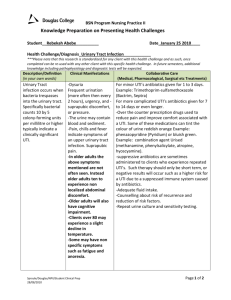
Urinary Tract Infection
advertisement

Urinary Tract Infection Date: October 2014 Guideline(s) Reviewed: 1. Cincinnati, 2006. UTI Guideline Team, Cincinnati Children’s Hospital Medical Center: Evidence-based care guideline for medical management of first urinary tract infection in children 12 years of age or less. http://www.cincinnatichildrens.org/assets/0/78/1067/2709/2777/2793/9199/c 2dda8f2-f122-4cc4-9385-f02035d4f322.pdf . Guideline 7, pages 1-23, November, 2006 2. NICE, 2007. National Collaborating Centre for Women’s and Children’s Health. Urinary tract infection in children: diagnosis, treatment and long-term management. 2007. 3. Roberts, KB. Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management. Urinary Tract Infection: Clinical Practice Guideline for the Diagnosis and Management of the Initial UTI in Febrile Infants and Children 2 to 24 months. Pediatrics. 2011;128(3):595–610. 4. Seattle Children’s Hospital Urinary Tract Infection Pathway Topic Owner: Kristi Kiyonaga, MD (kkiyonaga@everettclinic.com) OBJECTIVES 1. Provide criteria for accurate diagnosis 2. Provide criteria for hospitalization 3. Outline appropriate, age- and development-specific therapies 4. Reduce unnecessary laboratory testing, radiography, and hospitalization 5. Prevent complications of urinary tract infection (UTI) SUMMARY: 1. Diagnosis a. Diagnose infants and non-toilet trained children via high quality catheter specimen (not a bag) when possible. b. In sexually active adolescents, test for gonorrhea (GC) and chlamydia (CT) and offer an external genitourinary (GU) exam and/or self-obtained vaginal swab. 2. Empiric Therapy a. Start empiric therapy in non-toilet trained infants and children when there is clinical suspicion of UTI (presence of signs or symptoms and clinical experience), regardless or urinalysis results. b. Start empiric therapy in toilet trained children and adolescents when there is clinical suspicion and a positive urinalysis. c. Hospitalize infants 0-30 days of age with suspected UTI for empiric IV antibiotics. Urinary Tract Infection d. Empiric therapy in infants 31-60 days of age not meeting criteria for admission is ceftriaxone IM. e. Empiric therapy in non-toilet trained children, toilet-trained children and adolescents is cephalexin or cefuroxime. f. Target antibiotic therapy to sensitivities once available. 3. Outpatient treatment a. For infants 31-60 days of age, treat for 14 days. b. For non-toilet trained children, treat for 7-14 days. c. For toilet-trained children and adolescents with cystitis, treat for 3 days. d. For pyelonephritis, treat for 7-14 days. 4. Imaging and follow-up a. For infants and non-toilet trained children, perform renal bladder ultrasound (RBUS) or review high quality third trimester ultrasound. b. For toilet-trained children and adolescents, perform RBUS on boys diagnosed with first-time UTI and girls with atypical* UTI. c. Do not routinely perform a VCUG. VCUG is indicated for abnormal RBUS findings or atypical* UTI. d. Do not routinely perform a follow-up culture for test of cure. 1. Inclusion Criteria a. Birth to 18 years of age with a corrected gestational age of at least 40 weeks b. Suspected or confirmed UTI (but not chronic or recurrent UTI) 2. Exclusion Criteria a. Prior history of UTI b. Anatomic genitourinary abnormalities c. Chronic kidney disease (estimated GFR < 80 mL/min/1.73m²) d. Immunocompromised host e. Pregnancy f. Recent history of sexual abuse 3. Assessment/Diagnostic Test(s) a. Definitions: i. Urinary tract infection: combination of clinical features and the presence of bacteria in the urine a. Acute pyelonephritis / Upper urinary tract infection: inflammation of the kidneys due to UTI that manifests with fever 38°C or higher b. Cystitis / Lower urinary tract infection: inflammation of the bladder due to UTI that is confined to the lower urinary tract b. Diagnosis: i. Presumed UTI: 1. Infants and non-toilet trained children: clinical features where UTI is deemed likely (Reason: Urinalysis in these age groups Urinary Tract Infection have been shown to be insufficient to rule in or rule out urinary tract infection.) 2. Toilet-trained children and adolescents: combination of clinical features and a positive urinalysis ii. Definite UTI: combination of clinical features and a positive urinalysis and urine culture iii. Positive urinalysis (UA): demonstrates pyuria and/or bacteriuria 1. Leukocyte esterase (LE) is a surrogate marker for pyuria. 2. Nitrites are a surrogate marker for gram-negative enteric bacteriuria. 3. ≥5 WBCs per HPF on microscopy demonstrates pyuria (≥10 WBCs per μL if counting chamber is used). 4. Presence of bacteria on microscopy demonstrates bacteriuria. iv. Positive urine culture: 1. Catheterized specimen: ≥ 50, 000 CFUs / ml of a single uropathogen (at SCH equivalent to ≥ 10,000 CFUs¹) 2. Clean catch specimen: ≥ 100, 000 CFUs / ml of a single uropathogen c. Diagnostic Testing i. 0-60 days 1. Testing indicated if patient has fever, irritability, lethargy, emesis, failure to thrive, prolonged jaundice of unknown etiology. 2. Obtain a UA and urine culture, preferably by catheterization. If catheterization is not successful or not available, obtain bag specimen only to determine if negative. DO NOT SEND BAG SPECIMEN FOR CULTURE. Consider referral to ED for definitive testing when high clinical suspicion and unable to obtain catheterized specimen. 3. Do not use a positive UA obtained by bag or clean catch as evidence of a UTI; confirmation requires positive UA and culture of a specimen collected through catheterization. ii. Non-toilet trained children > 60 days of age 1. Test febrile (>39°) girls or uncircumcised boys with ≥ 1 of the following and febrile (>39°) circumcised boys with ≥2 of the following or suprapubic tenderness alone: I. Ill appearing II. Fever >39° for 48 hours without a source III. Abdominal pain / suprapubic tenderness IV. Boys: nonblack race V. Girls: white race 2. Discuss testing options with parents and consider feasibility of catheterization. Options: _____________ ¹Note that this differs from the SCH UTI guideline because the SCH lab does not report cutoffs of 50,000 and their cutoff of 10,000 is considered fairly equivalent. Urinary Tract Infection iii. I. Obtain a catheterized UA and urine culture. II. If catheterization is not successful, not available or if parents prefer noninvasive testing: obtain bag specimen only to determine if negative. If negative, no further testing required. DO NOT SEND BAG SPECIMEN FOR CULTURE. If positive, attempt to obtain urinalysis and urine culture via catheterization. * 3. Do not use a positive UA obtained by bag urine as evidence of a UTI; confirmation requires positive UA and culture of a specimen collected through catheterization. Toilet-trained children and adolescents 1. Testing indicated if patient has abdominal pain, back pain, dysuria, frequency, new-onset incontinence, fever > 40° (particularly if no source). 2. Obtain a urinalysis and urine culture from midstream clean catch. Definitive diagnosis requires that both suggest infection. 3. Sexually active adolescents and pre-adolescents: also obtain ‘dirty’ urine for GC/CT testing and offer an external GU exam and/or a self-obtained vaginal swab. I. ‘Dirty urine’: Do not apply alcohol wipe to external genitalia. Collect the first part 15-20 mL of the urine stream. II. Vaginal swab: insert swab into vagina about 2.5 inches in or as far as comfortable. Rotate for 15 to 30 seconds, then remove. 4. Disposition a. Outpatient management recommended if: i. Tolerating po ii. Infants 31-60 days of age who are afebrile and well-appearing iii. Well-appearing non-toilet trained children, toilet-trained children, and adolescents b. Indications for hospitalization: i. Less than 30 days of age with presumed or definite UTI. (If febrile and age 0-60 days also refer to SCH neonatal fever pathway.) ii. 31-60 days of age if febrile with presumed or definite UTI iii. Moderately or severely ill-appearing (e.g., febrile and not tolerating po). iv. Concerns for the family’s ability to adhere to recommended therapy, return for appropriate follow up, or seek/access emergency care (Exception: In adolescents with cystitis, adherence risk is not an admission criteria.) *Definitive diagnosis of UTI in non-toilet trained children requires a positive urine culture obtained by catheterization. However, in situations where this is not possible and UTI treatment is started empirically, consider appropriate follow-up imaging. Urinary Tract Infection 5. Outpatient Management a. 31-60 days of age: i. IM ceftriaxone (75mg/kg/day once daily; maximum dose 2 g) until culture and sensitivities available ii. Follow-up within 24 hours iii. Treatment duration is 14 days. b. Infants and Non-toilet trained children > 60 days of age: Start empiric therapy when there is clinical suspicion of UTI, regardless of urinalysis results. i. Cephalexin (50 mg/kg/day orally divided 2-4 times/day; max dose 4 g/day) or cefuroxime (10 mg/kg/dose 2 times/day). ii. In children who are penicillin-allergic, consider TMP-SMX. iii. May consider daily IM ceftriaxone (75mg/kg/day; maximum dose 2 g) initially. iv. Treat with full course of antibiotics for definite UTI only (positive UA and > 50,000 CFUs / mL for cultured catheterized specimen or 100,000 CFUs / mL for cultured clean catch specimen). v. Treatment duration is 7-14 days. c. Toilet-trained children and adolescents: Start empiric therapy when there are clinical findings in addition to a positive urinalysis / microscopy. i. Cephalexin (50 mg/kg/day orally divided 2-4 times/day; max dose 4 g/day) or cefuroxime (10 mg/kg/dose 2 times/day). ii. In children who are cephalosporin-allergic, consider TMP-SMX 810mg/kg divided 2 times/day, maximum 160mg of TMP. iii. Treat with full course of antibiotics for definite UTI only (positive UA and > 100,000 CFUs / mL for cultured clean catch specimen). iv. Treatment duration is 3 days in afebrile patients and 7-14 days in febrile patients (pyelonephritis). d. All age groups: Target antibiotic therapy to sensitivities once available. e. All age groups: Consider probiotics for antibiotic-associated diarrhea f. Imaging and prophylaxis i. Infants 0-60 days of age and non-toilet trained children 1. Obtain renal bladder ultrasound (RBUS) during or soon after treatment to assess renal anatomy and evaluate for hydronephrosis. Can skip if high quality (detailed anatomic survey with measurements) third trimester U/S is normal. 2. Obtain a voiding cystourethrogram (VCUG) if: I. Atypical* UTI II. RBUS shows evidence of high-grade VUR or obstructive uropathy such as hydronephrosis, renal parenchymal loss, or kidney size discrepancy. 3. Prophylaxis is recommended prior to VCUG Urinary Tract Infection I. Infants < 2 months: amoxicillin (20 mg/kg once daily; maximum dose 500 mg) II. Infants and children > 2 months: TMP-SMX (2 mg/kg of TMP once daily; maximum dose 80 mg) or nitrofurantoin (1mg/kg once daily; maximum dose 100 mg) 4. Obtain a DMSA Scan in 12 months if: I. < 6 months of age with atypical* UTI II. RBUS shows evidence for renal parenchymal loss or kidney size discrepancies ii. Toilet-trained children and adolescents 1. Obtain a renal bladder ultrasound (RBUS) after treatment if: I. Male with first UTI II. Female with atypical* UTI 2. Obtain a voiding cystourethrogram (VCUG) if: I. Atypical* UTI II. RBUS shows evidence of high-grade VUR or obstructive uropathy such as hydronephrosis, renal parenchymal loss, or kidney size discrepancy. 3. Prophylaxis is recommended prior to VCUG: TMP-SMX (2 mg/kg of TMP once daily; maximum dose 80 mg) or nitrofurantoin (1mg/kg once daily; maximum dose 100 mg). 4. Obtain a DMSA Scan in 12 months if RBUS shows evidence for renal parenchymal loss or kidney size discrepancies. g. Antibiotic Prophylaxis i. Ongoing antibiotic prophylaxis is not recommended for patients with first febrile urinary tract infection. ii. Antibiotic prophylaxis is not recommended for grade I-III vesicoureteral reflux. 6. Reassessment a. Expect clinical improvement within 48 hours of starting antibiotics. b. Expect resolution of fever within 72 hours of starting antibiotics. c. Reassess all infants between 31-60 days of age being treated for presumed or definite UTI as an outpatient within 24 hours. 7. Other Considerations a. If a febrile infant < 60 days of age or non-toilet-trained child requires antibiotics because of ill appearance or other pressing reason, obtain urinalysis and urine culture by catheterized specimen prior to antibiotic administration. b. Consider asymptomatic bacteriuria in absence of pyuria, particularly in school-aged and older girls. Asymptomatic bacteriuria normally resolves spontaneously, and therefore does not require treatment with antibiotics. Urinary Tract Infection c. Address dysfunctional elimination. d. In adolescents with suspected UTI consider culturing visible lesions for HSV, rapid plasma reagin if GC/Chl positive, annual HIV testing, pregnancy testing *Atypical versus Typical UTI An atypical UTI is defined as a UTI with one of the following properties: • Seriously ill • Poor urine flow • Abdominal or bladder mass • Elevated creatinine (eGFR < 80 ml / min / 1.73 m2) • Septicemia • Failure to respond to treatment with suitable antibiotics within 48 hours • Infection caused by organism other than Escherichia coli A typical UTI is defined as a UTI without any of these conditions.