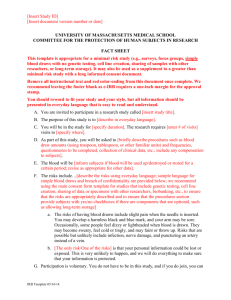
16.2 Adherence to Protocol
advertisement

If applicable: Insert collaborating groups’ logo/s TROG xx.xx Insert descriptive title identifying the study design, population, interventions, and, if applicable, trial acronym Draft Protocol: Version [insert number], [insert date] Sponsor: Trans Tasman Radiation Oncology Group (TROG) ABN: 45 132 672 292 Address: Calvary Mater Newcastle, Locked Bag 7, HRMC, NSW 2310, Australia Phone: +61 (0)2 401 43911 Fax: +61 (0)2 401 43902 Email: trog@trog.com.au Website: www.trog.com.au TROG Representative: Insert Name Protocol Authorisation: sign Trial Chairperson: Insert Name Address: Insert Address Email: Insert Email date Protocol Authorisation: sign Trial Coordinator: Insert Name Address: Insert Address Email: Insert Email Phone: Insert phone number Universal Trial Number: Insert UTN date Revision Chronology: Example . . . 2004-Jan-30: Original Amendment 01.: Primary reason for amendment: . . . 2004-Feb-7: Changes in Section 7.1 regarding composition of comparator placebo TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 1 of 40 TRIAL MANAGEMENT COMMITTEE Role /Affiliation Name Trial Chairperson Radiation Oncologist State Radiation Oncologist State Radiation Oncologist State Radiation Oncologist State Radiation Oncologist State Radiation Oncologist State Radiation Oncologist State Medical Oncologist Surgical Oncologist Radiation Therapist Medical Physicist Translational Researcher Quality of Life Health Economist Pathology Statistician Central Trial Coordinator Consumer 1 Consumer 2 FOREWORD This document is intended to describe a Trans Tasman Radiation Oncology Group (TROG) trial and to provide information about procedures for screening, enrolling and treating trial participants. It is not intended that the Protocol be used as a guide for the treatment of patients who are not enrolled on this trial. TROG will not accept any data for analysis unless each Trial Site has Human Research Ethics Committee (HREC) approval for patient enrolment and participation in this trial. Amendments to the document may be necessary; when approved by TROG, these will be circulated by the Trial Coordinating Centre, on behalf of TROG, to Trial Sites participating in the Trial. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 2 of 40 ABBREVIATIONS Example abbreviations: amend as required ANC Absolute neutrophil count AUC Area under the curve BaCT Centre for Biostatistics & Clinical Trials BSA Body Surface Area CRF Case Report Forms CRT Conformal Radiotherapy CT 4D CT CBCT 4D CBCT Computerised Tomography Time dependent CT Cone Beam Computerised Tomography Time dependent CBCT CTC AE Common Terminology Criteria for Adverse Events CTV Clinical Target Volume DQLI Dermatology Quality of Life Index DRR Digitally Reconstructed Radiographs DVH Dose Volume Histogram ECOG Eastern Co-operative Oncology Group EGFR EPID Epidermal Growth Factor Receptor Electronic Portal Imaging Device FACIT Functional Assessment of Chronic Illness Therapy FACT Functional Assessment of Cancer Therapy FBE Full blood examination FDG-PET Fluorodeoxyglucose – Positron Emission Tomography FDG-PET-CT FDG-PET computed tomography FFS Failure-free survival FNA Fine Needle Aspirate GCP Good Clinical Practice GTV Gross Tumour Volume Hgb Haemoglobin HHIA-S Hearing handicap inventory for adults, screening version HPV Human papilloma virus HREC Human Research Ethics Committee HRQOL Health-related Quality of Life IB Investigator’s Brochure IDSMC Independent Safety Data Monitoring Committee TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 3 of 40 IHC Immunohistochemistry LRF Locoregional failure LTF Liver function test MDASI-HN M.D. Anderson Symptom Inventory – Head and Neck MID Minimal important difference MRI Magnetic Resonance Imaging NCI National Cancer Institute OAR Organ at Risk OPC Oropharyngeal cancer OPSCC Oropharyngeal squamous cell carcinoma OS Overall survival PEG PET Percutaneous enterogastric Positron Emission Tomography PIC Participant Information Sheet and Consent Form Plt Platelets PRO Patient Reported Outcome PRV Planning Organ at Risk Volume PSS Performance Status Scale PTV Planning Tumour Volumes QA Quality Assurance QALY Quality-adjusted life year RT Radiation Therapy RTP Radiotherapy Treatment Planning SAE Serious Adverse Event SCC Squamous Cell Carcinoma TCC Trial Coordinating Centre TGA Therapeutic Goods Administration TMC Trial Management Committee TSC TROG Scientific Committee TCOO TROG Central Operations Office UAE Unexpected Adverse Events 3D 3-dimensional TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 4 of 40 TABLE OF CONTENTS TRIAL SUMMARY .................................................................................................................................... 8 TRIAL SCHEMA ...................................................................................................................................... 10 1.0 INTRODUCTION AND BACKGROUND ........................................................................................ 11 1.1 [Insert Name of Intervention] ............................................................................................... 11 1.2 Previous Studies .................................................................................................................... 11 1.3 Choice of Comparator ........................................................................................................... 11 1.4 Patient Reported Outcomes .................................................................................................. 11 2.0 TRIAL OBJECTIVES ...................................................................................................................... 12 2.1 Research Hypothesis ............................................................................................................. 12 2.2 Objectives .............................................................................................................................. 12 2.3 Endpoints ............................................................................................................................... 12 3. TRIAL DESIGN ............................................................................................................................. 13 4. PARTICIPANT SELECTION AND ELIGIBILITY ............................................................................... 13 4.1 Source of participants............................................................................................................ 13 4.2 Accrual numbers and timelines ............................................................................................. 13 4.3 Inclusion Criteria .................................................................................................................... 13 4.4 Exclusion Criteria ................................................................................................................... 14 5. SCREENING ................................................................................................................................. 14 5.1 Screening Log......................................................................................................................... 14 5.2 Informed Consent .................................................................................................................. 14 5.3 Participation in other research .............................................................................................. 14 6. REGISTRATION / RANDOMISATION .......................................................................................... 15 7. TRIAL PARTICIPANT ASSESSMENTS ........................................................................................... 15 7.1 Pre-registration assessments ................................................................................................ 15 7.2 Pre-treatment assessments (baseline) .................................................................................. 15 7.3 On-treatment assessments ................................................................................................... 15 7.4 Post radiotherapy assessments ............................................................................................. 15 7.5 Disease Progression ............................................................................................................... 16 7.6 Withdrawal from treatment or follow-up ............................................................................. 16 7.7 Participant transfers .............................................................................................................. 17 8. TRIAL PARTICIPANT ASSESSMENT TABLE .................................................................................. 18 9. RADIOTHERAPY TREATMENT REGIMEN .................................................................................... 19 9.1 Pre-trial treatment ................................................................................................................ 19 9.2 Treatment timelines .............................................................................................................. 19 9.3 Radiotherapy fractionation schedules .................................................................................. 19 9.4 Radiotherapy planning and delivery...................................................................................... 19 9.5 Treatment scheduling and gaps ............................................................................................ 20 TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 5 of 40 9.6 Concomitant therapy............................................................................................................. 20 9.7 Supportive care guidelines .................................................................................................... 20 9.8 Non-permitted medications/treatments .............................................................................. 21 9.9 Radiotherapy Quality Assurance (QA) ................................................................................... 21 10. CHEMOTHERAPY /SURGERY TREATMENT REGIMEN [if applicable] ......................................... 22 10.1 Chemotherapy [if applicable] ................................................................................................ 22 10.2 Insert name of chemo agent [if applicable] .......................................................................... 22 10.3 Surgical Therapy [if applicable] ............................................................................................. 22 10.4 Drug supply, storage, accountability and disposal ................................................................ 24 10.5 Investigator’s Brochure ......................................................................................................... 24 11. PATIENT REPORTED OUTCOMES AND HEALTH ECONOMICS ................................................... 24 11.1 Patient Reported Outcome questionnaires .......................................................................... 24 11.2 Non-English Speaking Patients [if applicable] ....................................................................... 26 11.3 Patient Reported Outcome Completion and Missing Data ................................................... 26 11.4 Completion of Patient Reported Outcome questionnaires................................................... 26 12. TRIAL ADMINISTRATION AND QUALITY ASSURANCE ............................................................... 27 12.1 Participating Centres ............................................................................................................. 27 12.2 Investigator Training .............................................................................................................. 27 12.3 Data acquisition ..................................................................................................................... 27 12.4 Site Visits ............................................................................................................................... 28 12.5 Completion of the study and definition of study end date ................................................... 28 12.6 Archiving ................................................................................................................................ 28 12.7 Quality Assurance reviews .................................................................................................... 28 13. ADVERSE EVENT SCORING AND REPORTING ............................................................................ 29 13.1 Adverse Event ........................................................................................................................ 29 13.2 Serious Adverse Event (SAE) .................................................................................................. 29 13.3 Adverse Event reporting ........................................................................................................ 30 13.4 Other situations requiring expedited reporting .................................................................... 30 13.5 New Zealand reporting requirements [if applicable] ............................................................ 31 14. STATISTICAL CONSIDERATIONS ................................................................................................. 33 14.1 Sample Size Calculation ......................................................................................................... 33 14.2 Sequence Generation ............................................................................................................ 33 14.3 Endpoint Definitions .............................................................................................................. 33 14.4 Measurement of response .................................................................................................... 33 14.5 Statistical Analysis Plan.......................................................................................................... 34 14.6 Interim analyses and early termination criteria .................................................................... 34 15. RESEARCH GOVERNANCE .......................................................................................................... 35 15.1 Sponsor and Funder .............................................................................................................. 35 TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 6 of 40 15.2 Trial Chairperson ................................................................................................................... 35 15.3 Trial Management Committee .............................................................................................. 35 15.4 Independent Data Safety Monitoring Committee ................................................................ 35 15.5 Principal Investigator ............................................................................................................. 35 15.6 Consumer Representative ..................................................................................................... 36 16. PATIENT PROTECTION AND ETHICAL CONSIDERATIONS .......................................................... 36 16.1 Ethical Principles and Regulatory Compliance ...................................................................... 36 16.2 Adherence to Protocol .......................................................................................................... 36 16.3 Aboriginal and Torres Strait Islander values and principles .................................................. 36 16.4 Confidentiality ......................................................................................................................... 36 16.5 Concealment Mechanism ...................................................................................................... 37 16.6 Security and Back up of Data ................................................................................................. 37 16.7 Insurance and Compensation ................................................................................................ 37 17. PUBLICATION AND PRESENTATION POLICY .............................................................................. 37 18. REFERENCES ............................................................................................................................... 38 APPENDICES .......................................................................................................................................... 39 Suggested Appendices ...................................................................................................................... 39 TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 7 of 40 TRIAL SUMMARY Data category Information (examples provided) Primary registry and trial identifying number Australia New Zealand Clinical Trials Registry ACTRN12612000407897 Date of registration in primary registry 11 June, 2010 Secondary identifying numbers TROG 12.01 Source(s) of monetary or material support List sources and types of financial, material, and other support Primary sponsor contact details Trans Tasman Radiation Oncology Group Secondary sponsor(s) Other collaborative trials group(s) Contact for public queries Central Trial Coordinator [phone number] [email address] Contact for scientific queries Trial Chairperson or nominated TMC member [phone number] [email address] Public title Scientific title Probiotic Saccharomyces boulardii for the prevention of antibiotic associated diarrhoea (SacBo) Saccharomyces boulardii for the prevention of antibiotic associated diarrhoea—randomised, double blind, placebo controlled trial Countries of recruitment Australia, New Zealand Health condition(s) or problem(s) studied Antibiotic treatment, Clostridium difficile, diarrhoea Intervention(s) Key inclusion and exclusion criteria Study type Active comparator: S boulardii (500 mg S boulardii per day) Placebo comparator: microcristallin cellulose (matching capsules containing no active ingredients) Ages eligible for study: ≥18 years Sexes eligible for study: both Accepts healthy volunteers: no Inclusion criteria: adult patient (≥ 18 years), patient hospitalised . . . Exclusion criteria: allergy against yeast and/or Perenterol forte and/or placebos containing S cerevisiae HANSEN CBS 5926, lactose monohydrate, magnesium stearate, gelatine, sodium dodecyl sulfate, titan dioxide, microcrystalline cellulose . . . Interventional Allocation: randomised Intervention model: parallel assignment Masking: double blind (subject, caregiver, investigator, outcomes assessor) TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 8 of 40 Primary purpose: prevention Phase III Target sample size Primary outcome(s) Key secondary outcomes Trial analyses timelines 1520 Cumulative incidence of any antibiotic associated diarrhoea (time frame: 2 years; not designated as safety issue) Cumulative incidence of C. difficile associated diarrhoea (time frame: 2 years; not designated as safety issue) . . . Include time points for interim, main and final analyses. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 9 of 40 TRIAL SCHEMA Patient screened for eligibility Not potentially eligible Patient invited to participate Patient accepts Patient declines Written Informed Consent obtained Formal assessment of eligibility performed Patient NOT eligible Participant log completed Eligibility confirmed Pre-registration form completed and submitted REGISTRATION/RANDOMISATION Protocol treatment: Arm A Screening log completed Patient confirmed as potentially eligible Protocol treatment: Arm B Pre-treatment forms completed and submitted Participant commences treatment On-Treatment forms completed and submitted Participant completes treatment End of Treatment forms completed and submitted Interim analyses performed at: Insert time points Participant followed-up for x years Follow-up forms completed and submitted Main /Final analyses performed TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 10 of 40 1.0 INTRODUCTION AND BACKGROUND Description of research question and justification for undertaking the trial. The background must be properly referenced and evidenced based. 1.1 [Insert Name of Intervention] Include: Name and description of the intervention. Description, dosage, dosage regimen, and treatment period(s). o 1.2 If the intervention is a marketed drug which is being studied in this trial for a new indication, an Investigators Brochure specific to this trial should be produced by the manufacturer. If this is impractical, the background section of this protocol must be expanded to include the minimum current information as described in section 7 of the ICH GCP Guidelines. Previous Studies Summary of relevant studies (published and unpublished) examining benefits and harms for each intervention. 1.3 Choice of Comparator Provide an explanation for choice of comparators The choice of control interventions has important implications for trial ethics, recruitment, results, and interpretation. In trials comparing an intervention to an active control or usual care, a clear description of the rationale for the comparator intervention will facilitate understanding of its appropriateness. For example, a trial in which the control group receives an inappropriately low dose of an active drug will overestimate the relative efficacy of the study intervention in clinical practice; conversely, an inappropriately high dose in the control group will lead to an underestimate of the relative harms of the study intervention. 1.4 Patient Reported Outcomes Provide an explanation for the rational for measuring Patient Reported Outcomes (PROs). State what is known and unknown for this patient population, where the gaps in the literature are and explain the clinical rational for collecting the PROs. Provide an argument for the PRO variables considered relevant in your trial (e.g. for acute side effects, late effects – benefit & harm, psychological domains and core +/- other domains of functioning) TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 11 of 40 2.0 TRIAL OBJECTIVES 2.1 Research Hypothesis Include a hypothesis that is an overall covering statement for the trial and its purpose. 2.2 Objectives 2.3 Provide a detailed description of the objectives of the trial. If PRO is used in the study, make sure that the PRO objectives are identified and that the key PRO domains and time points are specified. Refer to TROG Policy TPP E5 Statistical Guidelines for further information regarding objectives. 2.2.1 Primary Objective 2.2.2 Secondary Objectives 2.2.3 Exploratory Objectives [if applicable] Endpoints Specify what endpoints are to be used in the trial and prioritise them in relation to the objectives. At least one endpoint should be associated with each objective. If PROs are identified in the objectives, describe the methods for delivering PRO endpoints and which time points are involved and the analysis metric (i.e change from baseline). Refer to TROG Policy TPP E5 Statistical Guidelines for further information on endpoints. 2.3.1 Primary Endpoints 2.3.2 Secondary Endpoints 2.3.3 Exploratory Endpoints [if applicable] TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 12 of 40 3. TRIAL DESIGN Provide a description of the type/design of trial to be conducted (e.g. double-blind, placebo controlled, parallel design). Describe measures taken to minimise/avoid bias including randomisation and blinding if applicable. 4. PARTICIPANT SELECTION AND ELIGIBILITY 4.1 Source of participants This study is being conducted in Radiation Therapy treatment centres throughout Australia and New Zealand. 4.2 Accrual numbers and timelines It is anticipated it will take xx months to complete target accrual of xxx participants. All participants will be followed for another xx months after the end of accrual, giving the trial a duration of x years. 4.3 Inclusion Criteria Patients (or a representative) must provide written, informed consent before any study procedures occur. Patients may be included in the trial only if they meet all of the following inclusion criteria at randomisation. No exceptions, waivers or exemptions will be granted. Example variables: Aged 18 years or older Has provided written Informed Consent for participation in this trial Histological or cytologically confirmed disease Stage [insert relevant stage(s)] (see appendices) Adequate haematological, renal, hepatic and pulmonary functions as defined by, eg.: Absolute neutrophil count (ANC, segs + bands) 1.5 x 109/L Platelet count 100 x 109/L Total bilirubin 1.5 x upper normal Alanine aminotransferase (ALT) 2.5 x upper normal limit Pulmonary: FeV1 > 1 litre An ECOG performance status score of [insert number] or less (see appendices) Calculated creatinine clearance > 40ml/min (Cockcroft-Gault formula – see appendices ) Life expectancy greater than [insert number] months/years Participants capable of childbearing are using adequate contraception Available for follow up TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 13 of 40 4.4 Exclusion Criteria Choose variables that are relevant to your trial. Also add any that have not been listed. Do not repeat inclusion criteria in the negative. Women who are pregnant or lactating. Previous radiotherapy to the area to be treated Previous chemotherapy Previous surgery Prior diagnosis of cancer that was: - more than 5 years prior to current diagnosis with subsequent evidence of disease recurrence or clinical expectation of recurrence is greater than 10% within 5 years of current diagnosis with the exception of successfully treated basal cell or squamous cell skin carcinoma or carcinoma in situ of the cervix Patients with clinical evidence of metastatic disease. 5. SCREENING 5.1 Screening Log Appropriately qualified personnel at the Trial Site will screen patient health records for potentially suitable patients according to the eligibility criteria in the protocol. The Trial Site will then record deidentified information relating to each patient screened on the screening log (including in-eligible patients); screening will continue until the target population is achieved. The screening log will be requested by the Trial Coordinating Centre on a regular basis for the purpose of monitoring accrual. 5.2 Informed Consent Patients must be given the current HREC approved participant information sheet for their consideration. Patients should only be asked to consent to the study after they have had sufficient time to consider the trial and the opportunity to ask any further questions. 5.3 Participation in other research Participation in other research will be considered on a case by case basis by the Trial Management Committee. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 14 of 40 6. REGISTRATION / RANDOMISATION Insert registration and/or randomisation procedures and trial coordinating centre contact details 7. TRIAL PARTICIPANT ASSESSMENTS 7.1 Pre-registration assessments The following assessments must be performed within [e.g. 6 weeks] prior to registration. Insert assessments 7.2 Pre-treatment assessments (baseline) The following assessments must be performed within [e.g. 1 weeks] prior to treatment. Insert assessments 7.3 On-treatment assessments The following assessments must be performed weekly: Insert assessments The following assessment should be conducted during weeks x, y and z (if applicable) of radiotherapy: Insert assessments At last fraction: Insert assessments 7.4 Post radiotherapy assessments 7.4.1. 4 weeks from last radiotherapy fraction Insert assessments 7.4.2. 3 months from last radiotherapy fraction Insert assessments 7.4.3. 6 months from last radiotherapy fraction Insert assessments 7.4.4. 9 months from last radiotherapy fraction TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 15 of 40 Insert assessments 7.4.5. 12 months from last radiotherapy fraction Insert assessments 7.4.6. 18 months from last radiotherapy fraction Insert assessments 7.4.7. 24 months from last radiotherapy fraction Insert assessments 7.4.8. Annually to year 5 Insert assessments 7.4.9. Annually thereafter Insert assessments 7.5 Disease Progression 7.5.1 Definition of progression Provide an appropriate definition for this trial relating to locoregional and regional (or distant) relapse or failure as applicable for the endpoints of the trial. Consider special requirements for the disease site, such as whether primary and nodal sites are considered together for a combined assessment of response. 7.5.2 Required assessments The following assessments must be performed at the time of disease progression. Insert assessments 7.5.3 Diagnosis of new cancers Provide clarification on management of response assessments relating to diagnosis of any new cancers. 7.5.4 Managing disease progression Specify treatment of participants after relapse has been detected. 7.6 Withdrawal from treatment or follow-up A Trial Participant may discontinue trial treatment for any of the following reasons: Disease progression Unacceptable toxicity TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 16 of 40 Intercurrent illness which prevents further treatment Withdrawal of consent for treatment by participant Any alterations in the participant’s condition which justifies the discontinuation of treatment in the investigator’s opinion Unable to be treated in accordance with the protocol requirements, eg. dose constraints for radiotherapy plan cannot be met Discontinuation of treatment does not necessarily indicate withdrawal from the trial. The distinction between discontinuation of treatment and withdrawal from the trial is shown by the definitions in the following subsections. 7.6.1 Protocol Treatment Discontinuation A participant would be considered to have discontinued treatment where trial related treatment is ceased according to the reason(s) outlined above. The participant may however still agree to further follow-up assessments as scheduled in section 10. The participants’ discontinuation of treatment must be documented in the medical records and transcribed onto the relevant CRF. 7.6.2 Withdrawal from Trial Trial Participants have the option to completely withdraw from the trial at any time without giving a reason. Total withdrawal would occur in the circumstance that the participant decides to completely withdraw from all treatment aspects of the trial, and does not agree to any further scheduled follow up assessments. The participants’ total withdrawal must be documented in the medical records and transcribed onto the relevant CRF. No further information will be collected from this participant for the purpose of this trial. 7.7 Participant transfers Every effort should be made for a trial participant moving from the area to continue their treatment and/or follow-up at another participating Trial Site and for this Trial Site to take over responsibility for the participant. Until the new Trial Site formally agrees (in writing) to take over responsibility and provides evidence of ethics approval, the participant remains the responsibility of the original Trial Site. Source documentation will remain at the original Trial Site. One copy of the participant’s CRFs must be sent to the new Trial Site and one copy will remain at the original Trial Site. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 17 of 40 8. TRIAL PARTICIPANT ASSESSMENT TABLE The following assessments will occur during the trial [example only – table to be updated when section 9 has been finalised] Pre Trial Treatment PreRegistration PreTreatment 2 3 Post Treatment Follow-up 1 Treatment Wk 1 Wk 2 Wk 14 Wk 24 Wk 4 3 mths 6 mths 9 mths 12 mths 16 mths 20 mths 24 mths 30 mths 36 mths 42 mths 48 mths 54 mths End of Study Participant Assessments Informed Consent Inclusion/ Exclusion Criteria Medical History Clinical assessment CT PRO assessment 6 Full blood count Adverse Event Reporting7 Treatment Arm A – [treatment] Arm B - [treatment] Translational Sub Study Informed Consent Peripheral Blood Tumour Biopsy 1 2 3 4 6 7 Follow will continue until the last trial participant completes 2 years follow-up and for a maximum of 5 years Within 6 weeks before randomisation To be done after randomisation and within 6 weeks of planning simulation Visit required for those Participants who have consented to the Translation substudy only. ECORT C30 and MDSI AEs and Toxicity to be reported via CTC AE v4 Criteria TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 18 of 40 9. RADIOTHERAPY TREATMENT REGIMEN The examples provided in this section are excerpts from the TROG collaborative RAIDER study protocol, developed by the ICR Clinical Trials and Statistics Unit (ICR-CTSU) 9.1 Pre-trial treatment Example - All participants should have a transurethral resection of bladder tumour (TURBT) with completion of bladder tumour map by the urologist performing the procedure. Placement of fiducial markers is recommended either during TURBT or at cystoscopy following neo-adjuvant chemotherapy. 9.2 Treatment timelines Example - Radiotherapy should commence within 6 weeks following randomisation or completion of neoadjuvant chemotherapy (if used), to allow sufficient time for planning. 9.3 Radiotherapy fractionation schedules Example - Two fractionation schedules are permitted: 32 fractions or 20 fractions. Centres will specify their intended fractionation schedule prior to trial initiation and this should be used to treat all trial participants. 9.4 Radiotherapy planning and delivery Details of radiotherapy planning are provided in the accompanying Radiotherapy Planning and Delivery guidelines for this trial, available on the TROG website (insert link). The current version of the radiotherapy planning and delivery guidelines for this trial must be used as the primary source for planning and delivering radiotherapy treatment within the trial. Specify the RT treatment requirements for each arm of the trial, or for the technique being studied. Include basic patient preparation, dose, fractionation, IGRT requirements. See below for examples 9.4.1 Group 1: Standard whole bladder RT (WBRT) (control) Example - Radiotherapy will be delivered to an empty bladder. One treatment plan will be generated from a CT scan. 64Gy/32f or 55Gy/20f RT will be given daily for 6 ½ or 4 weeks. Pre-treatment CBCT should be conducted for treatment verification. 9.4.2 Group 2: Adaptive image guided Tumour focused RT (SART) Example - RT will be given with a partially full bladder. 2 planning CTs will be taken at 30 (CT30) & 60 (CT60) minutes after urination & drinking 350mls water. 2 target volumes will be defined: CTV1 = whole bladder and extravesical spread = CTV of group 1; CTV2= tumour bed i.e gross tumour volume (GTV). CTV1 & CTV2 will be used to create 2 PTVs from which 3 plans will be produced (small, medium & large). If >50mls filling occurs between CT30 & CT60 the large PTV will be defined from outlines derived from CT60. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 19 of 40 PTV1 will be treated to at least 52Gy/32f or 46Gy/20f (+/-5%) & PTV2 to 64Gy/32f or 55Gy/20f. Treatment will be planned using forward planned IMRT, inversed planned IMRT, VMAT or tomotherapy plans. Use of alternative techniques will require specific approval from the RAIDER TMG and QA team. Centres will be asked to specify their preferred method of treatment delivery and complete the appropriate Quality Assurance program. Prior to each fraction, a CBCT will be performed & the optimal plan will be selected for that day’s treatment by an accredited staff member & verified by a second trained individual. 9.4.3 Group 3: Adaptive image guided Dose escalated Tumour boost RT (DART) Example: Plans & treatment delivery technique will be as for group 2. An escalated tumour boost dose (PTV2) of 70Gy/32f or 60Gy/20f will be given. If preset dose constraints are not met for the medium plan participants will be treated as in group 2. 9.5 Treatment scheduling and gaps Example: Treatment can start on any day of the week and should be given five days a week until completion. Delays and treatment gaps should be avoided, however if gaps occur please refer to the radiotherapy planning and delivery guidelines for further information. 9.6 Concomitant therapy Example: Participants in all groups will be permitted to receive concomitant radiosensitising chemotherapy, either the BC2001 MMC/5FU regimen or gemcitabine, carbogen or cisplatin. Any other regimens in standard use at participating centres will require approval by the Trial Management Committee. Centres should aim to use the same regimen for all patients receiving radiosensitising treatment throughout the trial. If the patient isn’t fit for the centre’s usual radiosensitising treatment an alternative may be substituted after discussion with the Trial Chairperson. 9.7 Supportive care guidelines Example:All medication considered necessary for the patients’ welfare and which is not expected to interfere with the evaluation of the treatment may be given at the discretion of the investigator. In the event of patient catheterisation during the course of treatment it is expected that the participant will continue and complete radiotherapy in accordance with their allocated treatment group. For patients in group 1 (WBRT), as the bladder requires emptying prior to treatment delivery, the catheter must be on free flow in circumstances where there is a leg bag or voided in circumstances where there is a flip-valve. For patients in groups 2 & 3 (SART & DART), the catheter should be clamped 30 minutes before treatment (if possible). Participants’ symptoms should be managed according to local practice, although the following are suggestions for patient care: Anaemia: Patients should be maintained by transfusion with haemoglobin above 11 grams. Iron deficiency should be treated with iron supplementation. Dysuria/Frequency: Check for evidence of infection and treat if present with appropriate antibiotics, anticholinergics (eg oxybutynin, tolterodine), NSAIDs, analgesics. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 20 of 40 Diarrhoea: Loperamide or opioid Proctitis: steroid suppository +/- local anaesthetics (e.g. sheriproct, proctosedyl) 9.8 Non-permitted medications/treatments Investigators can prescribe medications/treatments that are deemed necessary for the well-being and overall treatment of the trial participant. The dates and dosage of all prescription and nonprescription medications must be documented in the patient’s medical record and transcribed onto the relevant CRF. In general, alternative and complementary medications are not recommended during radiation treatment until 12 weeks post-radiation completion. Every effort should be made to facilitate smoking cessation in patients who are current smokers in view of the potential adverse impact on treatment outcome and survival. 9.9 Radiotherapy Quality Assurance (QA) A comprehensive QA programme for this trial including pre-trial and on-trial components has been designed by the TROG QA team. Refer to the TROG XX.XX Radiotherapy Planning and Delivery Guidelines available on the TROG website (insert link). TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 21 of 40 10. CHEMOTHERAPY /SURGERY TREATMENT REGIMEN [if applicable] 10.1 Chemotherapy [if applicable] 10.1.1 Treatment Schedule Specify the duration of chemotherapy treatment and the timing limitations to registration/randomisation. If chemotherapy is given concurrently with other protocol treatment, specify which days chemotherapy is given and whether it is administered on the same day as the other treatment. If the timing of the chemotherapy is important, specify that the times when chemotherapy drugs are delivered must be documented on the prescription sheets. 10.1.2 Treatment regimens Specify the treatment regimens. 10.2 Insert name of chemo agent [if applicable] 10.2.1 Premedication – insert name of chemo agent Specify if premedication or an induction phase is prescribed before the beginning of radiotherapy. Specify how long before the chemotherapy treatment, the premedication or induction phase will need to be. 10.2.2 Administration – insert name of chemo agent Specify the dosage of each chemotherapy drug used in the trial and the administration process. 10.2.3 Known Toxicities – insert name of chemo agent Specify known toxicities of each chemotherapy drug used during the trial and at what time these side effects are anticipated to be evident. Specify investigational drug toxicities, if known from phase I and II trials. Toxicity must be described as per CTCAE Version 4.0. 10.2.4 Dose Modifications and Delays - insert name of chemo agent Specify dose modifications using grade levels and descriptions. Specify whether other trial modalities will be delayed at the same time as chemotherapy. Also specify if the second modality should continue if chemotherapy has been permanently discontinued. 10.3 Surgical Therapy [if applicable] 10.3.1 Surgery Details Provide specific detail of the surgery procedures. Provide details of unacceptable deviations. If surgery is performed before registration and/or randomisation, specify the extent of surgery which is required for trial inclusion. It may be that the pathology will be a surrogate for adequate surgery in this situation. Thus the pathology results required will need to be listed. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 22 of 40 Where surgery has not been performed before inclusion in the trial, the researchers will need to be clear what is required for surgical quality control. This needs to be clearly stated with a description of the surgical procedure. The essential requirements need to be clearly stated. Where the complications of a procedure are important parameters, these need to be stated. It may be that an increase of surgical complications above a certain level is not acceptable leading to early cessation. In this case the evidence and percentage of expected complications will need to be stated along with the “stopping rules”. If surgery is performed as part of the protocol: If pre surgery evaluation is needed, provide specific details on the assessments that will need to be performed e.g. history and physical examination, pulmonary function tests and blood tests. Specify if ‘staged surgery’ will be used and the type of staged surgery acceptable. Provide examples of surgery procedures that are not acceptable. Provide details of acceptable surgery procedures for all stages of surgery, e.g. staging procedures, therapeutic procedures and flaps and drainage. Also provide examples of protocol variations and procedures. Specify complete removal of primary lesion with negative gross margins or specify margins for resection, e.g. minimum 2 cm gross or 1 cm microscopic margins. 10.3.2 Treatment Sequencing The timing of surgery must be clearly specified. If surgery is performed before registration, the maximum interval between surgery, registration and/or randomisation and protocol treatment must be stated. If surgery is performed during the protocol treatment, the interval between surgery and the other treatment modality must be stated. If timing between surgery and registration affects eligibility, this must be stated in the eligibility criteria. 10.4 Hormone Therapy [if applicable] 10.4.1 Duration and Administration of Treatment Specify the days that hormone treatment must be given. Specify the duration of hormone treatment. Specify timing with registration/randomisation and radiotherapy. Specify if it is concurrent or sequential treatment. Include information on route of administration of the hormone therapy, e.g. intravenous or tablet form. 10.4.2 Monitoring Toxicity and Modifications Specify blood tests that must be performed before the start of treatment and at other specific time points. Specify modifications based on blood results. Specify how toxicity will be monitored and how modification of hormone therapy will occur. Specify side effects and medications allowed to ease symptoms. 10.4.3 Treatment Sequencing Multimodality treatments - specify any requirements or restrictions for timing between therapeutic modalities. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 23 of 40 10.5 Drug supply, storage, accountability and disposal The Pharmacy Department at the Trial Site will be responsible for ordering the trial medications and ensuring their proper storage. The Pharmacy Department at each Trial Site will maintain a record of drugs dispensed for each patient, including the drug name, batch number, expiry date, amount dispensed and where required, amount destroyed. The destruction of expired (and unused study drugs) will be undertaken in accordance with the Pharmacy’s routine practice for the destruction of biologicals. 10.6 Investigator’s Brochure Check the marketing status of each drug to be used in the trial and the approved indication for each country planning to participate in the trial. Select the most appropriate scenario below and delete remaining. Select the option that provides the most information if there is a difference in approval status for different countries. The investigational product [insert name of drug] is a marketed drug and its pharmacology is widely understood by clinicians. In this trial, [insert name of drug] is used for an approved indication. An Investigator’s Brochure (IB) is therefore not necessary for the purpose of this trial. A product information leaflet including current, comprehensive, and detailed information will be provided and should be filed in the Trial Master File at each Trial Site. OR The investigational product [insert name of drug] is a marketed drug which is being studied in this trial for a new indication. An Investigator’s Brochure (IB) specific to the new indication has been prepared by [insert name of company] who will provide the Trial Coordinating Centre with an adequate number of IBs for distribution to the responsible HREC and all Trial Sites participating in the trial. The IB will be reviewed annually and updated as necessary. 11. PATIENT REPORTED OUTCOMES AND HEALTH ECONOMICS 11.1 Patient Reported Outcome questionnaires The following Patient Reported Outcome (PRO) questionnaires will be used in this trial to assess Quality of Life (QoL) outcomes in accordance with the time points as specified in Section 10: Examples: AQol-8D EORTC QLQC30 (Core Questionnaire) EORTC PR25 (Prostate module) EQ-5D-5L Functional Assessment of Cancer Therapy-Head and Neck (FACT-HN) Hearing handicap inventory for adults, screening version (HHIA-S) TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 24 of 40 Hospital Anxiety and Depression Scale (HADS) M.D. Anderson Symptom Inventory – Head and Neck Module (MDASI-HN) Their content (items and domains), recall period, and scoring are summarised below, with the actual questionnaires included in the appendices. Each questionnaire will be scored according to standard scoring algorithms endorsed by the questionnaire developers. Justify the choice of questionnaires by linking back to the objectives via the key domains. Describe the questionnaire; number of questions, response scale, how it is scored (domain/total score), score range and direction (e.g. higher score = more symptom or higher score = better wellbeing) and an estimate time needed for completion. Provide citations for validity, reliability and responsiveness of the questionnaire Examples: 11.1.1 AQoL-8D The AQoL-8D is a copyrighted Quality of Life (QoL) assessment tool that is a multi-attribute utility health-related QoL instrument and is used in agreement with the Centre for Health Economics at Monash University. The dimensions of this questionnaire include independent living, life satisfaction, mental health, coping, relationships, self worth, pain, and senses. 11.1.2 EORTC QLQ-C30 (Core Questionnaire) The QLQ-C30 is a copyrighted QoL assessment instrument and is used under agreement with the EORTC for the purposes of this project. Refer to the appendices for a copy of this instrument. Information regarding the standardised administration of this instrument for all study participants is provided in the site specific protocol appendices. 11.1.3 EORTC PR25 (Prostate module) The EORTC PR25 is a copyrighted prostate specific QoL assessment instrument used in conjunction with the EORTC QLQ-C30 core questionnaire under agreement with the EORTC for the purposes of this study. 11.1.4 EQ-5D-5L The EQ-5D-5L is a validated, preference-based utility index of HRQOL61. It will contribute to the estimation of QALYs for use in cost-utility analysis and economic evaluation. The EQ-5D-5L is a copyrighted instrument and will be used under agreement with EuroQol. 11.1.5 FACT-HN Module The Functional Assessment of Cancer Therapy-Head and Neck (FACT-HN) module is a 39 item questionnaire that has been validated among patients with head and neck cancer. The FACT-HN is a copyrighted instrument and will be used under agreement with the Functional Assessment of Chronic Illness Therapy (FACIT) organisation for the purposes of this trial. 11.1.6 HHIA-S The HHIA-S is a validated tool for assessing hearing-related QOL45. The HHIA-S contains 10 items (five emotional and five social/situational), selected from the full 25-item HHIA. It does not specify a recall period. For each item, TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 25 of 40 a “yes” response is awarded 4 points and sometimes 2 points, and a "no" 0 points. Scores for the total HHIE-S range from 0 to 40. Higher score values indicate greater perceived handicap and impact of hearing problems. 11.1.7 HADS The HADS is a validated patient self-reported measure of the presence and severity of anxiety and depression. The HADS is a copy righted instrument and will be used under agreement with the GL Education Group (GL Assessment). 11.1.8 MDASI-HN Symptom Inventory The M.D. Anderson Symptom Inventory – Head and Neck Module (MDASI-HN) is a validated questionnaire that directly reflects the perceived impact of adverse disease and treatment-related effects on activities of daily living and perceived distress. The MDASI-HN Inventory is a copyrighted instrument and will be used under agreement with Prof Charles Cleeland, Department of Symptom Research, MD Anderson for the purposes of this trial. 11.2 Non-English Speaking Patients [if applicable] Depending on the eligibility criteria, a study may include participants that cannot read or write English. In this instant one of the following options may be implemented in order to include these participants in the PRO component of the study: The questionnaire may be requested in the appropriate language, for use by the participant. For this option, the following paragraph must be include in the protocol If the questionnaire is not available in the participants language, this will be documented on the Patient Reported Outcome (PRO) Completion and Missing Data (CoMiDa) checklist (see section 11.3 below). 11.3 A professional, accredited interpreter may be used to assist the participant with the completion of the questionnaire. Patient Reported Outcome Completion and Missing Data The Patient Reported Outcome (PRO) Completion and Missing Data (CoMiDa) checklist is a document developed by the Quality of Life Office within the Psycho-oncology Co-operative Research Group (PoCoG) The PRO CoMiDa checklist is a data management tool, designed to provide standardised documentation of the completion or reasons for non-completion of QOL assessments by participants in a clinical trial/study. Such documentation is crucial for quality assurance since missing data are the greatest threat to the integrity and interpretability of QOL data. A PRO CoMiDa checklist has been included in the Case Report Form (CRF) suite for this trial. The person responsible for data collection at the site (i.e. Site Trial Coordinator, Data Manager, Research Nurse, or equivalent) must complete the PRO CoMiDa checklist at each scheduled time point. 11.4 Completion of Patient Reported Outcome questionnaires It is vital that the questionnaires completed within acceptable time limits surrounding the scheduled assessments. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 26 of 40 In order for the [primary / secondary] endpoint to be valid and reliable, the completion rates of QoL forms will be monitored closely by the Trial Coordinating Centre. A completion and return rate of 90% is expected from each Trial Site. In the instance that this rate drops below 90%, the Trial Coordinator will contact the Trial Site to gauge if there is a problem and offer assistance where required. The recommended acceptable time limits for completion of QOL assessments are shown in Table x below; Assessment Time Point Beginning of acceptable time limit End of acceptable time limited Table x: Acceptable submission timeframes for PRO data Specific instructions regarding the administration of PRO questionnaires are provided in the Data Management Manual for this trial. These instructions must be followed to ensure the wellbeing of trial participants and the validity of PRO data. Please contact the Trial Coordinating Centre for further details. 12. TRIAL ADMINISTRATION AND QUALITY ASSURANCE 12.1 Participating Centres Before activating the trial, participating sites are required to sign an agreement accepting responsibility for all trial activity which takes place within their site. Sites may commence recruitment once the site agreement has been signed by all required signatories, the required trial documentation is in place (as specified by TROG) and a site initiation (visit or teleconference) has taken place. 12.2 Investigator Training Each centre will complete quality assurance procedures, as described in the TROG XX.XX Radiotherapy Planning and Delivery Guidelines (insert link), prior to commencing recruitment. The quality assurance programme will continue throughout the trial, with investigator training as required. 12.3 Data acquisition Case Report Forms (CRF) will be used for the collection of trial data. TROG will provide guidance to sites to aid the completion of the CRFs. The Trial Management Committee reserves the right to amend or add to the CRF template suite as appropriate. Such changes do not constitute a protocol amendment, and revised or additional forms should be used by sites in accordance with the guidelines provided by TROG. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 27 of 40 12.4 Site Visits If a monitoring visit is required, TROG will contact the site to arrange the visit. Once a date has been confirmed, the site should ensure that full patient notes of participants selected for source data verification are available for monitoring. TROG staff conducting on-site monitoring will review essential documentation and carry out source data verification to confirm compliance with the clinical trial agreement and trial protocol. If any problems are detected during the course of the monitoring visit, TROG will work with the Principal Investigator or delegated individual to resolve issues and determine appropriate action. 12.5 Completion of the study and definition of study end date The study end date is deemed to be the date of last data capture. 12.6 Archiving Essential trial documents and source documentation (including medical histories, radiological imaging, laboratory tests, chemotherapy and radiotherapy treatment records, verification films and portal images) , must be retained for 15 years after completion of the trial in accordance with ICH GCP Guidelines. Documents should be securely stored and access restricted to authorised personnel. 12.7 Quality Assurance reviews The following information is for guidance only and must be adapted as per the Quality Assurance requirements for each trial. 12.7.1 Regulatory Reviews The Trial Coordinating Centre will be responsible for collecting, maintaining and monitoring all required essential documentation from the Trial Site before, during and after the conduct of the trial. 12.7.2 Eligibility Reviews 12.7.2.1 Pathology Reviews There will be central review of all pathology reports to confirm eligibility. 12.7.2.2 Informed Consent and Other Eligibility Reviews Reviews of de-identified consent forms will be performed for all cases to determine that Informed Consent was obtained before registration on the trial. Throughout the trial, copies of relevant documents (such as participant diaries, clinical history notes, pathology/histology reports, imaging reports, blood test results, dental assessment reports, etc. may be requested for source data verification. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 28 of 40 12.7.3 Chemotherapy reviews [if applicable] For each participant, a checklist of information required for chemotherapy review (i.e. treatment charts/‘flow sheets‘) which clearly demonstrate the prescription and administration of chemotherapy drugs will be provided by the TROG QA Office. Review material will be required at the end of treatment. CRFs and the copies of chemotherapy records will be reviewed for each participant to assess and verify compliance with the protocol. Audits will focus on delivered dose, method of administration, treatment timing and dose modifications. 12.7.4 Surgery reviews [if applicable] For each participant, the TROG QA Office will request relevant information after the completion of protocol treatment. In general, adherence to pathology criteria and timing will be audited. 12.7.5 Loco-regional failure reviews [if applicable] All cases of LRF will be reviewed by designated review radiation oncologists and the TROG QA Office. Reviewers will require the following additional information: 13. Diagnostic images and report (failure site/s) FNA cytology or biopsy report (failure site/s) ADVERSE EVENT SCORING AND REPORTING It is important that Adverse Events (AEs) are monitored in the interest of participant safety. The investigator at each trial site is responsible for assessing and reporting AEs as part of routine clinical care and data collection. A subset of AEs will be classified as ‘serious’ and will require expedited reporting. 13.1 Adverse Event An adverse event is defined as any untoward medical occurrence the participant which does not necessarily have to have a causal relationship with the study treatment. An AE can therefore be any unfavourable and unintended sign (including any abnormal laboratory finding, for example), symptom, or disease temporally associated with the use of a medicinal product, whether or not considered to be related to the product. 13.2 Serious Adverse Event (SAE) Adverse events and adverse drug reactions are considered ‘serious’ if they threaten life or function. Due to the significant information they provide, Serious Adverse Events require expedited reporting. SAEs are defined as any adverse event or adverse drug reaction which: TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 29 of 40 • • • • • • Results in death Is life-threatening (an event in which the participant was immediately at risk of death at the time of event) Requires in-patient hospitalisation or prolongation of existing hospitalisation Results in persistent or significant disability/incapacity Is a congenital anomaly/birth defect Important medical event (events may be considered a serious adverse experience if they require medical or surgical intervention to prevent one of the listed definitions, e.g. an ‘allergic bronchospasm’ which required intensive treatment in an emergency room or at home) An event will not be considered to a SAE if: • • • • • • • 13.3 Hospitalisation is due to administration of trial procedures Hospitalisation is due to placement of a permanent intravenous catheter Hospice placement for terminal care is required Hospitalisation is due to pre-trial scheduled elective surgery Out-patient hospitalisation for procedures such as: o Elective day surgery o Convenience purposes (e.g. transportation difficulties) Death is due to cancer (this is considered ‘expected’ and is therefore not a SAE) Any new cancer is diagnosed (this is to be reported on relevant CRF) Adverse Event reporting All AE and SAEs are to be graded according to The National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 (appendix 4) by a study investigator. Figure 1 describes the reporting mechanism for Adverse Events and Serious Adverse Events required from the Principal Investigator at the Trial Site and the Trial Coordinating Centre. 13.4 Other situations requiring expedited reporting 13.4.1 Overdoses Overdoses (drug or radiation) must be reported to the TCC and TCOO if the event(s) associated with the overdose meet the SAE definitions. If no serious adverse events are experienced the overdose must be reported in the participants medical record and transcribed onto the relevant trial CRF. 13.4.2 New Cancers The development of new cancers at any time during the trial must be reported in the participants’ medical record and transcribed onto the relevant trial CRF. If any events associated with the new cancer meet the SAE definitions, then they should also be reported to the TCC and TCOO. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 30 of 40 13.4.3 Therapeutical Device Incidents [if applicable] All serious and unexpected adverse device events, i.e. suspected problems with a therapeutic device which has or may present a health hazard (including deficiencies in labelling, instructions or packaging, defective components, performance failures, poor construction or design) must be reported to the Australian and New Zealand Medical Device Incident Report Investigation Scheme (IRIS) using the Medical Device Incident Report Form. http://www.immune.com/rubber/AustraliaNewZealand.pdf Note: The manufacturer, TCOO and the TCC must all be included in the reporting chain of responsibilities. The order of reporting (including who will report to IRIS) will need to be determined and included in the protocol according to the individual requirement of the trial. The timelines should be the same as those specified for Serious ADR reporting. 13.5 New Zealand reporting requirements [if applicable] New Zealand Principal Investigators must follow the Australian reporting requirements outlined in section 16.1 and Figure 1. All Unexpected Serious ADRs will need to be reported to the Centre for Adverse Reactions Monitoring (CARM), rather than the TGA, by using the Adverse Reaction Reporting Card. An electronic version of this card is available at: http://www.medsafe.govt.nz/downloads/ADRMedicines.doc. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 31 of 40 Figure 1: TROG XX.XX [Acronym] Adverse Event Pathways Trial Site to complete Key ADVERSE EVENT (AE) DETECTED at Trial Site between [start point] and [finish time point] Trial Coordinating Centre to complete Final Responsibilities ADVERSE EVENT Not Serious Principal or Co-Investigator to DETERMINE AE SERIOUSNESS Investigator to Grade AE according to CTCAE SERIOUS ADVERSE EVENT (SAE) (report between start and stop point) Serious Principal or co-Investigator to ascertain cause of SAE and determine if it is expected Unexpected Treatment suspected as cause (Suspected Unexpected Serious Adverse Reaction - SUSAR) Investigator to document event & grade in medical records Other suspected cause Complete SAE form and fax within Delegate to transcribe AE information to relevant toxicity CRF and submit to TCC TCC to notify Trial Chair and/or Clinical Reviewer for an immediate review of SAE Expected 24 hrs of notification to the [trial name] Trial Coordinating Centre on [fax no] or email [email –if applicable] If a SUSAR, TCC to report to relevant bodies within reporting timelines Not a SUSAR If initial report is only partially completed, the complete report must be sent by trial site within the next 10 days. Data entered onto trial database by the TCC Add SAE to tracking log and send out ‘Addition Notifications’ (if applicable) e.g. Investigator letters or amend the protocol. Unresolvable AE/SAE DATA REPORTED by; 1. Trial Site to HREC and RGO as appropriate 2. Trial Coordinating Centre to Independent Data Safety Monitoring Committee (IDSMC) and to other relevant bodies as appropriate (e.g. safety reports/line listings) 3. IDSMC to Trial Management Committee and TROG Scientific Committee TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Event ongoing Event resolved Page 32 of 40 Trial Site to submit updated FU SAE reports until event resolved (with/without sequelae) or death has occurred. 14. STATISTICAL CONSIDERATIONS 14.1 Sample Size Calculation Provide the estimated number of participants needed to achieve study objectives and how it was determined, including clinical and statistical assumptions supporting any sample size calculations. The planned number of trial participants is a key aspect of study design, budgeting, and feasibility and is usually determined using a formal sample size calculation. If the planned sample size is not derived statistically, then this should be explicitly stated along with a rationale for the intended sample size Refer to TROG Policy Statement TPSE5 Statistical Guidelines for instructions on calculating the sample size 14.2 Sequence Generation For a randomised trial, state: The allocation ratio. The method of randomised allocation (e.g. balanced block/adaptive biased coin; minimisation; stratification). State whether treatment assignments are to be determined from pre-prepared randomisation charts or from using a dynamic (real-time) computer-based allocation system. Do not give details of the randomisation method if this might increase the ability to predict the next treatment assignment. If applicable, whether or not participants, those administering the trial treatment, and those assessing the outcomes are blinded to group assignment. Maintenance of treatment randomisation codes and procedures for breaking codes, including: - That the assignment schedule is locked away from even the person who generated it. Where the allocation list will be stored. State that the next treatment to be assigned will not be known by any person prior to eligibility criteria being established and the intention to randomise the patient being declared. State that once a patient is registered on a trial registration will not be cancelled. 14.3 Endpoint Definitions All endpoints, whether primary or secondary, must be completely defined in this section and, where applicable, standard definitions adhered to. 14.4 Measurement of response Baseline tumour measurements must be undertaken prior to any protocol treatment commencing. All tumour measurements must be recorded using the definitions of measurable/non-measurable disease provided below. The initial assessment of response will be determined after all protocol treatment has been completed, whether or not all of the planned treatment was received. The [insert criteria plus reference e.g. RECIST (Response Evaluation Criteria in Solid Tumours)] criteria must be used for assessment of tumour response. 14.4.1 Definition of Measurable/Non-Measurable Disease TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 33 of 40 Define as required for the disease site, for example: Measurable disease: tumour that can be accurately measurable as ≥2.0 cm (or ≥1.0 cm with spiral CT scan) in at least one dimension. The longest diameter is recorded as the tumour measurement. Non-Measurable Disease: all other known tumour sites, including those with a longest diameter <2.0 cm (or <1.0 cm with spiral CT scan) 14.4.2 Definition of Response 14.5 Statistical Analysis Plan In this section, provide: 14.6 Definition of the close-out date (for time-to-event endpoints). (A number of definitions exist, and may differ by endpoint.) Detailed method of analysis of the primary objective, including whether the main analysis will be unadjusted or will adjust for stated prognostic factors; Statement of the intention-to-treat principle, if applicable, and that it will be used for the primary analysis. When this will occur: e.g. at a fixed time following the end of accrual or once a given number of primary endpoint events have occurred General statistical tests to be used (e.g., Kaplan-Meier curves, Greenwood estimates, logrank test, Cox regression, cumulative incidence curves); and general statistical methods: e.g., 95% CI, 2-sided p-values, alpha=0.05; strategy for handling multiple comparisons. Describe analyses to check assumptions of the methods and the data transformations to be used. Methods of analysis of the secondary and exploratory objectives; these need not be as detailed as for the primary analysis. Interim analyses and early termination criteria State when interim analyses are planned to be done, or what criteria trigger them including those, where applicable, for efficacy, safety, futility, reassessment of sample size General statistical tests to be used (e.g., Kaplan-Meier curves, Greenwood estimates, logrank test, Cox regression, cumulative incidence curves); and general statistical methods: e.g., 95% CI, 2-sided p-values, alpha=0.05; strategy for handling multiple comparisons. Describe analyses to check assumptions of the methods and the data transformations to be used. Specify criteria that may cause the trial to be terminated before the planned target accrual such as: o Early evidence of efficacy (or lack of such) o Safety issues o Inadequate realisation of trial resources, including participant numbers o Diminished significance of the trial question The IDSMC will review confidential reports of relevant analyses of trial data and will use specified statistical criteria to guide its assessment of whether the trial should be stopped or undergo modification or continue without change. 14.7 Secondary Analysis of the Data TROG Policy Statement E12 Secondary Analyses in TROG Clinical Trials outlines when secondary analysis of the trial data is allowable. The data is only be used for a secondary analysis once the Trial TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 34 of 40 TMC and/or Chair, TSC and HREC have given approval to the new project/protocol. Participant consent for use of the data will only be sort if it is a requirement of the HREC. 15. RESEARCH GOVERNANCE 15.1 Sponsor and Funder This trial is sponsored by the Trans Tasman Radiation Oncology Group (TROG) and funded by [or ‘funding is being sought from’] xx. This funding source will have no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, or decision to submit results. As the sponsor of this trial, TROG requires that all TROG Policy Statements regarding the study design; collection, management, analysis, interpretation of data, writing of the report and publications are adhered to by the Trial Chairperson. 15.2 Trial Chairperson The Trial Chairperson will have overall responsibility for the design and conduct of the trial according to TROG Policy Statements. Further details regarding the responsibilities and delegations are set out in the Clinical Trial Agreement between TROG and the Trial Chairperson. 15.3 Trial Management Committee The Trial Management Committee (TMC) will be responsible for monitoring of the progress of the trial, decision making, education and information services and reporting as described in TROG Policy Statement TPS E8 Trial Management Committee Responsibilities. TMC members are listed at the beginning of the protocol. 15.4 Independent Data Safety Monitoring Committee An Independent Data Safety Monitoring Committee (IDSMC), separate to the TMC, will independently monitor the conduct of the trial in order to ensure its ethical and scientific integrity. The roles and responsibilities of the IDSMC are set out in TROG Policy Statement TPS E9 Data Monitoring Committee Guidelines and throughout this protocol document. If the members are not yet known, the protocol can indicate the intended size and characteristics of the membership until further details are available. 15.5 Principal Investigator In each participating centre a Principal Investigator (Radiation Oncologist) will be identified, and will be responsible for identification, recruitment, data collection and completion of CRFs along with follow up of study patients and adherence to the study protocol. Each Principal Investigator will be a full member of TROG and adhere to TROG Policy Statements. One investigator per country will be nominated as national coordinator and one investigator per ethics jurisdiction within Australia and within New Zealand will be nominated as Lead Ethics Coordinator. Further details regarding the TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 35 of 40 responsibilities and delegations are set out in the Clinical Trial Agreement between TROG and the participating centre. 15.6 Consumer Representative TROG encourages wider participation from consumer representatives’, as defined by the Statement on Consumer and Community Participation in Health and Medical Research, and supports the recommendation that consumers are involved in decision making throughout the development, conduct and close out phases of a trial. 16. PATIENT PROTECTION AND ETHICAL CONSIDERATIONS 16.1 Ethical Principles and Regulatory Compliance This trial will be conducted according to the approved protocol and its amendments, supplementary guidance and manuals supplied by the Sponsor and in accordance with relevant national guidelines. [If applicable] A Clinical Trials Notification (CTN) form must be submitted to the responsible HREC and returned to the Trial Coordinating Centre on approval. It is the responsibility of the investigator to not enter participants onto the trial before CTN acknowledgment is received from the Therapeutic Goods Administration of Australia. 16.2 Adherence to Protocol Except for an emergency situation in which proper care for the protection, safety and wellbeing of the trial participant requires that an alternative treatment be used, the trial shall be conducted exactly as per the terms and instructions described in the approved protocol. No protocol exceptions, waivers or exemptions will be granted. If the protocol constraints cannot be met then the participant should be treated off trial. 16.3 Aboriginal and Torres Strait Islander values and principles TROG recognises and commits to the respect of Aboriginal and Torres Strait Islander cultural values and principles. Although this trial is not targeted specifically to Aboriginal and Torres Strait Islander peoples, a person from one of these communities may be invited to participate if they meet the eligibility criteria of this trial. This decision will be at the discretion of the Principal Investigator at the Trial Site who shall consent and treat the participant according to the principles set forth in the Guidelines for Ethical Conduct in Aboriginal and Torres Strait Islander Health Research and any specific requirements of the approving Human Research Ethics Committee. 16.4 Confidentiality The trial will be conducted in accordance with applicable Privacy Acts and Regulations. All information regarding trial participants must be treated in strict confidence. Data, which identify any TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 36 of 40 trial participant, must not be revealed to anyone not directly involved in the trial or the clinical care of that participant. An exception is where the trial participant has provided written consent for his/her records to be included in source document verification. In this instance, the records may be inspected by (a) a representative of TROG for the purposes of source document verification or quality audit as stipulated in the ICH GCP Guidelines, or (b) a representative of a government regulatory authority for the purposes of official inspection. Records must be made available for inspection on the understanding that all information relating to trial participants will be treated in strict professional confidence. 16.5 Concealment Mechanism [If applicable] Participants will be randomised through a GCP compliant, programmable purposedesigned data management system. Allocation concealment is ensured, as the trial database will not release the randomisation code until the participant has been recruited to the trial after all baseline measurements have been completed and Case Report Forms submitted. 16.6 Security and Back up of Data All original CRFs related to study data will be kept in locked cabinets at trial site and the Trial Coordinating Centre. Access to the study data will be restricted to trial staff. In addition, Site Trial Coordinators will only have access to their own centre’s data. At the Trial Coordinating Centre a password system will be utilised to control access to CTDS and only those staff members who will be working on this study will be allocated access to this trial within CTDS. All reports prepared will be prepared such that no individual subject can be identified. An independent external back-up and disaster recovery system that ‘mirror replicates’ a copy of all data saved in real-time is in place at the TROG Central Operations Office. The back-up server is located off-site in a climate-controlled facility and will be retained indefinitely. 16.7 Insurance and Compensation TROG endorses the principles of the Medicines Australia Guidelines for Compensation for Injury Resulting from Participation in a Company Sponsored Trial and the Research Medicines Industry equivalent in New Zealand. To provide protection for trial participants involved in TROG Clinical Trials, TROG maintains a clinical trials insurance policy. 17. PUBLICATION AND PRESENTATION POLICY The Trial Chair and TMC are responsible for presentations and publications arising from this trial with the TROG Publications Committee providing oversight and independent scientific review of all relevant material prior to submission. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 37 of 40 Refer to TROG Policy Statement TPS E10 Authorship, Publication and Spokesmanship for detailed information and responsibilities of both committees. 18. REFERENCES The Vancouver (author-number) style of referencing is to be used in all TROG trials. Examples are available at http://www.nlm.nih.gov/bsd/uniform_requirements.html. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 38 of 40 APPENDICES Suggested Appendices Disease specific TNM criteria o ECOG Performance status criteria o Available at: o o AQol-8D EORTC QLQC30 EORTC PR25 EQ-5D-5L Permission to use must be sought for each questionnaire and copyright information must be included. Response Evaluation Criteria in Solid Tumours (RECIST) 1.1 Criteria o Available at: http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev4.pdf As published by the U.S Department of Health and Human Services, National Institutes of Health National Cancer Institute: May 28, 2009 Patient Reported Outcome Quality of Life Tools (PRO QoL) such as o o o o o http://www.mdcalc.com/creatinine-clearance-cockcroft-gault-equation/ As published in Nephron Journals:Cockcroft DW, Gault MH: Prediction of Creatinine Clearance from Serum Creatinine. Nephron 1976;16:31-41 (DOI: 10.1159/000180580) CTCAE (Common Terminology Criteria for Adverse Events, V4.0) o http://www.npcrc.org/usr_doc/adhoc/functionalstatus/ECOG%20Performance%20Statu s.pdf As published in Am. J. Clin. Oncol.: Oken, M.M., Creech, R.H., Tormey, D.C., Horton, J., Davis, T.E., McFadden, E.T., Carbone, P.P.: Toxicity And Response Criteria Of The Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649-655, 1982. Cockcroft-Gault Formula for Calculating Creatinine Clearance o Available at: o 7th Edition available at http://www.cancerstaging.org/products/ajccproducts.html Available at: http://www.recist.com/ Radiotherapy Contouring Guidelines including pictorial representations of target volumes Participant Information Sheet and Consent Form ((including Consent Form for Tissue Sample Storage And Use - if applicable) o o NOTE: The template Participant Information Sheet and Consent Form should be a separate document to the protocol so that when changes occur the entire protocol does not need to be submitted for HREC approval. The format of the PIC and instructions for the content will depend on the ethics committee undertaking the review and the state in which they are located. See following websites for examples: http://www.health.vic.gov.au/clinicaltrials/application-instructions.htm (for everything) http://www0.health.nsw.gov.au/policies/gl/2007/GL2007_016.html (PIC) TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 39 of 40 o TROG specific information to add into the trial PIC is as follows; 1. What happens when the research project ends? Once the study has finished, it is likely your doctors will still ask you to attend follow up visits to confirm that you remain well. OR You will continue to be followed by your doctor with regular CT scans as is normally the case for patients who are monitored following treatment for XXXXXX cancer. If you cancer recurs, it will be treated by the most appropriate standard methods. 2. What will happen with the results of the study? It may be a number of years before the results of this research are available. When the results are available they will be published as ‘journal articles’ in medical journals. A summary of the trial results will also be available via the TROG website (www.trog.com.au) and in the TROG Community Newsletter. Your identity will not be revealed in these publications. Please ask your doctor if you want to know more about this. 3. Compensation: This study is sponsored and coordinated by the Trans Tasman Radiation Oncology Group (TROG), a not-for-profit research group involving many cancer researchers in Australia and New Zealand, as well as internationally. If you suffer any injuries or complications that may be as a result of your participation in this study, you should immediately contact your doctor, who will assist you in arranging appropriate medical treatment. If you are eligible for Medicare, you can receive any medical treatment required to treat the injury or complication, free of charge, as a public patient in any Australian public hospital. In the unlikely event of an injury caused by your participation in this study, compensation may be payable to you. TROG maintains a clinical trials insurance policy. Please ask your doctor if you would like more information on this policy. 4. Who is organising and funding the research? This research study is being conducted and sponsored by the Trans Tasman Radiation Oncology Group (TROG) and funding is being sought through participating Radiotherapy Centres and competitive grants. TROG Protocol Template Version 4, 03 November 2014 (TROG XX.XX) [Insert acronym]; Final protocol: [insert date] Page 40 of 40