Plaza Senior Care And Rehabilitation Center 1401 Hampton Rd Texarkana 75503 (903) 792- 7994 New Boston Healthcare Center 210 Rice St New Boston 75570 (903) 628- 5551 Texarkana Nursing And Healthcare Center LLC 4920 Elizabeth St Texarkana75503 (903) 792- 3812 Sunny Acres Of Dekalb 12520 Fm 1840 Dekalb 75559 (903) 667- 2572 Nursing facilities that do not accept Medicaid or Medicare Cornerstone Retirement Community 4100 Moores Ln Texarkana75503 (903) 832- 5515 CASS COUNTY NURSING HOMES ICF/MR Facilities Evergreen Choctaw Community Home 1313 Choctaw Atlanta 75551 (903) 796- 9619 Evergreen Clearview Community Home 101 Clearview Atlanta 75551 (903) 796- 5552 Nursing facilities that accept Medicaid and/or Medicare Golden Villa 1104 S William St Atlanta75551 (903) 796- 0290 Linden Healthcare Center 1201 W Houston St Linden75563 (903) 756- 5537 Rose Haven Retreat 200 Live Oak St Atlanta75551 (903) 796- 4127 Hughes Springs Ltc Partners Inc 215 Highway 161 South Hughes Springs75656 (903) 639- 2561 The Springs 704 N Taylor Rd Hughes Springs 75656 (903) 639- 2531 DELTA COUNTYNURSING HOMES Nursing facilities that accept Medicaid and/or Medicare Birchwood Nursing And Rehabilitation LP 110 W HWY 64 Cooper 75432 (903) 395- 2125 HOPKINSCOUNTYNURSING HOMES Nursing facilities that accept Medicaid and/or Medicare Sulphur Springs Health And Rehabilitation 411 Airport Rd Sulphur Springs75482 (903) 885- 7668 Carriage House Manor 210 Pipeline Rd Sulphur Springs75482 (903) 885- 3589 Rock Creek Health And Rehabilitation LLC 1414 College Street Sulphur Springs75483 (903) 439- 0107 Sunny Springs Nursing & Rehab 1200 N Jackson St Sulphur Springs 75482 (903) 885- 6571 LAMAR COUNTYNURSING HOMES Nursing facilities that accept Medicaid and/or Medicare Brentwood Terrace Healthcare And Rehabilitation Center 2885 Stillhouse Road Paris75460 (903) 784- 4111 Heritage House Of Paris Health & Rehabilitation Center 150 S.E. 47th Street Paris75462 (903) 784- 3100 Legend Healthcare And Rehabilitation - Paris 520 SE 8th St Paris75460 (903) 737- 9820 Paris Nursing & Rehabilitation Center 2900 Stillhouse Road Paris75462 (903) 785- 1601 Paris Healthcare Center 610 DeshongDr Paris75460 (903) 784- 6638 Paris Skilled Nursing Facility Inc 820 Clarksville Street 7th FlSouth Paris75460 (903) 737- 3747 MORRIS COUNTYNURSING HOMES Nursing facilities that accept Medicaid and/or Medicare Omaha Healthcare Center 205 N Giles St Omaha75571 (903) 884- 2358 Windsor Place 507 E Watson Blvd Daingerfield75638 (903) 645- 3915 RED RIVER COUNTY NURSING HOMES Nursing facilities that accept Medicaid and/or Medicare Clarksville Nursing Center 300 E Baker St Clarksville75426 (903) 427- 2236 Regency Healthcare And Rehabilitation Center At Red River 2407 West Main Street Clarksville75426 (903) 427- 3821 TITUS COUNTYNURSING HOMES ICF/MR Facilities Pleasant Living Inc 2003 Happy St Mount Pleasant 75455 (903) 577- 8055 Nursing facilities that accept Medicaid and/or Medicare Mount Pleasant Healthcare Center 1606 Memorial Ave Mount Pleasant75455 (903) 572- 3618 Pleasant Springs Healthcare Center 2003 N Edwards St Mount Pleasant 75455 (903) 572- 5511 Greenhill Villas 2530 Greenhill Rd Mount Pleasant75455 (903) 572- 0974 Hospital-based Nursing Facilities Titus Regional Medical Center 2001 N Jefferson Mount Pleasant 75455 (903) 577- 6000 Regional Home Health Agencies: DELTA COUNTY HOME HEALTH AGENCIES Home Health Agencies that accept Medicare Cooper Home Health Inc 51 North Side Square Cooper 75432 (903) 395- 2811 HOPKINS COUNTY HOME HEALTH AGENCIES Home Health Agencies that accept Medicare 1st Choice Home Health 1091 Church Street Sulphur Springs75482 (903) 439- 4757 At Home Healthcare 858 Gilmer Sulphur Springs75482 (903) 885- 5606 Cypress Home Care 1304 Church St Sulphur Springs75482 (903) 438- 8400 Heritage Home Health 301 Gilmer Street Suite A Sulphur Springs 75482 (903) 561- 7250 Hospice At Memorial 1228 Church St Sulphur Springs75482 (903) 438- 4448 Legacy Hospice 301 Gilmer StSte A Sulphur Springs75482 (903) 569- 5167 Vibrant Home Health Care Inc 1707 S Broadway Suite #4 Sulphur Springs75482 (903) 454- 2273 Home Health Agencies that do not accept Medicare Hearts Choice Health Care Inc 1335 Shannon Road East Sulphur Springs75482 (903) 439- 6030 LAMAR COUNTY HOME HEALTH AGENCIES Home Health Agencies that accept Medicare At Home Healthcare 2775 NE Loop 286 Paris 75460 (903) 785- 5467 Country Style Health Care Of Texas 1603 Lamar Avenue Paris75460 (903) 567- 7770 Critical Provisions Inc 1705 E Houston Street Paris75460 (903) 739- 9090 Cypress Home Care 5020 SE Loop 286 Paris 75460 (903) 784- 8088 Hometown Home Health Services 2815 Fm 79 Paris 75460 (903) 737- 0116 Jordan Health Services 3745 Lamar Paris 75460 (903) 785- 4326 Legacy Hospice 2675 NE Loop 286 Paris 75460 (903) 784- 1147 Mays Home Care 385 Stone Avenue Paris75460 (903) 785- 6297 Mays Hospice Tx LLC 3310 B Lamar Ave Paris75460 (903) 785- 4357 Millennium Home Care Of NE Texas 3160 Clarksville Street Paris75460 (903) 737- 9865 On Call Home Health And Rehab Services 147 North Collegiate Drive Paris 75460 (903) 784- 6300 Paris Signature Home Health Inc 420 N Collegiate Paris 75460 (903) 785- 4900 Platinum Home Health Inc 140 S Collegiate Dr Paris 75460 (903) 739- 8070 Premier Home Care And Rehab / Premier Hospice 750 Clarksville St Paris75460 (903) 737- 9010 Red River Homecare LLC 6345 Lamar Road Reno75462 (903) 739- 9483 Home Health Agencies that do not accept Medicare Delta Home Health Care Of Greenville Inc 1705 E Houston Street Paris75460 (903) 739- 9600 Delta Home Health Care Of Paris Inc 1705 E Houston Street Paris75460 (903) 784- 1486 Genesis Pediatric Home Health 35 12th SE Paris75460 (855) 436- 7334 Home Helpers Homecare Inc 2845 Loop 286 NE Paris75460 (903) 784- 5500 Mays Plus Inc 3310 A Lamar Avenue Paris75460 (903) 783- 0525 Nurses Unlimited Inc 2625 N E Loop 286 Paris 75460 (903) 783- 0489 On Call Elder Care 147 North Collegiate Drive Paris 75460 (903) 905- 4975 Paris Pediatric Home Health Care Inc 3605 NE Loop 286 Suite 200 Paris 75460 (903) 737- 4337 Platinum Palliative & Hospice Care Inc 140 South Collegiate Drive Suite 10 Paris 75460 (903) 783- 1818 Red River Health Care Systems Inc 2152 Clarksville Street Paris75460 (903) 785- 4070 Visiting Angels Of Paris 1849 Lamar Ste 200 Paris 75460 (903) 784- 3902 Waterford Hospice LLC 420 N Collegiate Drive Paris 75460 (903) 785- 1800 MORRIS COUNTY HOME HEALTH AGENCIES Home Health Agencies that accept Medicare Cypress Home Care 200 Scurry St Daingerfield75638 (903) 645- 7854 RED RIVER COUNTY HOME HEALTH AGENCIES Home Health Agencies that accept Medicare Country Home Care 1505 W Main St Clarksville75426 (903) 427- 8366 Cypress Home Care 389 US HWY 82 West Clarksville75426 (903) 427- 4598 Hometown Home Health Services 597 US Highway 271 South Bogata 75417 (903) 632- 4790 Lewis Home Health Care Inc 157 North Main Street Bogata75417 (903) 632- 2173 TITUS COUNTY HOME HEALTH AGENCIES Home Health Agencies that accept Medicare Best Star Home Health Inc 2001 W Ferguson Road Suite 1010 Mount Pleasant75455 (903) 577- 9119 Chambers Home Health Agency Of Northeast Texas Company 801 North Madison Mount Pleasant 75455 (903) 572- 9700 Champion Home Health Services 1002 N Jefferson Avenue Mount Pleasant75455 (903) 577- 0355 Cypress Basin Hospice Inc 207 Morgan Street Mount Pleasant75455 (903) 577- 1510 Cypress Home Care 1318 S Jefferson Mount Pleasant 75455 (903) 577- 0577 Hnb Home Health Agency 406 2nd St Mount Pleasant75455 (903) 577- 5666 Hometown Home Health Services 1007 North Jefferson Mount Pleasant 75455 (903) 577- 9412 Integracare Of North East Texas 106 Morgan Mount Pleasant 75455 (800) 572- 8751 Jordan Health Services - Pediatrics 203 W 20th Street Suite A Mount Pleasant 75455 (903) 577- 8822 Mays Home Care 804 West 16th Suite 1 Mount Pleasant 75455 (903) 577- 0748 Premier Home Care Inc 2605 West Ferguson Rd Mt Pleasant 75455 (903) 667- 2000 Texas Helping Hands Inc 116 East 3rd Street Mount Pleasant75455 (903) 572- 4280 Home Health Agencies that do not accept Medicare At Home Healthcare 806 N Jefferson Avenue Mount Pleasant75455 (903) 577- 9877 Outreach Health Services 618 South Jefferson Ave Mt Pleasant 75455 (903) 575- 9251 Regional Health Departments: Regional Mental Health Agencies: Regional Assisted Living Facilities: BOWIE COUNTY ASSISTED LIVING FACILITIES Assisted Living - Type A Facilities Independent Living Of Texarkana LLC 3120 Smith St Texarkana75501 (903) 831- 3911 Mshc Colonial Lodge Of Texarkana LLC 5001 N Elizabeth Texarkana 75503 (903) 792- 0838 Mshc The Oaks Assisted Living LLC 4317 Mcknight Rd Texarkana75503 (903) 838- 5001 Mshc Whispering Pines Of Texarkana, LLC 5002 N Elizabeth Texarkana 75503 (903) 792- 8014 Assisted Living - Type B Facilities Cornerstone Retirement Community Personal Care Unit 4100 Moores Ln Texarkana75503 (903) 832- 5515 Sterling House Of Texarkana 4204 Moores Ln Texarkana75503 (903) 838- 3562 The Magnolia Alzheimer's Assisted Living 4205 Richmond Meadows Texarkana 75503 (903) 838- 7319 CASSCOUNTY ASSISTED LIVING FACILITIES Assisted Living - Type B Facilities Wesley House 1102 S Williams Atlanta 75551 (903) 796- 6300 HOPKINSCOUNTY ASSISTED LIVING FACILITIES Assisted Living - Type A Facilities Wesley House 1044 Church St Sulphur Springs75482 (903) 439- 0529 Assisted Living - Type B Facilities Hopkins House 890 Camp St Sulphur Springs75482 (903) 439- 1202 LAMARCOUNTY ASSISTED LIVING FACILITIES Assisted Living - Type A Facilities Paris Oaks 2905 N Main St Paris75460 (903) 784- 3243 Assisted Living - Type B Facilities Paris Oaks 2905 N Main St Paris75460 (903) 784- 3243 Pine Tree Ranch 2990 Pine Mill Rd Paris75460 (903) 783- 0652 Spring Lake Assisted Living And Memory Care Community 750 N Collegiate Drive Paris 75460 (903) 785- 1110 Sterling House Of Paris 2410 Stillhouse Rd Paris75462 (903) 784- 8800 The Home Place 115 NE 27th St Paris75460 (903) 739- 9450 MORRISCOUNTY ASSISTED LIVING FACILITIES Assisted Living - Type A Facilities Bluebonnet Elite Assisted Living 102 Floyd St Naples75568 (903) 897- 9600 TITUSCOUNTY ASSISTED LIVING FACILITIES Assisted Living - Type A Facilities Mount Pleasant Assisted Living 2009 N Edwards Mount Pleasant 75455 (903) 572- 8123 Assisted Living - Type B Facilities Mount Pleasant Hospitality House 804 West 16th St Mount Pleasant75455 (903) 572- 9893 Mt Pleasant Assisted Living 2013 N Edwards Mount Pleasant 75455 (903) 572- 8123 Mt Pleasant Assisted Living 2011 N Edwards Mount Pleasant 75455 (903) 572- 8123 Villa Of Mount Pleasant 1714 N Edwards St Mount Pleasant 75455 (903) 577- 0759 Villa Residential Care Of Mount Pleasant 1712 North Edwards St Mount Pleasant 75455 (903) 577- 0759 Vintage Lace Inc 409 W 1st Mount Pleasant 75455 (903) 577- 0158 Regional School Districts: REGIONAL SCHOOL DISTRICTS INFORMATION Region 8 ISDs Click on name to view website (where available). All area codes are 903. District Superintendent Phone # Atlanta ISD Mr. Sidney Harrist, Interim 796-4194 Avery ISD Mr. Barry Bassett 684-3460 Avinger ISD Mr. Kenny Abernathy 562-1271 Bloomburg ISD Mr. Mike White 728-5216 Chapel Hill ISD Mr. Marc Levesque 572-8096 Chisum ISD Ms. Diane Stegall 737-2830 Clarksville ISD Ms. Pam Bryant 427-3891 Como-Pickton CISD Ms. Sandra Billodeau 488-3671 Cooper ISD Mr. Jason Marshall 395-2112 Cumby ISD Mr. Lance Campbell 994-2261 Daingerfield-Lone Star ISD Mr. Pat Adams 645-2239 DeKalb ISD Mr. David Manley 667-2566 Detroit ISD Mr. Steve Drummond 674-2208 Fannindel ISD Mr. Harvey Lynn Milton 367-7251 Harts Bluff ISD Mr. Eddie Johnson 572-5427 Hooks ISD Ms. Kathy Allen 547-6077 Hubbard ISD Ms. Traci Drake 667-2645 Hughes Springs ISD Mr. Rick Ogden 639-3800 Jefferson ISD Dr. Sharon D. Ross 665-2461 Leary ISD Mr. Jim Tankersley 838-8960 Liberty-Eylau ISD Mr. Nick Blain, Interim 832-1535 Linden-Kildare CISD Mr. Clint Coyne 756-5027 Malta ISD Ms. Linda Estill 667-2950 Maud ISD Mr. Robert Stinnett 585-2219 McLeod ISD Mrs. Cathy May 796-7181 Miller Grove ISD Mr. Steve Johnson 459-3288 Mount Pleasant ISD Mr. Terry Myers 575-2000 Mount Vernon ISD Mr. Rick Flanagan 537-2546 New Boston ISD Dr. Gary VanDeaver 628-2521 North Hopkins ISD Ms. Donna George 945-2192 North Lamar ISD Mr. James Dawson 737-2000 Paris ISD Mr. Paul Trull 737-7473 Pewitt ISD Dr. David Fitts 884-2804 Pittsburg ISD Ms. Judy Pollan 856-3628 Pleasant Grove ISD Ms. Margaret Davis 831-4086 Prairiland ISD Mr. James Morton 652-6476 Queen City ISD Mr. Rob Barnwell 796-8256 Red Lick ISD Ms. Rose Mary Neshyba 838-8230 Redwater ISD Ms. Anne Farris 671-3481 Rivercrest ISD Mr. Rickey Logan 632-5205 Roxton ISD Mr. Dan Pickering, Interim 346-3213 Saltillo ISD Mr. Paul Jones 537-2386 Simms ISD Mr. Rex Burks 543-2219 Sulphur Bluff ISD Mr. Robert (Robin) Ross 945-2460 Sulphur Springs ISD Mrs. Patsy Bolton 885-2153 Texarkana ISD Mr. James Henry Russell 794-3651 Winfield ISD Mr. Danny Denton 524-2221 College/University President Phone # Texas A. & M. - Commerce Dr. Keith D. McFarland 886-5011 Texas A. & M. - Texarkana Dr. Stephen Hensley 223-3002 Texarkana College Mr. Frank Coleman 838-4541 Northeast Texas Community College Dr. Bradley Johnson 572-1911 Paris Junior College Dr. Pamela Anglin 785-7661 AreaColleges and Universities Regional Churches: