Froberg_Diseases_of_Infancy_and_Childhood_3.22.10
advertisement

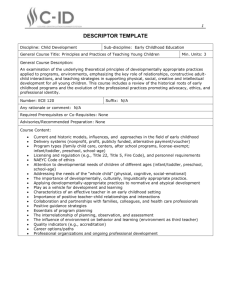
Froberg --Diseases of Infancy and Childhood—3.22.10 Objectives: •Learn basic epidemiology of childhood causes of death •Learn factors contributing to intra-uterine growth retardation (IUGR) •Understand the pathophysiology of Respiratory Distress Syndrome (RDS) •Know the major factors related to metabolic inherited diseases of childhood, SIDS, and benign & malignant neoplasms of childhood Causes of Death & Age •Under 1 yr IUGR, RDS, congenital anomalies, SIDS, pneumonia •1-4 yrs injuries, congenital anomalies, malignant neoplasms, homicide •5-9 yrs injuries, malignant neoplasms, congenital anomalies, homicide •10-14 yrs injuries, malignant neoplasms, suicide, homicide •15-24 yrs injuries, suicide, homicide (all traumatic stuff) Birth Weight and Gestational Age •AGA=appropriate for gestational age, SGA=small, LGA=large •10-90th percentile = AGA •Before 37th week = preterm, >42 = post-term –1500gm infant at 32 weeks has mortality risk of ~20% –700gm infant at 32 weeks has mortality risk of 65% -mortality is more related to weight than gestational age. Mortality is related to gestational age, but birth weight is more important for infants of the same gestational age. -So for a 32 week infant of 700 g the expected mortality is 63%, while for a 1750 g infant of the same gestational age the expected mortality is ~6%. Neonatal intensive care has improved the survival of preterm infants. IUGR •Underlies SGA, detect by US •Factors relating to IUGR: –Fetal - trisomies, congenital anomalies & infections (symmetric growth retardation-Type I) –Placental - uteroplacental insufficiency, thrombosis, infarction, abruption, placenta previa, confined placental mosaicism (placenta can have division of DNA) (disproportionate growth retardation-Type II) –Maternal - most common: includes toxemia, HTN, malnutrition, ETOH, smoking, narcotics, teratogens (often cause learning disabilities, cerebral dysfunction) 1 Organ Immaturity: Problem of preterm regardless of weight –Lungs - alveoli mature late in gestation (7th month), alveoli lined by cuboidal epith prior to 26-32 weeks, septa thick, reach full compliment of alveoli by 8 yrs (develop slowly over yrs) –Brain - smooth surface, soft, nerve fibers poorly myelinated –Liver - large but physiologically immature, jaundice esp in low birth wt infants (def bilirubin glucuronyl transferase, etc) Infant Mortality •20.0 per 1000 population in 1970 7.5 per 1000 in 1995 •Rate for blacks >twice whites: 14.9/1000 compared to 6.3/1000 •US infant mortality ranks 21st among industrialized nations Socioeconomic factors underlie the frequency of low birth weight babies (worse in SE) Congenital Anomalies •In 3% of newborns, major cause of M&M in 1st yr •Definitions: –Malformations - intrinsic abnl occurring during development, ex. Anencephaly –Deformations - arise later in fetal life, alteration in structure from mechanical factors (small uterus, leiomyomata) or fetal-placental (abnl presentation, multiple births, oligohydramnios, ex. Clubfeet) More Definitions •Disruptions - 2 interference with previously normal organ or region, ex amniotic bands •Sequence - pattern of cascade anomalies, ex. Potter’s sequence: renal agenesis oligohydramnios pulmonary hypoplasia •Other terms: agenesis - organ & primordium absent; aplasia failure of organ development; atresia - absent opening; hypoplasia - # of cells; hyperplasia - # of cells; dysplasia abnl organization Amniotic Band An amniotic band has interrupted development of a lower extremity (arrow). Placenta is present to the right. Causes of Malformation 1. Genetic - include karyotypic aberrations, single gene mutations, multifactorial –Abnl karyotype in 10-15% of live-born infants with congenital malformations; frequency - Down, Klinefelter, Turner, Patau syndromes –Usually arise during gametogenesis, so not familial –Single gene mutations - Mendelian, uncommon (210%) - Marfan syndrome –Multifactorial - interaction with environment (2025%) (cleft lip/palate) 2. Environmental - infections (TORCH), maternal disease states (diabetes), drugs (thalidomide) Infections -rubella in 1st trimester can cause cataracts, heart defects, deafness (50% in 1st month of gestation) Froberg --Diseases of Infancy and Childhood—3.22.10 CMV - most common cause of fetal viral infection, can cause MR, deafness, hepatosplenomegaly thalidomide - limb malformations (50-80%), amelia & phocomelia (underdeveloped limbs) ETOH - growth retardation, microcephaly, ASD Examples of Toxicants associated with impairment of fetal growth -drugs of abuse: cigarette, ethanol, heroin -Rx: glucocorticoids, propranolol, phenytoin, warfarin -infectious agents: Herpes simplex, CMV, rubella, toxoplasmosis Malformations: Timing - critical to type & severity of malformation -early embryogenesis - 1st three weeks death more likely -organogenesis - weeks 3-9 most susceptible to teratogens Teratogens & genetic defects may act on cell proliferation, migration, differentiation or damage formed organs - affect growth factors (WT-1, TGF-) -Hox (homeobox) genes interact with multiple downstream genes, hence is a regulator of morphogenesis, can be affected by retinoids - temporal & spatial expression of retionic acid-binding proteins may affect morphogenesis 3-9 wks you will see greatest effects of insult Forms of vitamin A are necessary for normal development but in excess can cause malformations -Excess renioic acid (Vit A) MS, CNS, cardaic -Def Vit A defects of eye, lung, cardiac -Enters nucleus, binds to response element alt HOX genes patterns of malformation 2 Perinatal infections Ascending - transcervical leading to –funisitis (cord) & –chorioamnionitis (membranes), –fetus may inhale amniotic fluid or contact microbe in birth canal during delivery; most bacterial, few viral •Hematological - most viral or parasitic; Treponema, Listeria, HIV, Hep B •Perinatal sepsis - group B Strep and E. coli lead to pneumonia and sepsis in 4-5 days, late sepsis - Listeria and Candida •TORCH syndrome: toxoplasma, rubella, cytomegalovirus, herpesvirus and others (syphilis, etc.). –Cause similar clinical & pathological picture in newborn. –Clinical: fever, encephalitis, chorioretinitis, hepatosplenomegaly, pneumonitis, myocarditis, hemolytic anemia, and vesicular or hemorrhagic skin lesions. –Chronic sequelae: growth & learning delays, cataracts, cardiac anomalies and bone defects Respiratory Distress Syndrome/Hyaline Membrane Disease •Still common in newborn period, affects 60-70,000 infants/yr –Risk Factors: •excess sedation of mother respiratory depression & brain injury •Prematurity muscle & resp immaturity (1 atelectasis) •Aspiration of blood, mucus, squames, amniotic fluid •Umbilical cord coils hypoxia •Mortality previously 25,000 infants/yr, now 5,000 •CSx: usually preterm, or associated with maternal diabetes or cesarean section –May see resuscitation at birth improve –Soon develop resp distress grunting, retraction, cyanosis, rales on auscultation, ground-glass picture by CXR, may progress despite ventilator assistance •Pathogenesis: incidence ~ 1/gestational age, 60% <28 wks, 15-20% if 32-36 wks, <5% if over 37 wks –Main defect is lack of surfactant - 75% is phosphatidylcholine (lecithin) made by type II pneumocytes esp after 35th week, sphingomyelin is universal cell membrane component (use for relative baseline) –L/S ratio 2.0 or > in amniotic fluid = 95% chance of no RDS, matures rapidly (1-2 days) RDS Pathology •Gross - lungs stiff, solid, reddish purple •Micro - atelectasis & dilation, hyaline membranes, cell debris •Rx: oxygen, ventilatory assistance, surfactant •Complications: bronchopulmonary dysplasia (emphysematous changes 2 to ventilatory injury), PDA, IVH, necrotizing enterocolitis •Mortality ~1/body wt 3 Froberg --Diseases of Infancy and Childhood—3.22.10 self perpetuating cycle of pathology. With this damage you get leaky caps fibrinogen fibrin + necrotic cells hyaline membranes thicker wall inc diffusion gradient The most common variant of galactosemia occurs from a lack of galactose-1-phosphate uridyl transferase. A rare variant is due to galactokinase deficiency Atelectasis & dilation uneven ventilation. Congestion of bld vessels. hyaline membranes Phenylketonuria (PKU) •Autosomal recessive disorder caused by lack of phenylalanine hydroxylase PKU, incidence 1/20,000 births, pathogenesis unknown •NL at birth, rapid serum phenylalanine severe MR by six months, Only 4% of untreated PKU pts have IQ>50 or 60, also see seizures, eczema, hypopigmentation, 2/3 unable to talk, 1/3 unable to walk (bad!) •Can prevent MR by restricting phenylalanine in diet •Other forms of PKU: –Maternal PKU: profound MR in child of non-compliant mother with PKU (although child is heterozygote) –Benign PKU: perinatal screen (Guthrie test) positive but only partial def of phenylalanine, serum levels NL (so ), don’t develop stigmata –Other variant forms: may affect other enzymes in cascade, some transient, some due to lack of tetrahydrobiopterin cofactor, can see neurological impairment with NL serum phenylalanine levels Pathway of phenylalanine metabolism: in PKU PAH is usually reduced or absent. However, deficiencies in BH4 or DHPR may also lead to PKU or a positive Guthrie test. •Newborn screening tests: -heel stick bld collection –Urine + FeCl3 black color in presence of phenylpyruvate –Guthrie test - heel stick -bacterial inhibition assay, repeat if + and follow serum phenylalanine (1% of newborns +, but 90% FP rate) –Molecular tests Galactosemia •Autosomal recessive: classic form - lack of galactose-1phosphate uridyl transferase & accumulate substrate (some galactokinase def.), incidence 1 per 80,000 whites –Targets liver, brain & eyes steatosis, cirrhosis, cataracts, neuronal loss & gliosis (MR in severe form) –Eye: galactose converted by aldose reductase to galactilol absorbs water cataracts Galactosemia •Mechanism of liver & CNS damage unknown •CSx: reluctant to nurse, Failure to thrive, Vomit & Diahhrea, hepatomegaly, MR by 6-12 months, jaundice, neonatal sepsis (E. coli) •Dx: enzyme def in RBCs, heel stick for enzyme immunoassay, can do on amniotic fluid •Rx: restrict dietary galactose (milk) Fibrosis & fatty liver from galactosemia Cystic Fibrosis (not on test – see module) Sudden Infant Death Syndrome •“Crib Death,” sudden, unexplained death of infant <1 yr of age after thorough investigation 1.~ 6000/yr in US, worldwide 1-5/1000 live births 2.90% in first 6 months of life (peak 2-4 months) 3.Cyanosis and cessation of respirations, most have minor manifestations of URI 4. Risk factors: mother <20 yrs, unmarried, smoking, low socioeconomic status, drug abuse, black race, infant prematurity, LBW, male sex, SIDS in prior sibling 5. 1-10% have inborn error of metabolism like acyl-CoAdehydrogenase def, may be heterogeneous group of disorders with same outcome, some homicides 6. Apnea & abnl temperature control thought to be involved, delayed autonomic development? 7. Supine SIDS Tumors & Tumor-Like Lesions •Only 2% of all malignant neoplasms occur in infancy & childhood, but 2nd leading cause of death 4-14 yrs of age 1.Heterotopia (choristoma) - NL cells in abnl location, ex. adrenal rests 2.Hamartoma - excessive growth of cells/tissues native to organ, ex. Cardiac myomas & subependymal hamartomas of tuberous sclerosis 3. Benign - may be difficult to distinguish from hamartomas, are most common neoplasms of childhood •Hemangiomas - most common tumor of infancy, skin of face & scalp, flat to elevated, irregular, red-blue masses. Very large = port-wine stains. May regress Froberg --Diseases of Infancy and Childhood—3.22.10 spontaneously. May be part of von Hippel-Lindau Syndrome (tumor suppressor gene in vasc development. Hemangioblastoma of cerebellum, cysts of organs, renal cell carcinomas, often hemangiomas as well) 4. Teratomas - tumor composed of more than one germ cell layer, may be benign (mature) cystic or malignant (immature) solid masses. May be congenital. Sacrococcygeal > head & neck, gonads, mediastinum, incidence 1/20,000, F:M is 4:1, 75% benign, may cause non-immune hydrops fetalis (massive edema); Rx: surgery Fetal ultrasound showing heart chambers of 18 week of gestation fetus Ultrasound seven weeks later showing a large mediastinal mass An island of cartilage is surrounded by glands showing dissolution in mature teratoma Neuroepithelial rosette (arrow) in benign teratoma liver The heart (red arrow) is displaced by a large mediastinal mass (black arrow) Tumors: Malignant Concepts •May be related to abnl development •May regress or cytodifferentiate •Rx may lead to 2 malignancies •Small , round, blue cell tumors •Sites: hematopoetic, nervous system, soft tissue, bone •Include neuroblastoma, lymphoma, rhabdomyosarcoma, PNET/Ewing’s sarcoma 4 Neuroblastoma •Most commnon malignant tumor of children <1yr, 15% of childhood cancer deaths, 35% in 1st yr of life, 85-90% prior to age 5 •25-35% arise in adrenal medulla, rest along sympathetic chain (paravertebral mediastinum or abdomen, pelvis, neck, even brain) •Gross: soft, gray, hemorrhagic, areas of necrosis, calcifications •Histopath: small, round, blue-cell tumor (neuroblasts), HomerWright pseudorosettes (no lumen-fibrillar extensions), may show some level of diffentiation (~ganglioneuroma = benign) •Clinical: present as abdominal mass, fever & wt loss. Later may be signs of mets (GI or resp complaints) •Produce catecholamines (90%) elevated urine VMA and HVA (unlike pheochromocytomas do not typically produce hypertension) •Clinical: –Prognosis: age & stage dependent •<1yr good regardless of stage, if <1yr and stage I or II 95-98% 5-year survival, • >1yr and stage III or IV 10% –Stage IV-S (1 plus single mets to skin, liver or bone mets) 80% 5-yr survival (4S limited to infants <1yr) –Disseminated neuroblastoma to skin may present as “blueberry muffin baby” (multiple hemorrhagic nodules of skin) •Genetics: Commonly have –17q gain (50% of tumors) in unbalanced translocation usually with 1q adverse outcome –1p deletion in region of band p36 (25-35% of tumors), site of likely tumor suppressor gene have worse prognosis •25-50% of neuroblastomas have 14q del & aggressive course •25% have amplification of N-myc oncogene, see double minutes by karyotype have poorer prognosis •Hyperdiploid or near triploid tumors have a better prognosis (divide faster), while diploid tumors have unfavorable outcome •Neuroblastomas may spontaneously regress or differentiate •IF nerve growth factor receptor Tyrosine Kinase A favorable outcome •If Trk A poorer prognosis •Trk A may play a role in maturation of tumor to ganglioneuroma (mature neural elements) •Cytodifferentiation may be spontaneous or following Rx Froberg --Diseases of Infancy and Childhood—3.22.10 Retinoblastoma •Most common malignant eye tumor of childhood •1% of all cancer deaths to 15 yrs •Seen in 1 of 17,000 live births •90% diagnosed prior to age 7 •Gross: nodular mass within globe (arising from retina), do fundoscopic exam on all neonates •Histopath: small, round, blue-cell tumor with FlexnerWintersteiner rosettes (central lumen), histogenesis ~ retinoblasts •Clinical: often present at birth or by 2 yrs with poor vision, strabismus, whitish hue to pupil (cat’s eye) or eye pain, usually fatal once spread beyond orbit •Rx: radiation, laser photocoagulation, cryotherapy, enucleation •Genetics: loss of Fx of retinoblastoma gene at 13q14, a tumor suppressor gene •Hypophosphorylated Rb binds E2F & prevents G1 S transition of cell cycle •Tumors sporadic or hereditary: Knudson “two-hit” hypothesis •Sporadic 60-70% of cases, require two somatic mutations in same retinoblast •Familial (autosomal dominant) have one germline and one somatic mutation •Rb alterations also seen in osteosarcomas, etc. Bone tumors may follow Rx for retinoblastoma 5 Loss of Rb function leads to loss of tumor suppression & cell cycle regulation. Genetic alterations in retinoblastoma include large deletions seen by karyotyping or Southern blot or by point mutations leading to a stop codon. Retinoblastoma: primitive neuroepithelial cells forming FlexnerWintersteiner rosettes (arrow) Knudson two-hit hypothesis: requires one germline and somatic mutation of the Rb gene. Sporadic forms have two mutations within retinal cells after birth Froberg --Diseases of Infancy and Childhood—3.22.10 Wilms Tumor •Most common 1 renal malignancy of childhood •Gross: solitary, gray-tan, well-circumscribed mass, 10% bilateral •Micro: recapitulate stages of nephrogenesis, usually triphasic with blastemal (nephroblasts), stromal and epithelial elements •Clinical: 2-5 yrs, abdominal mass (hematuria, obstruction) •Rx: 5-yr survival now >90% with triple therapy 8. 9. 10. Wilms tumor at lower pole of kidney 11. 12. 13. Wilms Tumor: triphasic histology with blastema (blue), tubular epithlium (red) and stroma (black) 14. 15. 16. 17. •Genetics: sporadic vs inherited, genetic alterations of 11p13 (WT-1) or 11p15.5 (WT-2). WT-1 necessary for NL nephrogenesis •Associated congenital malformations risk of developing Wilms tumor: –WAGR syndrome: aniridia, genital anomalies, MR, & 33% chance of Wilms tumor –Denys-Drash syndrome: gonadal dysgenesis & nephropathy leading to renal failure –Beckwith-Wiedemann syndrome: organomegaly, hemihypertrophy (one side of body much larger), renal medullary cysts, adrenal cytomegaly (WT-2 altered), some have genomic imprinting •Premalignant condition: nephroblastomatosis-persistent immature nephrogenic elements (nephrogenic rest = fetal renal tissue persistent into adult life) Questions: 1. Disproportionate growth retardation is a characteristic of _________. While proportionate growth retardation is a characteristic of __________. Finally, learning disabilities, cerebral dysfunction is often caused by _______________. a. fetal b. Maternal c. placenta 2. What is the difference between disruption and sequence? 3. What is the most common viral infection of pregnancy? What effect does it have on the fetus? 4. Why are Hox genes important? 5. What does TORCH stand for and what effect can these infections have on a fetus? 6. What are risk factors for Respiratory Distress Syndrome? 7. Mother presents at 32 weeks in premature labor. The L/S ratio is 2.3. What is chance of the baby having RDS? Should you halt labor or is it ok for her to deliver? 6 Atelectasis & dilation, hyaline membranes, cell debris on histological exam are characteristic of what newborn disease? The perinatal PKU screen (Guthrie test) on an infant is positive, but only partial deficiency of phenylalanine is present with normal serum levels. What is this called? Will the baby develop stigma? A 7 month infant is reluctant to nurse, is failing to thrive, is vomit & diahhrea, has hepatomegaly, MR, and jaundice. What is the most likely diagnosis? The 4 month old male infant of a poor 16 year-old mother who smokes is found dead in his crib. An investigation rules out fool play. What is the most likely diagnosis? What is the most common location of teratomas? An 11 month old previously health girl presents with present as abdominal mass, fever & wt loss. What is the most likely diagnosis? 25% of the patients described in question 13 have an amplification of which of the following genes? a. 17q b. 1p c. 13q14 d. N-myc A 15 month old boy presents with vision loss, eye pain, and “cat’s eye”. What is the most likely diagnosis? Using the answers to Q14, what is the genetic origin of this disease? Describe the genetic differences between sporadic and familial retinoblastomas. What tumor often recapitulates the stages of nephrogenesis? Answers: 1. C, A, B 2. Disruptions - 2 interference with previously normal organ or region, ex amniotic bands •Sequence - pattern of cascade anomalies, ex. Potter’s sequence: renal agenesis oligohydramnios pulmonary hypoplasia 3. CMV - most common cause of fetal viral infection, can cause MR, deafness, hepatosplenomegaly 4. Hox (homeobox) genes interact with multiple downstream genes, hence is a regulator of morphogenesis, can be affected by retinoids temporal & spatial expression of retionic acid-binding proteins may affect morphogenesis 5. TORCH syndrome: toxoplasma, rubella, cytomegalovirus, herpesvirus and others (syphilis, etc.). –Cause similar clinical & pathological picture in newborn. –Clinical: fever, encephalitis, chorioretinitis, hepatosplenomegaly, pneumonitis, myocarditis, hemolytic anemia, and vesicular or hemorrhagic skin lesions. –Chronic sequelae: growth & learning delays, cataracts, cardiac anomalies and bone defects 6. •excess sedation of mother respiratory depression & brain injury •Prematurity muscle & resp immaturity (1 atelectasis) •Aspiration of blood, mucus, squames, amniotic fluid •Umbilical cord coils hypoxia 7. 5% chances of RDS, she is ok to deliver 8. RDS 9. Benign PKU, no they will not develop stigma 10. Galactosemia 11. SIDS 12. sacrococcygeal 13. Neuroblastoma 14. D 15. retinoblastoma, C 16. •Sporadic 60-70% of cases, require two somatic mutations in same retinoblast •Familial (autosomal dominant) have one germline and one somatic mutation 17. Wilms Tumor