ETIOLOGY OF PERIODONTAL DISEASES DENTAL PLAQUE
advertisement

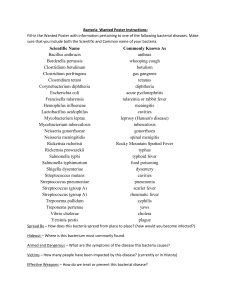
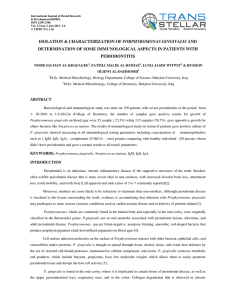
ETIOLOGY OF PERIODONTAL DISEASES DENTAL PLAQUE = PERIODONTITIS? • dental plaque → gingivitis (Loe 1965) • dental plaque → periodontitis • dental plaque → no periodontitis PERIODONTITIS – PATOGENESIS • participation of many genetic and environmental factors (multi-factorial disease) • presence of different species of bacteria (polymicrobial infection) • a susceptible host • the presence of pathogens • absence of beneficial bacteria • a conductive environment in the pocket DENTAL PLAQUE - MATRIX • bacterial components (polysaccharides) • host components (saliva glycoproteins, dead cells, serum proteins) DENTAL PLAQUE - BACTERIA • approximatly 500 species • 1010 – 1012 of bacteria per gram of plaque HOW DO BACTERIA CAUSE PERIODONTAL DISEASE? • acquisition → at birth (from mother) → later (from partner) • adherence/retention → glycoprotein pellicle → mucopolysaccharides (Gram-positive streptococci) → lipoteichoic acids (Gram-negative bacteria) • survival → presence of glucose and iron → biofilm – a complex structure (bacteria, matrix, bacterial antigens and toxins) → avoidance of elimination by host defense system • multiplication • elaboration of virulence factors → enzymes (collagenase, elastase, hyaluronidase) → metabolic waste products (ammonia, cytotoxic amines, volatile fatty acids) → toxins (endotoxins – LPS, exotoxins – leucotoxin) MATURATION OF PLAQUE BIOFILM • immature plaque Gram-positive aerobic and facultative bacteria→ rods and cocci (S. sanguis, Actinomyces sp.) • matured plaque Gram-negative anaerobic bacteria → rods, spirochetes WHICH ORGANISMS CAUSE PERIODONTAL DISEASE 1. THE SPECIFIC PLAQUE HYPOTHESIS (Loesche 1976) Specific microorganisms are necessary for the development of periodontal disease Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Tannerella forsythia 2. THE NON-SPECIFIC PLAQUE HYPOTHESIS (Thielade 1986) Periodontal disease results from the shear mass of bacteria present and once this exceeds a certain threshold, disease will occur 3. THE ENVIROMENTAL PLAQUE HYPOTHESIS (Haffajee 1991) The entire subgingival microbial environment is the key to periodontal disease developing Condition Organism Healthy gingivae Streptococcus sanguis Actinomyces viscosus Streptococcus oralis Gingivitis Fusobacterium nucleatum Porphyromonas gingivalis Necrotising ulcerative gingivitis Treponema vincentii Fusobacterium nucleatum Prevotella intermedia Condition Organism Localised aggressive periodontitis Aggregatibacter actinomycetemcomitans Generalised aggressive periodontitis Porphyromonas gingivalis Chronic periodontitis Porphyromonas gingivalis Tannnerella forsythia Treponema denticola Fusobacterium nucleatum Campylobacter rectus Eikenella corrodens Peptostreptococcus micros Prevotella intermedia THE ENVIROMENTAL PLAQUE HYPOTHESIS (Haffajee 1991) • Bacteria must be of a virulent clonal type • The host must be susceptible to the pathogen • The number of pathogens within a clone must exceed a threshold for the host • Bacteria must be located at correct site • Other species must support or at least not inhibit the pathogen • The local environment must be conductive the the production of virulence factors SUBGINGIVAL BIOFILM (Socransky 1998) • certain organisms cluster together in discrete micro-environments Complex Bacteria Purple Veillonella parvula (gram-positive rods and cocci) Actinomyces odontolyticus I Yellow Streptococcus sanguis (gram-positive facultative cocci) Streptococcus godonii Streptococcus intermedius Streptococcus oralis Streptococcus mitis Green Eikenella corrodens (gram-positive and gram-negative rods/ cocci non-motile) Aggregatibacter actinomycetemcomitans Capnocytophagia ochracea Capnocytophagia sputigena Capnocytophagia gingivalis Complex Bacteria Orange Fusobacterium nucleatum (gram-positive and gram-negative rods/ cocci some motility) Fusobacterium periodonticum Prevotella intermedia Prevotella nigescens Streptococcus constellatus Eubacterium nodatum Campylobacter gracilis Campylobacter rectus Campylobacter showae Peptostreptococcus micros Red Porphyromonas gingivalis (gram-negative, anaerobic, motile) Tannerella forsythia Treponema denticola Porphyromonas gingivalis • Gram-negative anaerobic rod • dark pigmentation on media containing lysed blood • Black pigmentation due to accumulated hemin used as an iron source for growth Virulence factors • IgA proteases • Collagenases • Hemagglutinins - mediate the binding of Pg to epithelial cells and erythrocytes • LPS – endotoxin • Gingipain(cystein proteases) • Trypsin-like protease • Fimbriae - mediate the binding of Pg to epithelial cells • Cytotoxic metabolic end products - butyrate, propionate, have low molecular weights which allows them to easily penetrate periodontal tissue and disrupt the host cell activity Tannerella forsythia Virulence factors • LPS - endotoxin • Trypsin-like protease • cell-wall lipoproteins -induction of apoptosis • Cytotoxic metabolic products– fatty acids Treponema denticola Virulence factors • Major outer membrane protein (Msp) - 53-kDa adhesin with pore forming activity, cytotoxic for epithelial cells and erythrocytes • Proteases - involved in cell attachment, tissue destruction, tissue invasion • Hemin- /lactoferrin-binding proteins - iron acquisition and utilizes lactoferrin from the saliva • Immunosuppressive activity - suppressed lymphocyte proliferative responses to antigens and mitogens Aggregatibacter actinomycetemcomitans Virulence factors • Leukotoxin - binds monocytes, neutrophils and lymphocytes, forms pores and leakage of contents • LPS – endotoxin • Collagenases • IgA proteases • Fc-binding proteins -proteins that bind the Fc region of Igs, can compete with neutrophils for binding to the Fc and therefore inhibit phagocytosis • Fimbriae CONCLUSIONS OF CLINICAL IMPORTANCE • Gingivitis is a disease caused by the progressive accumulation of plaque at the gingival margin - plaque removal results in resolution • The majority of patients may suffer from gingivitis • Specific bacteria cause chronic periodontitis, they exist in a subgingival biofilm, where selfsupport and protection provide resistance to elimination • Only a small number of patients appear susceptible to aggressive periodontitis • Physical disruption of the biofilm is essential to eliminate anaerobic pathogens • Pathogens can be transmitted within families • Failure of therapy me be due to factors peculiar to the patient, but may also be due to reinfection from a partner or family member HOST RESPONSE innate immunity → intact epithelial barriers → anti-bacterial factors present in saliva or GCF → neutrophils and macrophages → complement cascade → chemokines i cytokines acquired immunity • T cells • B cells • immunoglobulins CYTOKINES ADN PERIODONTITIS Cytokine Source Effect IL-1 IL-6 TNF PGE2 macrophages activation of osteoclasts fibroblasts activation of neutrophils epithelial cells production of PGE2, TNF and IL-6 macrophages production of acute phase proteins fibroblasts bone resorption epithelial cells activation of T and B cells macrophages production of IL-1 and PGE2 epithelial cells activation of neutrophils macrophages blood vessel permeability neutrophils activation of neutrophils mast cells bone resorption epithelial cells CONCLUSIONS OF CLINICAL IMPORTANCE • In clinical health, PMNs are the predominant defence cells. Innate immunity functions at a low level, without causing significant tissue damage • As plaque builds up, complement activation leads to a greater inflammatory response and gingival tissue damage • With time, T and B lymphocytes appear, providing specific and controlled killing of bacteria • If left untreated in disease-susceptible patients, the size of inflammatory response exceeds a threshold, and the host tissue damage occurs as a side-effect of the defence strategy RISK ASSESSMENT Risk factor – a factor that increases the probability that a disease may develop in an individual 1. systemic (subject-based) risk factor (smoking) 2. local (site-based) risk factor (overhanging restorations occlusal forces) Risk marker (predictor) – is not linked to ‘causation’, but is a consequence of the disease being present (bleeding on probing) RISK FACTORS • genetic (inherited syndromes, polymorphism of cytokines, FcR, MMPs) • behavioural (poor oral hygiene, smoking, stress, malnutrition) • metabolic disorders (diabetes mellitus, pregnancy, oral contraceptive, osteoporosis) • haematological (leukaemia, myelodysplasia syndrome, agranulocytosis) • drugs (phenytoin, calcium channel blockers, cyclosporine) MOST IMPORTANAT RISK FACTORS FOR PERIODONTAL DISEASE Increased plaque amount • improper oral hygiene • overhanging restorations or crowns • caries cavities • teeth crowding • xerostomia Improper host defence • innate or acquired host immune deficiency • hyperreactivity of host immune system (IL-1) and other genetic factors • general diseases (diabetes) • environmental factors (stress, smoking, unbalanced diet, certain medications) GENE POLYMORPHISMS AND PERIODONTITIS IN THE CAUCASIAN POPULATION • IL-1α (-899), (+4845)C>T • IL-1β (+3953/4)C>T • IL-6(-572)G>C • IL-10 (-819)C>T, (-592)C>A • IL-18 (-607)A>C, (-137)G>C • FCGR2A, FCGR3A SMOKING AS A RISK FACTOR • 3-6 times higher risk of periodontitis • one cigarette per day increases attachment loss by 0,5% • prevalence of T. forsythia • harder to eradicate A.a., P.g. and T.f. • level of salivary IgA • release of TNF, IL-1, i IL-6 by monocytes when stimulated by LPS • destruction of extra-cellular matrix proteins • gingival keratosis and fibrosis • gingival blood flow