Perinatal Substance Abuse
Program
Dept of Alcohol and Drug Services
(DADS)
Presented by Lara Windett
M.A., MFT, LPPC
Certified Addiction Specialist (CAS)
The Department of Alcohol & Drug Services
exists within the overall
Santa Clara Valley Health & Hospital System
Dedicated to the health of the whole community
regardless of ability to pay
Background
PSAP was Brainchild of Anthony
Puentes, MD, MPH, 1987
Funding stream
Goal of PSAP Program
PSAP Keeps babies
out of the NICU
NICU costs ~$2,100 – 5000 per day
2007 140 babies exposed, 30 in NICU
Avg Length of Stay: 15 days
PSAP Treatment Works!
92% drug/alcohol free - neg tox
screens
Perinatal Drug Exposure
Overview
1992 Study
Estimated 15-18% of pregnant women
use alcohol or drugs.
PSAP Admission Statistics
PSAP = Empowerment Model
Comprehensive Intensive Outpatient
Treatment
Medically Monitored
Multidisciplinary Approach
Day Care for clients’ children
Transportation
PSAP Client Eligibility
Resident of Santa Clara County
Pregnant or Early Parenting Women
18 years or older
On Methadone (MMT) or opiate
dependent
Hx or DOA abuse or currently using
Family Wellness Court Referrals
Medi-cal, Valley Care II, sliding scale
fee, or other insurance (Kaiser)
Length of PSAP Stay
Assigned a Licensed Therapist, PSW
Case Management
Individualized Tx Plan
Typical Treatment Episode: 6-12 months
Staff
HCPM II
3 Therapists (MFT)
MD
Health Ed Specialist
1 Health Services Representative
3 day care aides (1/2 codes)
1 Community Worker (van) (1/2 codes)
Volunteers
Current PSAP Client Demographics
~Capacity for 65+
Women ages 19 to 43 years
23% pregnant
10 clients on Methadone (3 pregnant)
30% Caucasian
33% Latina,
9 % Asian/Pacific Islander
18% Mixed Race
2% African American
8 % Declined to State
30% in THU’s
CPS Cases ~70%
Prop 36 ~40%
FWC 30%
Probation Only - 20%
DEJ – 10%,
Out Patient Drug Treatment in
Santa Clara County – Including
Methadone
On the VMC campus
Readily accessible - pregnant OPIOID
DEPENDENT patients (Methadone candidates)
are scheduled for admission the next business day
All Patients can call Gateway 1-800-488-9919
Providers can call Central Valley Clinic
408 885-5400 Front Desk
408 885-4064 PSAP Clerical
Items to Remember if a Patient
is in PSAP Treatment
We ask for a verification of OB Care/complete the
referral to VMC if no care is scheduled for
pregnant people.
We obtain a release to speak with the OB and all
MDs in the patient's life.
We obtain a release to Public Health.
We obtain a release to the Pedi and we alert the
Pedi (and OB) if the patient drops out of treatment.
Overview of AOD
Treatment/Concerns
Red flags
When interviewing/observing the patient
When considering the history
Risks associated with various drugs
To the pregnancy
To the baby
Substances to Be Discussed
Opioids
Cigarettes
Alcohol
Marijuana
Methamphetamine
Amber
32 y.o. Woman and the mother of an 8
y.o.
Unplanned pregnancy
Using daily
Heroin by injection 2 grams/day
Cocaine
Cigarettes 2 PPD
Seeking admission to methadone
program
Amber
Stealing to obtain drugs
Isolated – only living relative is
maternal grandmother
8 y.o. son is being raised by patient’s
grandmother
Father of baby is using and at risk of
deportation
Amber
Medically indigent
History of depression and anxiety
History of domestic violence (prior
relationship)
Amber
Frustrated – requested tubal ligation
at 23
Frightened – concerned about
damage already done to baby
Motivated
Requests residential treatment
Resolves to leave boyfriend if he will not
get into treatment
Red Flags: Multiple & Obvious
Patient volunteering history of
substance abuse
Physical exam remarkable for multiple
tracks and physical withdrawal
Life in disarray
Chaotic and disrupted family
relationships
Why Share this Story?
Opioid dependence requires medical
intervention
Pregnant patients need treatment to
prevent adverse outcomes
Women caring for infants need
treatment to be functional mothers
Pregnancy can be a Huge
Motivation for Change: Amber
Stabilized on methadone maintenance
Completed residential treatment
Permanently left the boyfriend who
continued to use
Delivered drug free
A Sense of Hope:
12 Years Later Amber is…
Abstinent and still in treatment
Raising her daughter
Working
Prevalence of AOD Abuse in
Pregnancy
2008 and 2009 data from the National
Survey on Drug Use and Health found
that among pregnant women ages 15 to
44, the youngest ones generally
reported the greatest substance use.
Also, pregnant women ages 15 to 17
had similar rates of illicit drug use (15.8
percent or 14,000 women) as women of
the same age who were not pregnant
(13.0 percent or 832,000 women).
Brenda
Referred to treatment for history of
methamphetamine abuse
Worked as a medical assistant until
about two years ago
Served as caretaker for mother who
died of breast cancer
After mother died, dad was diagnosed
with lung cancer; patient served as
caretaker
Reported having a prescription for
vicodin
Brenda
Reported taking prescribed vicodin for
chronic back pain (occasionally)
Denied history of prescription opioid abuse
Weekly u tox screens consistently positive
For a variety of prescription opioids
Not just for vicodin
Easy access to unlimited supply of
prescription opioids
Transferred to methadone maintenance
26
Prescription Opioid Abuse May
Not Be Obvious
Consider the history
Unusual number of painful conditions for
a young healthy patient
Multiple opioid prescriptions during
pregnancy
Multiple ER visits for complaints of pain
Multiple care providers/no regular
provider
Opioids for unusual indications
27
Patient’s Appearance on
Opioids
Normal
Sedated with small pupils
Symptoms of withdrawal
Sweats/chills/gooseflesh
Lacrimation/rhinorrhea
Yawning/sneezing
Irritable/anxious/fidgety
Vomiting
Ask About Behaviors:
Have you ever?…
Taken more than prescribed?
Taken medication after the pain was
gone?
Gotten pills from a friend or relative?
Bought pills on the street?
Written or called in a prescription for
yourself?
Tried to stop and found you couldn’t?
Ask about Reasons for Use
Manage emotions?
Deal with stress?
Feel high?
Numb everything or go to sleep?
Opioids: Three to Seven Times
Higher Rates of…
Still birth
Fetal growth retardation
Low birth weight
Small head circumference
Prematurity
Neonatal mortality
Heroin: Medical Risks
Associated With Injection
Cellulitis
Abscesses
Endocarditis
Hepatitis
HIV infection
Wound Botulism
Opioid Dependence in
Pregnancy: Treatment
Currently, methadone maintenance is
the gold standard
Buprenorphine maintenance looks
promising and may be more available
in the future (not FDA approved)
A comfortable, stable mother
increases the likelihood of a healthy,
term delivery
Impact of Methadone Treatment
Reduced deaths
Reduced IVDU
Reduced HIV
seroconversion
Reduced crime
days
Reduced relapse
Improved health
Improved
relationships
Improved
productivity
Improved social
functioning
Additional Benefits During
Pregnancy
Increased participation in prenatal care
Reduced obstetrical complications
Improved maternal nutrition
Daily observation in clinic while dosing
Therapeutic Dosing With Methadone
Suppresses opioid withdrawal
symptoms
Reduces opioid cravings
Provides a stable opioid blood level
Allows a patient to concentrate on
counseling/program to support
recovery
Minimizes side effects; patient should
not be sedated
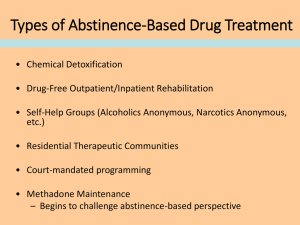
Methadone Withdrawal:
Not Recommended During
Pregnancy
The relapse rate is high (80%)
Risk of intrauterine demise
Risk of premature labor/miscarriage
What can you say to a patient wanting
to Withdraw from MMT?
Send them to their primary CSLR/the
addiction MD to discuss
Methadone Withdrawal:
Not Recommended After
Delivery?
Like insulin, methadone stabilizes a
chronic illness
The normal brain has an endogenous
opioid system that may never function
properly in an opioid dependent patient
Very high relapse rate when
methadone treatment is discontinued
Methadone: Effects on the
Baby
No known birth defects
More likely to be born at term
Lower birth weight/smaller head
circumference at birth
May experience developmental delay
during the first year of life
Not associated with learning difficulties
Increased SIDS with opioid exposure
Methadone and Breastfeeding
Negligible amounts of methadone are
passed in breast milk
The American Academy of Pediatrics
considers methadone compatible with
breastfeeding at any dose
Methadone: Neonatal
Withdrawal
Safer than heroin withdrawal in utero
Experienced by 60-80% of exposed
babies
Usually occurs within the first 2-3 days
of life; may occur within the first month
Usually treated with an opiate agonist
Duration of treatment is days to months
Can be life threatening without
treatment
Opiates: The Neonatal
Abstinence Syndrome
High-pitched cry, irritability
Poor feeding, vomiting, diarrhea
Hyper tonicity (stiff muscles)
Tremors
Sneezing
Sweating
Occasionally seizures
Symptoms of Opioid Withdrawal
W = wakefulness
I = irritability
T = tremulousness, temperature variation,
tachypnea
H = hyperactivity, high-pitched persistent cry,
hyperacusia, hyperreflexia, hypertonus
D = diarrhea, diaphoresis, disorganized suck
R = rub marks, respiratory distress, rhinorrhea
A = apneic attacks, autonomic dysfunction
W = weight loss or failure to gain weight
A = alkalosis (respiratory)
L = lacrimation
Clarissa
23 y.o.
Pregnant with first child
Smoking 1½ - 2 PPD since late teens
“I will only quit if the doctor tells me my
baby will die if I do not quit now”
“My whole family smokes; I grew up
with it; I’ve been around it my whole
life”
United States (1996-1998)
National Household Survey on Drug
Abuse (NHSDA)
Survey of pregnant women
Cigarettes
Alcohol
Any Illicit Drug
% using
# fetuses/yr
20.3%
14.8%
2.8%
1.2 million
0.8 million
0.2 million
Ebrahim, SH, Gfroerer, J. Pregnancy-related substance use in the United States
during 1996-1998. Obstet Gynecol 2003; 101:374.
Cigarette Smoking
Smoking during pregnancy is the most
modifiable risk factor for poor birth
outcome
It is associated with 5% of infant
deaths, 10% of preterm births, and
30% of small for gestational age infants
Trends in smoking before, during, and after pregnancy - Pregnancy Risk
Assessment Monitoring System (PRAMS), MMWR Surveill Summ. 2009 May
29;58(4):1-29.
Cigarettes in Pregnancy:
Obstetric Complications
Adverse Event
Relative Risk
Placental Abruption
1.4-2.5
Placenta Previa
1.4-4.4
Stillbirth
1.2-1.4
Pre-term PROM
1.9-4.2
Preterm Birth
1.3-2.5
Low Birth Weight
1.3-10.0 dose
dependent
dose dependent
dose dependent
Clinical Outcomes in Pregnant
Women who Quit Smoking
20% reduction in low birth weight babies
17% decrease in pre-term births
Average increase in birth weight of 280g.
Quitting before 30 weeks can still
positively affect birth weight
Cigarette Smoking in Pregnancy
& Other Drug Use
10 times higher use of marijuana
22 times higher use of cocaine
21 times higher use of amphetamine
Vega, WA, Kolody, B, Hwang, J, Noble, A. Prevalence and magnitude of
perinatal substance exposures in California. N Engl J Med 1993; 329:850
In Utero Cigarette Exposure:
Congenital Malformations
May contribute to anomalies
associated with focal vascular
disruption
Cleft lip with or without cleft palate
Gastroschisis
Anal atresia
Transverse limb reduction defects
Risk may be modified by genetic
factors
In Utero Cigarette Exposure:
Effects on the Newborn
There is a dose-response relationship
between maternal cigarette use and
infant…
Stress
Hypertonicity
Excitability and irritability
May be due to neurotoxicity or withdrawal
With second hand smoke exposure
there is an increased risk of low birth
weight
In Utero Cigarette Exposure:
Postnatal Morbidities
Morbidity
Neonatal death
RR 1.2 - 1.4
SIDS
RR 2.0 – 7.2
Prenatal exposure a higher
risk than postnatal 2nd hand
exposure
Respiratory infections, asthma,
otitis media, infantile colic,
bronchiolitis, short stature,
childhood obesity, type 2
diabetes in adulthood
Heart disease and lung cancer
in never smokers
Second-hand smoke increases
risk by 20-30%
52
In Utero Cigarette Exposure:
Behavioral Problems
Toddlers (12-24 mo.s) showed a high and
escalating pattern of disruptive behavior
Children developed Oppositional Defiant
Disorder at double the rate of controls
ODD is a precursor of Conduct Disorder
Seen in older children and adolescents
Characterized by persistent antisocial
behaviors (lying truancy, vandalism, aggression)
NIDA Notes 2008: Vol.21 No. 6
In Utero Cigarette Exposure:
Cognitive Outcomes in 9-12 yr
olds
IQ impacted (dose response effect)
Poorer impulse control
Many individual WISC tests w/
significant dose response effects
Poorer performance on tests requiring
visuoperceptual skills.
Auditory memory particularly impacted
WISC = Wechsler Intelligence Scale for Children
Medical Issues for the Children
of Smokers
Increased incidence of smoking
initiation
20% higher if mom smoked up to 1PPD
60% higher if mom smoked 1PPD or more
Diabetes mellitus
Four times higher with more than 10
cigs/day
Increased asthma in adult offspring
Decreased sperm volume/count in adult
male offspring
Alcohol
“Of all the substances of abuse
(including cocaine, heroin, and
marijuana), alcohol produces by far
the most serious neurobehavioral
effects in the fetus.”
IOM Report to Congress, 1996
A look at Denial/PreContemplation: Denise
28 y.o. pregnant woman and the
mother of 7 and 3 y.o. boys
Pregnant for the 5th time
History of two 2nd trimester
miscarriages
Started drinking at 23 (not pregnant)
Denise
Drinking 1-2 shots of peppermint
schnapps daily until about 1 yr ago
Quit drinking when learned was
pregnant with second child, now age 3
GA ~ 9wks when quit
Growth and development of this child
appear normal
Denise
Drinking 5 shots of peppermint
schnapps daily for the past year
Drinking this pregnancy until GA ~33
wks
Not worried about the baby because
Last baby was okay
U/S during this pregnancy looks normal
Alcohol Use During
Pregnancy:
Obstetrical Complications
Increased risk of second-trimester
abortion
50% increase in fetal mortality
Infant withdrawal (3-12 hrs after
delivery)
Fetal Alcohol Spectrum Disorders
Alcohol is a Teratogen that
Freely Passes the Placenta
Teratogen: a substance that causes
abnormal physical development
Behavior teratogen: a substance that
causes impaired cognitive, affective,
social, reproductive, and/or
sensorimotor behavior, even in the
absence of obvious physical problems
Prenatal Alcohol Exposure Can
Cause:
Death
Malformation
Growth deficiency
Functional deficits
Teratogenic Effects Depend
On:
Dose of alcohol
Pattern of exposure (binge vs.
chronic)
Developmental timing of exposure
Susceptibility (genotype of mother
and fetus)
Synergistic reactions with other drugs
Interaction with nutritional variables
Dose-Response Effects
Higher maximum blood alcohol levels
result in more severe neurotoxicity
Binge drinking is particularly dangerous
Males appear to be more susceptible
than females
SOME CREDIBLE INCREDIBLE
WEBSITES!
(Thanks Mark Stanford, PhD)
Addiction Technology Transfer Center
http://www.nattc.org/asme.asp
Brookhaven Addiction Research. Center for Translational Neuroimaging
http://www.bnl.gov/CTN/addiction.asp
National Institute of Drug Abuse (NIDA). Medical and Health Professionals http://www.nida.nih.gov/medstaff.html
Moyers On Addiction: Addiction As A Disease
http://www.pbs.org/wnet/closetohome/science/
The Institute of Medicine. Marijuana and Medicine: Assessing the Science Base
http://www.nap.edu/readingroom/books/marimed/index.html
NIDA Science & Practice Perspectives
http://www.drugabuse.gov/Perspectives/
National Institute of Mental Health (NIMH). Medications
http://www.nimh.nih.gov/health/publications/medications/complete-publication.shtml
UCLA Addiction Clinic
http://www.uclaisap.org/addclinic/
University of Utah. Genetic Science Learning Center
http://learn.genetics.utah.edu/units/addiction/issues/treatments.cfm
Counselor Magazine for Addiction Professionals
http://www.counselormagazine.com/component/option,com_magazine/Itemid,1/
Society of Neuroscience. Advancing the Understanding of the Brain and Nervous System
http://www.sfn.org/
DADS:
Sccdads.org
Please ask me for more – or e-mail me!!!
Content Provided by:
Deborah Stephenson, MD, MPH
Dept of Alcohol & Drug Services
Santa Clara Valley Health & Hospital System
Mark Stanford, PhD
Dept of Alcohol & Drug Services
Santa Clara Valley Health & Hospital System
Margaret Williams, M.S., RD, H.E.S.
Dept of Alcohol & Drug Services
Santa Clara Valley Health & Hospital System
Thank you!