Case study Comparative study of risk factors of SSI following spinal
advertisement

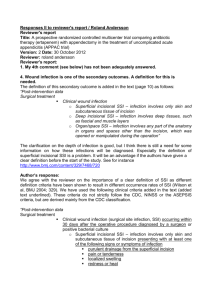
Case study Comparative study of risk factors of SSI following spinal fusion in two cases. Introduction: SSIs are divided into the categories of superficial incisional SSI, deep incisional SSI, and organ/space SSI. Superficial incisional SSIs involve only the subcutaneous space, between the skin and underlying muscular fascia, occur within 30 days of the index opera and are documented with at least 1 of the following findings: (1) purulent incisional drainage; (2) positive results of culture of aseptically obtained fluid or tissue from the superficial wound; (3) local signs and symptoms of pain or tenderness, swelling, and erythema, with the incision opened by the surgeon (unless culture results are negative); or (4) diagnosis of SSI by the attending surgeon or physician. A deep incisional infection involves the deep layers of soft tissue (e.g., fascia and muscle) in the incision and occurs within 30 days after the operation or within 1 year after the operation if a prosthesis was inserted and has the same findings as described for a superficial incisional SSI. At least one of the following criteria: Purulent drainage from the incision but not from the organ/space of the surgical site A deep incision spontaneously dehisces or is deliberately opened by a surgeon when the patient has at least one of the following signs or symptoms - fever (>38°C), localized pain or tenderness - unless the culture is negative An abscess or other evidence of infection involving the incision is found on direct examination or by histopathology or radiological examination diagnosis of a deep incisional SSI by a surgeon or attending physician. An organ/space SSI has the same time constraints and evidence for infection as a deep incisional SSI and involves any part of the anatomy (organs or spaces) other than the incision opened during the operation.Any deep SSI that does not resolve in the expected manner after treatment should be investigated as a possible superficial manifestation of a deeper organ/space infection. Literature review showed the following flow chart with factors leading to SSI which are observed in this study. Results and discussion: Patient factors in Case 1 and Case 2 Non modifiable Case -1 Case-2 Advanced Age 77yrs 68yrs Development delay NA NA Immunosupression No No Spinal trauma NO NO Diabetes YES 203-300 HbA1c -7.3 YES Hba1c -5.9 >200 Perioperative-161-179 122-157 No urea/creatinine raised rheumatoid arthritis , low CD4 counts cancer patients on chemotherapy Radiotherapy Chronic Renal failure High rates of infection have been observed in elderly patients and spine trauma patients. Insensate patients with spinal dysraphism and developmental delay undergoing scoliosis surgery have also been found to have higher rates of postoperative infection. Operating through previously irradiated tissue or previously operated tissue has also shown an increased risk for surgical site infection. Diabetes mellitus, especially when it is uncontrolled with blood glucose levels greater than 200 mg/dL is shown to impede chemo taxis and phagocytosis, hence diminishing immune response to bacteria/infections Modifiable Case 1 Case-2 Obesity BMI 23 WT58 HEIGHT 159.5CM BMI 25 HEIGHT162CM Smoking/Alcoholism No no Indwelling catheter Yes Yes( recatheterisation) Extended hospitalization Yes(3days) No Malnutrition Hb 13gm Albumin 3.9(6.7) HB-10.1gm 1.8(4.8) L 27.3% WT-65 albumin- L3.8% Biophysical alterations in obesity and technical issues with surgery. Tissue dissection in these patients can be extensive. Wide retraction and use of electro cautery can lead to fat necrosis and large devitalized areas promoting bacterial proliferation. Klein and Garfin reported preoperative malnourishment in 25% of 114 patients undergoing elective lumbar fusion and 11 of 13 reported complications in this series occurred in this malnourished group. Paradoxically, obesity also can be a risk factor for malnutrition, especially in those patients undergoing rapid weight reduction. Malnutrition, objectively defined by a serum albumin level <3.5 g/dL, a total lymphocyte count less than 1,500 to 2,000 cells/mm3 and a serum transferrin level of 150 μg/dL is another documented risk factor. Most surgeons will attempt to address modifiable factors preoperatively to minimize the risk of postoperative infection. Patients should be counseled to quit smoking both for reducing risk of infection and preventing pseudarthrosis. All active infections should be identified and treated before undertaking elective spine surgery Systemic conditions such as diabetes, rheumatoid arthritis, HIV, and malnutrition should be optimized preoperatively. Furthermore, patients with a prolonged hospital course may be considered for discharge and return as a same-day admission for elective spinal surgery to minimize nosocomial/iatrogenic infections. Surgical factors in case 1 and case 2: Keller and Pappas reported a dramatic decrease in infection rates from 2.7% to 0% with the use of preoperative prophylactic antibiotics. Infection rates after lumbar diskectomies dropped from 9.3% to 1% with the use of preoperative antibiotics. Another study showed that infection rates were significantly lower (4.3%) in patients treated with preoperative antibiotics vs those treated with placebo (12.7%) before undergoing clean lumbar surgery. Surgical Factors Case1 Case 2 Preoperative infection Negative HCV+ local/ Systemic Prophylactic Antibiotics Supacef 750mg Surgery classification L2 to S1 transpedicular screw and rod fixation and L2 to L5 laminectomy L2 to S1 Trans pedicular screw and rod fixation, L3-L5 Laminectomy Clean clean Short segment fusion Short segment fusion Implant Medtronics M8 spinal system Medtronics M8 spinal system Sterilization Implant sticker Implant sticker Duration of surgery >2hours 61/2 hours 5hours Electro cautery/Retraction Used Used Bone graft /Tessel glue No Yes Romovac drain malfunction No Yes Hematoma No Yes Complexity of surgery Yes Yes Intraoperative CF leak No Yes Osteoporosis Osteoporosis of high risk of fracture Radiology suggestive osteoporosis/ Vit- D-31 H/O of postoperative wound drainage Before discharge No Yes Suture material/Re-exploration Vicryl / Ethel one/no Vicryl/ Ethel one/ vicryl sutures were removed Inspection of the postoperative period Regular healthy Regular healthy Diagnosis of SSI wound 1.5gm Amikacin Follow up OPD visit Attending neurosurgeon Case 1 Bone densitometry-Osteoporosis of high risk for fracture. by Magnex 1gm Follow up OPD Visit attending neurosurgeon of by Radiology evidence of disease/Surgery • Short Segment Fusion Indications • Cobb’s angle • Sagittal imbalance • Coronal imbalance • Lordosis • Rigid fixation is doubtful as bone are osteoporotic. Fusion without instrumentation has been associated with infection rates from 0.4% to 4.3%. The use of internal fixation raises the risk significantly (6.6–8.7%) . Several theories attempt to explain this increase likelihood of infection. It is suggested that instrumentation can cause local soft tissue irritation leading to inflammation and seroma formation with subsequent infection. The implants provide an avascular surface for bacteria to lay down a glycocalyx, which in turn protects them from antibiotic penetration. Finally, metallosis from micromotion of the instrumentation leads to granuloma formation and yet another medium for bacterial colonization Long segment fusion has higher immediate postoperative complication s than short segment fusion. Case 2 Short Segment Fusion Indications are Cobb’s angle,Saggittal imbalance,Coronal imbalance,Lordosis Right L4 pedicle could not be tapped due to being narrow and breach of medial wall (few drops of CSF seen coming – controlled by waxing of entry point may be additional factor. Radiology evidence of disease/surgery Rigid fixation as no evidence of osteoporosis. Anaesthetic factors of SSI in case 1 and case 2. Factors Case 1 Case2 Pain Low back ache ,Pain radiating to B/L lower limb. Low backache ,Left lower limb radicular pain History of neck and left shoulder pain. VAS-6/10,Discharged VAS 3/10 VAS 6/10, Discharged VAS3/10 Crocin pain relief (Gabapentin stopped) Combination analgesia Perioperative 250mg Perioperative Fentanyl 250 mcg Fentanyl Perfalgan 1gm Perfalgan 1GM Normovolumic/ hypovolemic Blood transfusion Normovolumic ?Hypovolemic Urine output -460ml Urine Output 280ml 1Autologous (1200ML) 1PRBC(300ML) 1PRBC Hb-9.2-8.4 Hb 11.6-8.6-8.5 Peroperative temperature body 35 degree F No record FIO2 100-0.45-0.5 0.5-0.5 Tissue perfusion(MAP at 4 hour of surgery) >70 mm Hg >70 mm Hg Clinical presentation of SSI. Worsening pain 1 to 4 weeks after a spinal procedure is the most common symptom suggestive of infection . Pain may or may not follow a period of initial relief. The patients often confuse this pain as a recurrence of their original back pain, thus confusing the diagnosis with that of a mechanical cause. The back pain is generally out of proportion to the physical findings and may be referred to the buttock, thigh, leg, groin, perineum, or abdomen Constitutional symptoms have also been reported but are less common than pain. A floridly septic picture with high fevers, chills, and sweats is a rare, but dramatic, presentation In the setting of superficial infections, local wound changes, such as erythema or drainage, may be present . Persistent progressive pain is once again the hallmark of a developing infection. Occasional drainage is noted and frank sepsis is uncommon. The patients, however, may complain of malaise and night sweats. Significant pain with lumbar range of motion is the sine qua non for post procedural diskitis. The incision is usually unremarkable, and in fact, less than 10% of surgical incisions show signs of purulent infection with erythema, drainage, or dehiscence. The presence of a neurological deficit (motor/sensory involvement or bowel/bladder changes) should raise the suspicion for an epidural abscess. Sixteen percent of epidural abscess are postoperative complications. Clinical presentation Case 1 Case 2 Yes Yes Postoperative wound drainage within one week No Yes Postoperative fever/Malaise with 1 week of postoperative period yes Yes Postoperative confusion No Yes Preop weakness present Nil Benign appearing wound Yes Yes Significant postoperative Drainage beyond 1st postoperative week Serous Purulent Dermal necrosis/ Ecthyma gangrenosum No Yes Postoperative pain/Neuralgic pain back neurological Investigations The white blood cell (WBC) count may, or may not, be elevated, depending on host and pathogen factors. Thus, this parameter is unreliable, when used in isolation, for the diagnosis of infection. Less than 50% of the cases of infective spondylodiskitis had an elevated WBC count according to a recent report. The ESR alone is not very specific for infection, Relatively sensitive marker for an inflammatory process and can be reliably followed during the treatment course of a patient to assist with clinical decision making such as cessation of antibiotics. In the setting of infection, the ESR is 78% to 82% sensitive and 38% to 62% specific as a laboratory marker. When interpreting ESR values, it is paramount to understand that the ESR is routinely elevated in the first 1 or 2 weeks after a procedure/operation of the spine. Several authors have attempted to delineate the ESR trend in the postoperative period. Kapp and Sybers reported that the ESR was rarely elevated greater than 25 mm/h and that it generally returned to baseline by the third week of an uncomplicated spine surgery. Jonsson et al ( reported a higher postoperative peak in ESR in more extensive spine procedures (102 mm/h) compared with the limited procedures (75 mm/h). Case 1 Case2 CBC HB9.2,TLC5800-8600 Hb7-9TLC 9600(13000) ESR NO NO CRP NO 18.025 very high Procalcitonin NO 2.71 high risk of sepsis Wound swab culture No growth E-coli/Enterococcus faecalis Furthermore, they reported that the ESR peaked on the fourth postoperative day and returned to baseline after 2 weeks in most patients. A study conducted by Thelander and Larsson showed an even longer postoperative period (6 weeks) during which the ESR was elevated. In light of these data, the ESR is not thought to be useful as a definitive marker for infection. CRP, an acute-phase reactant, is possibly the most sensitive indicator of postoperative infection Both, CRP elevation and its return to baseline after surgery are more rapid compared with the ESR values. CRP levels usually peak on the second or third postoperative day and normalize within 2 weeks after surgery/procedure. A rise in CRP values after the aforementioned timeframe correlates highly with the presence of an infection. Some authors recommend obtaining preoperative ESR and CRP values as a baseline for comparison with postoperative measurements. In the future, other laboratory markers such as interleukin-6 (IL-6) may provide us with the most accurate and reliable means of diagnosing surgical site infection Postoperative Radiology: Plain radiographs are the first imaging modality, there are no changes in the first 3 weeks. In cases of diskitis, disk space narrowing and endplate changes are the earliest findings, seen from the fourth to the sixth postoperative week. Paravertebral soft tissue shadows may be visible on plain films and might signify a paravertebral abscess. Plain radiographs are also helpful in inspecting surgical implants. Lysis around the implants (suggestive of loosening) and overall alignment can be readily assessed from the x-rays. Computed tomography (CT) scans show areas of early bony destruction and soft tissue collections with better anatomical detail than plain radiographs. Similar to plain films, early changes include that of erosive and destructive changes at the endplates and disk space narrowing .The image quality and the level of detail may be compromised in the presence of instrumentation-related scatter/artifact, particularly if stainless steel implants were used. CT guidance can also be used to obtain a tissue biopsy of postoperative diskitis/osteomyelitis or needle aspiration of pus from abscess cavities to provide a microbiological diagnosis.The specimens should be sent for Gram stain and cultures to identify the organism and its susceptibilities before starting antimicrobial therapy. Nuclear medicine studies have been used as part of the diagnostic workup of spinal infections, but usually show nonspecific increased uptake in the majority of cases. Gallium 67 often identifies the presence of a postoperative disk space infection earlier than techne-tium-99m scans or plain films.The results are less accurate and predictive than they are for appendicular infections. A sequential technetium-99m study followed by a gallium-67 study increases the cumulative accuracy of these studies Indium 111-labeled WBC scans may also be useful in establishing the diagnosis but are infrequently used secondary to suboptimal specificity. Magnetic resonance imaging (MRI) with gadolinium enhancement is the imaging modality of choice to delineate post procedural spine infections. MRI is shown to have the highest sensitivity and specificity in the diagnosis of post procedural diskitis, superior to both technetium-99 and gallium-67 scans reported sensitivity of 93% and a specificity of 97%. ), contrast enhancement of the disk space/ paraspinal tissues in the absence of Modic I changes is suggestive of infection when comparing MRI scans of asymptomatic individuals with those with biopsy proven diskitis. An epidural abscess is seen as an area isointense with the cord or cauda equina on T1-weighted images that may cause effacement of the neural structures, and on the T2-weighted images, these lesions reveal a high signal expression. Gadolinium-enhanced T1-weighted images provide additional evidence of infection, as enhancement of the collection is typically quite apparent Gram negative organisms: Historically, the primary gram-negative pathogens have been E. coli, Klebsiella species, and P. aeruginosa, but there is wide variability in the pathogens isolated in different treatment centers]. The relative incidence of gram-negative bacilli as causes of initial infections has decreased significantly during the past 2 decades, but they remain important pathogens for patients with profound neutropenia (<100 polymorphonuclear leukocytes/µL) with a prolonged duration (7–10 days) or for patients who have not received antibacterial prophylaxis during their period of neutropenia. Dermatologic manifestations of gram-negative skin and soft-tissue infections include erythematous maculopapular lesions, focal or progressive cellulitis, cutaneous nodules and ecthyma gangrenosum. Ecthyma gangrenosum begins as painless, erythematous, macules that rapidly become painful and necrotic during a 12–24-h period. They may be discrete or multiple; are found preferentially in the groin, axilla, or trunk; and can increase in size from 1 cm to >10 cm in <24 h. Ecthyma gangrenosum is a cutaneous vasculitis caused by bacterial invasion of the media and adventitia of the vessel wall. Progression of the lesion leads to dermal necrosis, and bacteria are often visible during microscopic analysis of biopsy specimens. Ecthyma gangrenosum has classically been reported to occur with P. aeruginosa infections, but similar lesions can occur with disseminated infections caused by other Pseudomonas species, Aeromonas species, Serratia species, S. aureus, Stenotrophomonas maltophilia, Candida species, and fungi, including Aspergillus, Mucor, and Fusarium species Case 1Incision site Case2 Incision site Case -2 Gr IIID A deep incision spontaneously dehisces or is deliberately opened by a surgeon when the patient has at least one of the following signs or symptoms - fever (>38°C), localized pain or tenderness - unless the culture is negative Practice Guidelines for the Diagnosis and Management of Skin and Soft-Tissue Infections Incidence of SSIs following closure/delayed closure of an infected wound Opening and re-closure times Reinfection rate Opening and re-closure at once 50% Opening and re-closure after two days 20% Opening and re-closure after four days 5% Opening and re-closure after nine days 10% Classification of postoperative wound and scoring system. Conclusion:Major factors has beed analysed with review of the literature.Patient factors,surgical factors are major cause of SSI in case I and Case 2.Malnutrition ,Diabetes and renal impairement is associated with Case2.CRP is strong marker of infection in case 2 associated with evidence of infection and culture positivity.Modifiable risk factors should corrected before surgery.