File
advertisement

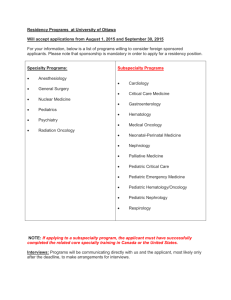
Running head: EXPLORING CULTURE ESSAY 1 Exploring Culture Essay Kelsey D. Vormbrock University of Kentucky EXPLORING CULTURE ESSAY 2 Abstract Since 2010 the cases of childhood cancer have increased by nearly 24%, causing an urgent need for more doctors. These certified doctors are more commonly known as Pediatric Hematologists/Oncologists. They are the ones that work with children and young adults suffering from cancer and blood diseases. This paper presents a brief overview of the disease itself as well as the patients that are involved. It is meant to convey not only the importance and growing urgency for these specialists but also explain the cultural behaviors that the majority of them practice and in which they believe. The main purpose, however, will be to give insight into these doctors attitudes towards their jobs, coping with the inevitable hardships, as well as their religious values and beliefs in alternate forms of medicines. Keywords: Cancer, Doctor, Medicine, Pediatrics, Chemotherapy, Ethics, Morals EXPLORING CULTURE ESSAY 3 Exploring Culture Essay A majority of people know someone who has had cancer or who has been affected by this awful disease, but do the majority of those people know a child who is living with or has lived with cancer? The answer to this is usually no. This is because childhood cancers are very rare, making the caregivers of those children all the more important. The doctors that work with these children are called pediatric oncologists. They face the day-to-day challenges that come with working with those children. Pediatric oncologists have special beliefs, values, lifestyles and ethics based solely on whom their clientele is and come together to form a society with hopes of bettering the future of childhood cancer. The road to becoming a pediatric oncologist is not one without struggle. Those interested in pursuing a career in pediatric oncology, or going in to any medical field for that matter, must first obtain a bachelor’s degree. Most students planning on going to medical school will get a degree in some sort of life sciences; however, this is not a requirement for admission to medical school. Taking the MCAT is one of the most important steps in becoming a pediatric oncologist. The MCAT is a standardized test that measures students on problem solving, critical thinking and scientific knowledge (Education Portal, 2011). How well one does on this test will determine their admission to medical school and how good of a program into which they can be accepted. Applying for and choosing which medical school to go to will be another very important decision. Upon graduation from medical school these new doctors must obtain a medical license before beginning their three-year residency. After the residency has been completed, they must be certified by the American Board of Pediatrics in order to begin a fellowship. Because many childhood cancers, such as leukemia, lymphoma and osteosarcoma are blood or bone related, it is not uncommon for pediatric oncologists to complete a fellowship in both pediatric hematology EXPLORING CULTURE ESSAY 4 and oncology. Once the fellowship has been completed they can become board certified in pediatric hematology and/or oncology. The basic job description of a pediatric oncologist is to treat children with cancer and blood diseases. Figure 1. Ben with Dr. Salman [Photograph.] Retrieved October2, 2014, from: http://www.leememorial.org/childrenhospital/images/Ben-with-Dr-Salman.jpg is a good representation of how these Doctors interact with their patients. As mentioned previously, childhood cancer is very rare and even harder to diagnose. Suspicions of cancer are usually first noticed by a family doctor or pediatrician and from there the children are sent to the pediatric oncologists for further testing. Depending on the symptoms being shown by the patient, the pediatric oncologist will order a test for the most likely cancer. Different cancers require different tests in order for a proper diagnosis to be made. These tests could include blood tests, inspection of cell samples, or other forms of genetic and molecular testing. Diagnosing a child is not a one-person job however. These doctors work closely with other oncologists and specialists to ensure that they make an accurate diagnosis and design a proper treatment plan. They must also work closely with other specialists throughout the child’s treatment. For example, they EXPLORING CULTURE ESSAY 5 would need to work closely with a brain surgeon if a child were to need surgery to have a tumor removed from the brain. They would have to communicate the type of tumor, location and best way of going about the removal. For this reason pediatric oncologists would be considered a collectivist culture. Through shared decision making, good intuition, and an all-around team effort they are able to make decisions with the children’s best interest in mind. These doctors have a lot of personality traits that are very unique to most people. Two of these traits are dedication and hard work. They spend eight to 12 years in school before they can even begin their career. The work that they go through is not easy and it’s not always enjoyable. An example of this would be their terminology, also known as jargon, while part of any medical profession, is a different language to many doctors, and learning the terms is no easy task. For example, chemotherapy, carcinoma, benign, in situ, malignant, metastasis, sarcoma, and tumor are all terms that would generally only be used by oncologists and aren’t terms that are known to many people outside of the medical field. There are also many acronyms for the therapies and treatments such as BMT (bone marrow transplant) and TBI (total body irradiation.) With approximately 13,400 new cases of childhood cancer each year, the community of pediatric oncologists is a fast growing one. According to the Bureau of Labor Statistics the demand for pediatric oncologists is expected to increase by 24% from 2010 to 2020. Due to the longevity of schooling and the vast spread of medical professions it is hard to keep up with the increasing numbers. It takes a very strong-willed person to endure that many years of school and training, but for those who can, their willingness to help people sets them apart. Very few people in this world are gifted with the natural ability to interact with people and even fewer have the desire to help them. These doctors are not only fighting for these children’s lives but fighting to EXPLORING CULTURE ESSAY 6 find cures and preventions so that no child will ever have their life cut short due to cancer. Figure 1. Supporting a patients parent [Photograph]. Retrieved October 15, 2014, from: http://everydaylife.globalpost.com/DMResize/photos.demandstudios.com/getty/article/97/6/87739927.jpg?w=6 00&h=600&keep_ratio=1&webp=1 Any doctor in a medical field has to have a certain quality of ethics but those involved in pediatric oncology must have ethics of a totally different sort. Figure 2. Supporting a Patients Parent [Photograph.] Retrieved October15, 2014, from: http://everydaylife.globalpost.com/DMResize/photos.demandstudios.com/getty/article/97/6/87739927.jpg?w=600&h+600&keep_ratio= 1&webp=1 demonstrates the tough situations that these doctors are put in and how they must handle them. They have to be able to deal with not only the children but also their parents; and telling them that their child has cancer is never easy. “The subsequent trend, at least in the U.S., has been toward an increasingly patient-centered approach in which the physician may recommend, but the patient ultimately decides” (Berg, 2007.) In the case of children, the majority of those with childhood cancer are not old enough to be able to understand and make their own decisions. It is the job of the physician to inform the parents of the options as well as the side effects of each and let them have the final decision. They may feel that the decision of the parent is not the most logical and can advise against it but ultimately it is not their place to go against the wishes of the parent. While it is commonly thought that any doctor working in pediatrics would only deal with children, that is not necessarily the case for pediatric oncology. Not all cases of childhood EXPLORING CULTURE ESSAY 7 cancers are seen in young children or even teenagers. There often are cases involving adults up to 30 years old. Megan Halstead, a child life specialist working at the University of Kentucky Hematology/Oncology clinic said, “Recent studies have shown that young adults under the age of 30 who have a pediatric cancer usually fair better when they are treated by a pediatric oncologist on pediatric protocols” (M. Halstead, personal communication, September 22, 2014). Due to the range in their patients’ ages pediatric oncologists must have the ability to work with children, teenagers, young adults, and adults. Most people either work really well with kids and not adults or vice versa. These doctors have the people skills to do it all though. It is imperative that these doctors are able to deal with children in a gentler manner than the adults, as it is harder for children to comprehend why all the medication is needed and why they are always at the hospital having tests run. On the other hand, the doctors must be able to turn around five minutes later with an older patient and tell them exactly what is going on without trying to lessen the severity of the older child’s situation. The lifestyle of a pediatric oncologist is much different from a typical white collar worker and from most doctors even. The majority will work a 60-plus- hour work week between office hours, seeing patients, running labs, and doing paperwork. While the hours may not be as demanding as a general surgeon or primary caretaker it is still a lot more than the average 40hour work week. Most of them however, are still able to be flexible with their hours and make time for families. The average salary for these doctors in the United States is $195,249 (Healthcare Salaries, 2014). While the pay is good and most of them enjoy their work, there is still the inevitable tragedy that comes with the job. Approximately 2,000 children, under the age of 19, die each year in the United States from cancer. Cure rates for most childhood cancers are at an all-time high of 75% (National Cancer Institute, 2014). With this number you can figure EXPLORING CULTURE ESSAY 8 that out of every 100 patients a single oncologist will lose 25. To put that into perspective most people will only experience about 27 close deaths in a lifetime. While that is a lot of death to be around there are also many positive points to the profession. A 75% cure rate means that these doctors do see more survival than deaths. They can also have the satisfaction of knowing that even though they may not have been able to cure a child, they were able to give them the best quality of life possible. These traits in mind, pediatric oncologists would be considered a more passive culture. While the doctors may not be okay with their statistics, they have to accept them and not let the numbers affect their work. Due to the number of deaths each pediatric oncologist will experience in their career, there are mandatory courses that these doctors must go through before becoming certified. These courses include training in death and dying, and classes in child development (M. Halstead, personal communication, September 22, 2014). Once they have been certified they must continue going through CEU’s (Continuing Education Units) and professional development seminars. Dr. Nick Code says: I try to get all my work done in the office before I leave the office and when I walk out of the office I just kind of turn a switch in my brain and I just don’t dwell on it. Now once in a while I think a little bit more about it but I realize it’s not doing anyone any good for me to dwell on it (Dr. N. Code, Personal Communication, September 23, 2014). Some of these doctors will seek out therapeutic help in times of especially tough cases but it is not mandatory. Although religious beliefs vary widely across races, cultures, lifestyles, and careers there is a common trend among pediatric oncologists when it comes to the subject. The two people that were interviewed for this paper both identified as Christian and said that a good amount of EXPLORING CULTURE ESSAY 9 the people they work with also practice some variation of religion. While not everybody in a medical profession practices religious values, many feel that it is too tough of a field to go through without something to believe in. As most people know children are naturally very curious, but when you throw something like cancer and the chance of death into the equation that innocent curiosity intensifies. While it is generally hospital policy to not talk about religious affiliation with patients, if a dying child asks if God and Heaven are real very few people are going to tell them no. When Megan Halstead was asked how she responded to religious questions from the children she said, “I typically don’t talk about it unless they bring it up themselves and I try to use really open ended questions. But everybody’s beliefs are special and I just try to honor it” (M. Halstead, personal communication, September 22, 2014). When asked what the best advice is that they can give to someone, regarding their profession or the patients they work with, these doctors tend to focus on happiness and the treatment of their patients. Dr. Nick Code explains it as thinking about whether or not you will be happy in ten years and ensuring that one is capable of separating themselves from work at the end of the day. When Megan Halstead was asked she took to the patient perspective and said: They’re kids first. First and foremost they’re kids. And that nine times out of ten they just wanna be treated like kids… You just have to develop your listening skills and your observation skills and you know, just let the kid tell you what they’re wanting and that not to assume anything… It may be nonverbal cause they don’t have the words for it, but just don’t assume anything. First and foremost they’re kids (M. Halstead, personal communication, September 22, 2014). EXPLORING CULTURE ESSAY 10 As demonstrated above the tasks that come with being a pediatric oncologist stretch far beyond simply curing children of their cancer. Yes they prescribe treatments such as chemotherapy and radiation and their overall goal is to rid the children of their disease but most of us don’t realize what goes on in these treatment sessions, much less outside of them. To these kids their doctors are more than just doctors. They are more than just the people stabbing them with needles and making their hair fall out. To these kids their doctors are their heroes, their support systems, their friends. They are the ones putting all of their time and effort into healing them, caring for them, and getting to know them as the brilliant children that they are rather than the walking disease that most people see them as. Many people think of pediatric oncologists and they think one of two things. First: What kind of a morose person wants to work with dying children all day? Or second: It takes an extremely selfless and compassionate person to be able to work with severely and terminally ill children. Not everybody will have the same opinion of these doctors but they are not morbid death doctors, rather they are lights of hope for children that have none. As you can see it takes a lot of hard work and determination to become a pediatric oncologist. These men and women that endure those never ending years of schooling, those all night study sessions and the piles of debt that are always adding up are one of life’s great wonders. They have more in common than just their job title. They all work towards the same goal of healing those children plagued by the awful diseases of cancer. They share the same ethical and moral values when it comes to their job and their patients. They are a well-defined culture of hard working heroes. They are warriors against cancer; and much like the road to beating cancer is not easy, neither is the road to curing it. EXPLORING CULTURE ESSAY 11 References Decker, Fred. Pediatric Oncologist Job Description. Retrieved from http://everydaylife.globalpost.com/pediatric-oncologist-job-description-4491.html Education Portal (2011, March 11). Become a Pediatric Oncologist: Education and Career Roadmap. Retrieved from http://educationportal.com/articles/Become_a_Pediatric_Oncologist_Education_and_Career_Roadmap.ht ml Healthcare Salaries (2014). Pediatric Oncologist Salary. Retrieved from http://www.healthcaresalaries.com/physicians/pediatric-oncologist-salary HealthyChildren.org (2013, May 13). What is a Pediatric Hematologist/Oncologist?. Retrieved from http://www.healthychildren.org/English/family-life/health-management/pediatricspecialists/Pages/What-is-a-Pediatric-Hematologist-Oncologist.aspx Delany, C., Galvin, J. (October, 2014). Ethics and Shared Decision-making in Pediatric Occupational Therapy Practice. Developmental Neurorehabilitation. 17(5), 347-354. doi:10.3109/17518423.2013.784816 Veniou, A., Tentolouris, N. (2013). Factors That Influence the Doctor-patient Relationship. Archives of Hellenic Medicine/ Arheia Ellenikes Latrikes. 30(5), 613-618. doi: 91871024