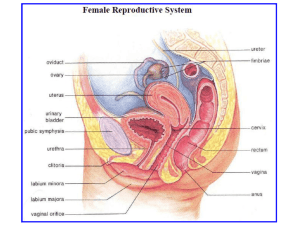
Female Reproductive System
advertisement

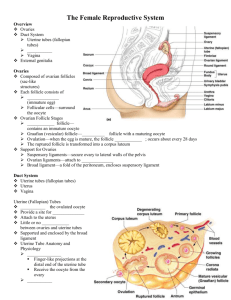
Female Reproductive System Ovary – attached to broad uterine peritoneum by double fold of peritoneal serosa (mesovarium). o Peritoneal suspensory ligament of ovary attached to upper pole of ovary and carries ovarian vessels and nerves. o Uterine pole of ovary is attached to lateral aspect of uterus by ovarian ligament that contains no blood vessels or nerves but may contain smooth muscle. o Each ovary has central medulla and peripheral cortex. o Medulla is inner zone consisting of loose connective tissue and numerous tortuous arteries and veins from hich small branches reach into cortex. o Cortex contains very large number of multicellular ovarian follicles. o Spindle-shaped cells of stroma look like fibroblasts but many have potential to differentiate into steroid-secreting cells of theca interna. o Ovary covered by simple cuboidal epithelium – germinal epithelium. o Dense connective tissue capsule between germinal epithelium and cortex is tunica albuginea of ovary. o Primordial follicle – single layer of flattened follicular cells surrounds small primary oocyte. Oocyte typically has large round euchromatic nucleus with prominent dark nucleolus. Inactive ovarian follicles – tend to be located in superficial cortex beneath dense tunica albuginea. o Primary follicle – oocyte has grown in size and ii surrounded by cuoidal to columan granulosa cells. Zona pellucida – glucosaminoglycan-rich zone forms between granulosa cells and oocyte. Theca folliculi – developing in immediately surrounding stroma, with external fibrous layer (theca externa) and internal steroidogenic layer (theca interna) that is well vascularized. Theca interna contains clusters of foamy-appearing theca interna cells – secrete estrogen precursors that cross granulose cells of follicle that complete synthesis of estrogens. o Secondary follicle – marked by formation of centrally located antrum that appears between granulosa cells. Membrana granulose can now be separated into granulose proper, culmulus oophorus, corona radiata. o Graafian follicle – very large follicle that presumably would have ovulated. o Atretic follicle – granulose cells undergo degeneration by apoptosis, and their distinctly small dense pyknotic nuclei appear among normal granulose cell nuclei. Remnants of larger ovarian follicles may appear as wavy collagenous scars but most atretic follicles are completely phagocytosed by macrophages. May be seen at any stage of development. o Corpus luteum – forms following ovulation and expulsion of oocyte. Walls of empty follicle collapse and fold extensively. Following ovulation, granulose cells enlarge and become secretory – basement membrane surrounding follicle breaks down and allows small blood vessels to penetrate previously avascular layer of granulosa cells. Temporary endocrine gland – formed from remnants of Graafian follicle’s granulosa cells and theca interna cells. Granulosa lutein cells (progesterone) are large pale spherical whereas theca lutein cells (estrogen) are smaller, have less cytoplasm and often stain poorly – both cells secrete steroids. Uterine tube (Fallopian Tube). o Oviduct extends from near ovary to lumen of uterus in mesenteric fold (mesosalpinx that carries blood vessels and nerves) that is attached to broad ligament. o Opens medially by uterine os into uterine cavity, and opens laterally (abdominal os) into peritoneal cavity near ovary. o From lateral to medial: fimbriated end of infundibulum, ampulla, isthmus, intramural portion that traverses uterine wall – mucosal folds progressively differ from distal to proximal end. o Thickness of muscular layer varies along tube, being thinnest at infundibulum and becoming progressively thicker as it approaches wall of uterus – inner circular layer and outer longitudinal layer of smooth muscle – create peristaltic movement toward uterus. o Mucosa covered by ciliated and secretory simple epithelium – principal cells have cilia that beat towards uterus (move viscous mucous film that covers luminal surface of oviduct), nonciliated secretory cells are peg cells and are interspersed among ciliated cells (secretions provide nutrients for oocyte and agents that promote activation of spermatozoa). o Number of ciliated cells greatest at fimbriated end and least in intramural end. o Mucosa folding especially complex in infundibulum and ampulla, becoming progressively less so in isthmus and reduced to little more than small bumps in intramural portion of oviduct. o Highly folded mucosa helps to slow transit of oocyte along fallopian tube, to allow time for fertilization, which usually occurs in ampulla. o Infundibulum can be identified in sections where there’s obvious discontinuity in surrounding wall. o Epithelium of fimbria is continuus with serosal mesothelium on outside of infundibulum. o Ampulla – comprises nearly 2/3 of oviduct. Cervix – part of uterus with distal portion extending into vagia. o Cervical canal opens into uterine lumen at internal os and opens into lumen of vagina at external os. o Outer mucosal surface of portio vaginalis is ectocervix. o Epithelium of lumen of cervix (cervical canal) is simple columnar secretory. o Vagina lined with stratified squamous nonkeratinized epithelium. o Abrupt demarcation line between epithelia of cervix and vagina – border between ectocervix and endocervix, and typically occurs just inside opening of cervical canal into vagina (at external os of cervix). o Mucosa lining cervical canal forms deep furrows – plicae palmatae (endocervical/cervical glands). Epithelium consists of tall columnar cells with basal nuclei; some cells are ciliated but most are mucoid, secreting substance that occludes opening of cervical canal protecting uterus from bacteria. o Wall of cervix contains mostly dense collagenous and elastic fibers among which are distributed relatively few smooth muscle cells. Vagina – fibromuscular sheath that extends from cervix to external genitalia. o Lined with mucosa that has transverse rugae. o Epithelium is stratified squamous nonkeratinized epithelium that is rich in glycogen, especially in surface cells – lactic acid accumulation and vagina’s low pH. o Lamina propria divided into more superficial dense papillary layer (1/3-1/2 thickness) and deeper/looser vascular layer. o Muscularis layer consists mainly of longitudinal smooth muscle but includes some inner circular fibers. Female repro organs formed in embryo from tissue that would in presence of testosterone (from Leydig cells) and antimullerian hormone (from Sertoli cells) differentiate into male structures. o Male hormones preserve embryonic mesonephric (Wolffian) duct that forms epididymis, ductus deferens, seminal vesicle. o In female, this duct degenerates and paramesonephric (Mullerian) duct is preserved that forms cervix, uterus, oviducts. Ovaries and Oocyte Development. o Ovaries attached to broad ligament by peritoneal fold (mesovarium), attached to uterus y ovarian ligament, and attached to pelvic wall by suspensory ligament. o 2 major functions: gametogenesis and steroidogenesis. o Gametogenesis – oogenesis in female. Developing gamete is oocyte and mature gamete is ovum. o Primary hormones produced are estrogen and progesterone. Estrogen promotes growth and maturation of sex organs and promotes formation of female secondary sex characteristics. Progesterone prepares uterus for implantation and pregnancy and prepares mammary gland for lactation. o Each ovary covered with single layer of squamous or cuboidal cells possessing microvilli and occasional cilia – germinal epithelium. Directly under is tunica albuginea of ovary. Underlying tunica albuginea is cortex, which is composed of cellular connective tissue with scattered smooth muscle fibers and ovarian follicles at various stages of development. Each ovary has central medulla, which is compsed of loose connective tissue and contains blood vessels, lymphatics, nerves. o Maturation of oocyte – primary oocytes formed in developing female embryo. At 6 weeks PF, small number of primordial oogonia migrate to genital ridge and begin to undergo rapid mitosis. By 5-7 months PF, each oocyte becomes surrounded by follicle cells and begins first meiotic division. Meiosis interrupted at prophase I and pimray oocytes remain arrested for 12-50 years. Just prior to ovulation, one or more primary oocytes stimulated to complete meiosis I – two resulting cells are secondary oocyte and first polar body. Secondary oocyte immediately begins second meiotic division but becomes arrested in metaphase Ii – oocyte at ovulation has not completed 2nd meiotic division, which is completed only upon entry of spermatozoon. o Maturation of ovarian follicles – occurs in cortex of ovary and independent of maturation of oocyte. Each follicle composed of 1 oocyte surrounded by follicle cells. Growth of follicle occurs uder influence of FSH, which is secrete from anterior pituitary. Primordial follicle – resting stage, lasting between 12-50 years; found beneath tunica albuginea, with single squamous layer of follicular cells surrounding oocyte. Primary follicle – first stage of follicular maturation that occurs during reproductive years, and persists for several repro cycles. Oocyte – becomes active and enlarges. Follicular cells – proliferate and become cuboidal and then stratified granulosa cells. Zona pellucida – occupies space between follicle cells and oocyte; PAS positive region that’s rich in GAGs and glycoproteins and secreted by oocyte. Theca folliculi – sheath of stromal cells surrounding follicle, subdivided into: o Theca interna – inner, highly vascularized ovoid secretory cells that secrete estrogen precursors that are converted by granulosa cells. o Theca externa – connective tissue layer containing smooth muscle cells, collagen fibers. Secondary follicle – stage of follicular growth defined by presence of fluid-filled antrum (fluid-filled, oocyte is pushed to one side). Cumulus oophorus – thickened portion of granulosa cells, which projects into antrum. Corona radiata – granulose cells immediately surrounding oocyte – send processes through zona pellucid to communicate with oocyte via gap junctions. Graafian (mature, tertiary) follicle – further state of maturation of secondary follicle, occurring within 1 repro cycle, marked by rapid expansion in follicular size in preparation for ovulation. Ends with mid-cycle surge in LH inducing completion of first meiotic division of oocyte and triggering ovulation within 24 hours. Luteinization begins to occurs and granulosa and theca cells begin to produce progesterone. Prior to ovulation, granulosa cells secrete enzymes that erode ovarian tunica albuginea, creating visible thin spot on ovarian surface – stigma. o Ovulation – occurs when secondary oocyte with corona radiata is expelled from follicle and transported into oviduct. Caused mainly by increased volume of follicular fluid, enzymatic breakdown of follicle wall, prostaglandin-induced contraction of smooth muscle fibers in externa. Only 1 oocyte is released in ach cycle. Fertilization takes place in ampulla of oviduct. After ovulation, remaining granulosa cells form corpus luteum – follicular wall becomes highly folded and cells increase in size and known as granulosa lutein and theca lutein, derived from granulosa and theca interna. Theca lutein cells secrete estrogens and granulosa lutein cells secrete progesterone – prepare uterus for implantation and inhibit FSH and LH, which prevents development of new follicles. If pregnancy occurs, hCG from placenta maintains corpus luteum, which remains primary source of estrogen and progesterone for 1st 8 weeks of pregnancy. If no pregnancy occurs, estrogens and progesterone decrease approximately 12 days after ovulation – luteal cells autolyse and form corpus albicans, a white scar of hyaline material that slowly disappears. Great majority of developing follicles don’t make it to maturity – degenerate at various stages of development (atretic follicles). PCOS – Graafian follicles persist. Oviducts (Fallopian tubes) – divided into infundibulum with fimbriae, ampulla, isthmus, intramular portion. o Infundibulum is funnel-shaped end of oviduct that opens into peritoneal cavity – just prior to ovulation it moves to overlie site of Graafian follicle in order to capture emerging oocyte. Muscularis relatively thin compared to lumen size, with extensive mucosal folds, extending from opening as fimbriae (ciliated cells sweep oocyte into infundibulum). o Longest portion is ampulla, which is usually site of fertilization. Function is to nourish both oocyte and sperm and retain them to optimize chances for fertilization. Primary means of moving ovum is peristalsis – epithelial cells become shorter and fewer of them are ciliated, mucosa becomes thrown into extremely convoluted folds, muscularis becomes thicker. o Final portions of oviduct function to move fertilized ovum into uterus by peristalsis – isthmus and intramural portion have small lumen, short non-ciliated epithelial cells, few mucosal folds, thick muscularis. o If oviduct doesn’t function properly, embryo can implant outside of uterus – ectopic pregnancy – tubal pregnancy in oviduct. Uterus – provides environment for developing embryo and functions to expel baby at birth. o Divided into body (fundus) and cervix, which extends into vagina. o Wall of uterine body is divided into: myometrium, endometrium, perimetrium. o Myometrium – extremely thick muscle layer that’s loosely organized into 3 layers, and serves to protect developing fetus and to expel fetus at birth. Size of muscle fibers increases significantly and new muscle cells are produced. Undergoes an increase in collagen content during pregnancy. o Endometrium – divided into stratum functionalis and stratum basalis. Stratum functionalis proliferates and degenerates during menstrual cycle – composed of simple columnar epithelium with both ciliated and secretory cells. Epithelium invaginates into simple tubular glands – uterine glands. Highly vascularized with spiral arteries that are important during menstruation. Stratum basalis – underlies stratum functionalis and is retained during menstruation. Cells act as stem cells to regenerate stratum functionalis with each cycle. Nourished by short straight arteries. Endometriosis – endometrial tissue is present in peritoneal cavity and can lead to ectopic pregnancies but can be treated with hormone therapy. o Hormonal control of menstrual cycle – cycle is 28 days. Proliferative/follicular stage (day 5-15) – influenced by estrogen from eveloping ovarian follicles. At beginning of this phase, stratum functionalis is absent and stratum basalis is thin. Endometrium rapidly proliferates. Epithelial cells from base of glands residing in stratum basalis reconstitute uterine glands and endometrial surface. Stromal cells proliferate and spiral arteries regenerate into lower 2/3 of stratum functionalis. Secondary/luteal phase (day 16-28) – influenced mainly by progesterone from corpus luteum. Uterine glands enlarge and become corkscrew-shaped and begin to secrete glycogenrich fluid. Spiral arteries lengthen, become more coiled, extend nearly to surface, Menstrual phase (day 1-4) – influenced by decline in estrogens and progesterone as corpus luteum degenerates. Spiral arteries begin to contract as progesterone levels decline, causing stratum functionalist to become ischemic. Surface epithelium disrupted and blood vessels burst. Blood, uterine fluid, and sloughing epithelial and stromal cells from stratum functionalis constitute menstrual flow. Drugs to predict and control fertility. Birth control pills contain progesterone, effectively mimicking secretory phase. Emergency contraception often consists of high-dose progesterone. Mifepristone (RU-486) is abortifacient that is competitive inhibitor for progesterone – without progesterone, uterine lining doesn’t maintain itself in secretory phase and implanation of embryo cannot be sustained. Pregnancy test kits may test for presence of hCG, which is produced by placenta and excreted in urine. Ovulation prediction kits may test for presence of LH, which is only present for less than 12 hours around time of ovulation. = progesterone - - - - - - - - = estrogens + + + + + + = LH = FSH Cervix – lower 1/3 of uterus and does not contain spiral arteries and its epithelium is not sloughed off during menstruation. o Function is to provide tight muscular opening to uterus that allows sperm to enter but provides barrier to infection. o 2 surfaces – endocervix bordering cervical canal and ectocervix, which is its surface facing vaginal lumen. o Endocervix – mucosa is continuous with endometrium and is composed of simple, mucus-secreting columnar cells. Thrown into deep crypts – plica palmatae. Mucus produced by epithelial cells helps to protect against bacterial invasion. o Ectovervix – external surface of part of cervix that projects into vagina. Its mucosa is continuous with vaginal lining and has epithelium of stratified squamous cells. Abrupt squamocolumnar junction between endocervical and ectovervical epithelia typically occurs at external os. Vagina – connects uterus to outside of body and acts in transport of sperm to uterus and in expulsion of newborn. o Nonkeratinized stratified squamous epithelium – no glands and no mucus secretion. o Lamina propria has many thin-walled blood vessels that contribute to diffusion of vaginal fluid across epithelium. o Mucosa throw into transverse folds/rugae. o Vaginal epithelium responds to hormonal changes during menstrual cycle – glycogen stores in epithelial cells and reaches maximal levels at ovulation, after which time glycogen-rich superficial layer of epithelium is shed. o Breakdown of glycogen by bacteria in vagina produces lactic acid, causing environment to have acidic pH – inhibits growth of other bacteria, bacterial pathogens, fungus, limits time sperm can survive in vagina. Vulva – labia majora, labia minora, clitoris, vestibule of vagina. o Labia majora – paired outer folds of relatively adipose epidermal tissue. o Labia minora – hairless inner epidermal folds. o Clitoris – body of erectile tissue, homologous to corpus cavernosum of penis, which becomes engorged during sexual stimulation. o Vestibule of vagina contains numerous minor glands. Barthilin’s glands – paired mucous lands which open to either side of vaginal orifice and homologous to bulbourethral glands of male in that they secrete during sexual arousal. Paraurethral glands – form network of tissue in space anterior to vaginal wall, surrounding and opening to urethra. Arise from same embryonic tissue that forms prostate.