Your State`s Base-Benchmark Plan Excludes Methadone for Opioid
advertisement

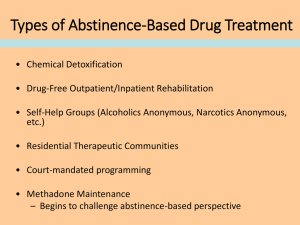
Template Language: Your State’s Base-Benchmark Plan Excludes Methadone for Opioid Addiction Treatment As a highly effective medication to assist in the treatment of opiate addiction, STATE X’s essential health benefits (EHB) package should and must cover medication-assisted treatment that utilizes methadone. Excluding use of methadone from Affordable Care Act (ACA) coverage in STATE X violates several provisions of the ACA, including the parity, and non-discrimination provisions of the federal law. To be brought into compliance with the requirements of the law, STATE X’s base-benchmark plan must be supplemented to cover medication-assisted treatment that utilizes methadone. Medications are an essential tool to assist in the treatment of all chronic illnesses. There are only three federally approved medications to treat chronic opioid addiction. The rate of prescription drug misuse and heroin abuse is increasing nationally; SAMHSA estimates that X# of people (in STATE X, if data is available) need treatment for problems with illicit and prescription opiates. Excluding the use of methadone in treatment for opioid addiction from ACA coverage will severely restrict access to a treatment that is an approved standard of practice for opioid addiction. Numerous studies recognize the effectiveness of methadone as a medication for maintenance, detoxification and medically supervised withdrawal. Methadone is a highly regulated medication, with extensive accreditation, licensing and other oversight requirements at both the federal and state levels. Methadone offers pharmacologic benefits that help to support an individual’s efforts to achieve and sustain abstinence, and is particularly effective for patients with long term histories of chronic opioid addiction who have a high narcotic tolerance. Methadone is also effective in helping individuals to stay in treatment. Research has also shown that methadone is a cost-effective medication. Excluding coverage for treatment with methadone would violate the parity requirements of the ACA. o Excluding coverage for one of the three medications approved for the treatment of opioid addiction would violate the parity requirements of the ACA. The basebenchmark plan covers a number of medications to help in the treatment of other chronic illnesses including hypertension, cancer and heart disease. Allowing the methadone exclusion to remain in STATE X’s EHB plan would be the equivalent of the plan also excluding coverage for 1/3rd of the medications approved for the treatment of another chronic illness. o In addition, under the parity requirements of the ACA, a plan’s MH/SUD coverage must meet standards of clinical practice. Methadone is a highly effective medication for individuals with opiate addiction. Medications are a critical piece of the continuum of care for all chronic illnesses. Excluding coverage for a medication that been an important part of the continuum of care for people with opioid addiction is contrary to established national standards of care and accordingly violates parity. Excluding methadone would disproportionately and harmfully restrict access to an effective treatment for certain individuals with opioid addiction. To be brought into compliance with the parity requirements of the ACA, the base-benchmark plan must be supplemented to cover treatment that utilizes methadone. o If the base-benchmark in your state is a small group plan: As a small group plan, STATE X’s base-benchmark has not had to comply with the federal parity law and will very likely need to be supplemented to meet the parity requirements of the EHB. A review of the base-benchmark plan’s medical necessity criteria used to determine the exclusion of medication-assisted treatment that utilizes methadone is necessary to complete a full parity analysis. Stakeholders in STATE X need to have full access to the plan’s medical necessity criteria to determine if treatment with methadone can be legally excluded from the EHB. Under the parity requirements of the ACA, if the criteria used to determine which medications to assist in the treatment of SUD or mental illness should be covered is different from and/or applied more stringently than the criteria used to determine coverage for medications used to assist in the treatment of other illnesses, that would also represent a violation of the law. o If the base-benchmark in your state is a large group plan: A review of the basebenchmark plan’s medical necessity criteria used to determine the exclusion of medication-assisted treatment that utilizes methadone is necessary to complete a full parity analysis. Stakeholders in STATE X need to have full access to the plan’s medical necessity criteria that was used to determine that use of methadone could be legally excluded. Under the parity requirements of the ACA, if the criteria used to determine which medications to assist in the treatment of SUD or mental illness should be covered is different from and/or applied more stringently than the criteria used to determine coverage for medications used to assist in the treatment of other illnesses, that would also represent a violation of the law. Excluding use of methadone for the treatment of opioid addiction would be inconsistent with the non-discrimination requirements of the ACA. Allowing EHB plans to exclude use of methadone from coverage is contradictory to the ACA’s requirement that the EHB addresses the healthcare needs of diverse segments of the population. If medicationassisted treatment utilizing methadone is excluded as a service, individuals with opiate addiction will have their choice of treatment severely restricted. Methadone is a highly effective medication that is consistent with recognized standards of clinical care and is beneficial to diverse groups of people whose health needs have traditionally not been well met. People with opioid addiction have been particularly stigmatized and have historically experienced considerable discrimination. Singling out for denial of coverage a specific medication which is essential for a significant number of people with a disability to become and stay well suggests the type of discrimination that is precluded by the ACA. Excluding coverage for one of the three medications approved to help treat opioid addiction also is contrary to ensuring meaningful consumer choice in care, a central principle of the ACA. Methadone has a distinct pharmacological profile for which there is no adequate substitute for certain patient populations. Excluding coverage of the use of methadone to treat opioid addiction through the ACA would severely and unfairly restrict access to and consumer choice for an effective medication. The full range of medications approved for the treatment of MH and SUD should be covered in the EHBbenchmark plan.