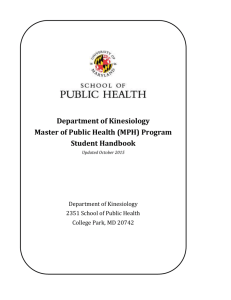
2014-2015 Admitted Student Handbook
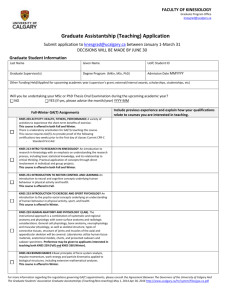
advertisement

MS in Kinesiology 2014-2015 Admitted Student Handbook Revised 5/13 (SA), 9/14 (EAW), 10/14 (EAW), 11/14 (EAW), 02/15 (EAW) Contents Program Description .............................................................................................................................................. 4 Applied Physiology and Neuromechanics Concentration (Thesis required) ................................................. 4 Clinical Exercise Physiology Concentration (Non-thesis) ............................................................................. 4 Programmatic Contacts .......................................................................................................................................... 5 Getting Started ........................................................................................................................................................ 6 Requirements upon Enrollment ...................................................................................................................... 6 University & College Policies ........................................................................................................................ 6 Student Services .............................................................................................................................................. 6 Source of Information and Support................................................................................................................. 6 Things to Know/Get ........................................................................................................................................ 7 Financial Information..................................................................................................................................... 7 Degree Requirements .............................................................................................................................................. 8 Core Courses for Both Concentrations (12 hours) .......................................................................................... 8 Applied Physiology and Neuromechanics Concentration-Specific Courses (15 hours) ................................ 8 Clinical Exercise Physiology Concentration-Specific Courses (18 hours)..................................................... 9 Applied Physiology and Neuromechanics Elective Courses (9 hours) ........................................................ 9 Clinical Exercise Physiology Elective Courses (6 hours).............................................................................. 9 Progression of Classes ......................................................................................................................................... 10 Traditional APN Progression ....................................................................................................................... 10 Traditional CEP Progression........................................................................................................................ 10 Early-Entry APN Progression ..................................................................................................................... 11 Early Entry CEP Progression ....................................................................................................................... 11 Comprehensive Examination ................................................................................................................................ 12 Research Thesis ............................................................................................................................................ 12 General Research Thesis Timeline ............................................................................................................... 13 Registered Clinical Exercise Physiology Exam ............................................................................................ 14 Comprehensive Competency Exam .............................................................................................................. 15 Graduation............................................................................................................................................................. 16 Additional Academic Regulations ........................................................................................................................ 17 Appendix A: KSA Matrix ..................................................................................................................................... 18 2 Appendix B: Practicum Handbook ....................................................................................................................... 30 Welcome ....................................................................................................................................................... 31 Brief History of the Program ........................................................................................................................ 31 How the Clinical experience is incorporated into the program .................................................................... 32 Items to be covered in the Practicum ............................................................................................................ 32 Qualifications of students assigned to Clinical Sites ................................................................................... 33 Assignment of students to Clinical Sites ..................................................................................................... 33 Documents the Clinical Student will keep ................................................................................................. 34 Regulations regarding students .................................................................................................................... 34 Drug Screening and Criminal Background Checks ..................................................................................... 35 Attachment 1 – Practicum Course Syllabus................................................................................................. 37 Attachment 2 – Student Clinical Experience Schedule agreement ............................................................ 41 Attachment 3 – Example format for Student Hour Logbook ...................................................................... 42 Attachment 4 – Example format for Student Clinical Journal .................................................................... 43 Attachment 5 – Preceptor evaluation of Student ......................................................................................... 44 Attachment 6 – ACSM RCEP Code of Ethics ............................................................................................ 46 Attachment 7 – RCEP Scope of Practice ..................................................................................................... 47 Attachment 8 – Drug Screening and Criminal Background Check Form .................................................... 48 Attachment 9 CHHS Clinical Agency Requirements Form ........................................................................ 49 Appendix C: Graduate Assistantship Handbook .................................................................................................. 50 Clauses in all GA Contracts .......................................................................................................................... 51 Graduate Assistant Dress Code Policy ......................................................................................................... 52 KNES Teaching Assistant Dress Code Policy .............................................................................................. 52 Attitude: ........................................................................................................................................................ 55 Teaching Assistant Handbook: ..................................................................................................................... 55 Punctuality: ................................................................................................................................................... 56 External jobs/work: ....................................................................................................................................... 56 Academic Expectations ................................................................................................................................. 56 Notice of Assistantship Status ...................................................................................................................... 57 Appendix D: Certification Opportunities.............................................................................................................. 58 3 Program Description The Master of Science in Kinesiology program prepares graduate students to advance the fields of Kinesiology through evidenced-based patient care and translational research. The program emphasizes basic and clinical interdisciplinary education and research in areas of Kinesiology. The MS in Kinesiology has two concentrations that include a clinical (non-thesis) and research (thesis) degree option. Applied Physiology and Neuromechanics Concentration (Thesis required) The Applied Physiology and Neuromechanics (APN) concentration is excellent preparation for those planning to continue their education through the PhD, either in Kinesiology or a related field (Biology, Rehabilitation Sciences, Biomechanics, Motor Control, Physiology, etc). Students selecting this concentration will also be well qualified for employment in aspects of the health industry or in research labs. Clinical Exercise Physiology Concentration (Non-thesis) The Clinical Exercise Physiology concentration is a CAAHEP-accredited program that is designed to prepare students to become Registered Clinical Exercise Physiologists. Clinical Exercise Physiologists are employed in inpatient and outpatient clinical/rehabilitation settings (e.g. Cardiopulmonary Rehab programs), general wellness/fitness commercial and corporate settings, and industrial settings that provide health care services for both diseased and healthy populations. Through a blend of classroom instruction and clinical experience, the degree program teaches a wide variety of specific health care skills, knowledge, and behaviors within the cardiovascular, pulmonary, metabolic, neoplastic, musculoskeletal, neuromuscular, and immunologic practice areas. Specific Knowledge, Skills, and Abilities (KSAs) associated with the course sequencing can be seen in Appendix A: KSA Matrix. 4 Programmatic Contacts Graduate Program Coordinator Practicum Coordinator Susan Tsivitse Arthur, PhD Dr. Trudy Moore-Harrison Assistant Professor Lecturer Cameron 253 CHHS 328 704-687-0856 704-687-0862 sarthur8@uncc.edu tlmoore2@uncc.edu Department Chair Dr. Scott Gordon Professor and Chair CHHS 335 704-687-0855 scott.gordon@uncc.edu Administrative Support Administrative Support Mrs. Erin Stehmeyer Mrs. Fran Paluso Administrative Support Specialist Administrative Support Specialist CHHS 335 CHHS 335 704-687-0874 704-687-0873 fpaluso@uncc.edu Erin.stehmeyer@uncc.edu A full list of Kinesiology faculty and staff can be found here. Getting Started 5 The following are student services, good information, and/or requirements that students are required to be aware of immediately upon enrollment. Requirements upon Enrollment Immunization Requirements: North Carolina law requires students to have proof of immunizations. These must be provided to the Student Health Center upon registration. Students whose immunizations records are not complete are subject to being withdrawn from their classes. Please see “Immunization Requirements” in the Graduate School section of this Catalog or visit the Student Health Center website for more information. Health Insurance Enrollment or Waiver: Each semester every student must either accept or waive health insurance provided by UNC Charlotte. Your student account will be billed unless you take action to decline the health insurance option. University & College Policies University Regulation of Student Conduct College of Health & Human Services Student Handbook Plagiarism Student Services Disability Services University Center for Academic Excellence Multicultural Academic Services Source of Information and Support Client Services within Information and Technology Services works to ensure that students have access to computer equipment, software, and information. All current students are provided with a NinerNet account that allows access to email, 49er Express, and the University network. Technical support is available through the online helpdesk tool, and via phone at 704-687-5500. The Graduate School J. Murrey Atkins Library Graduate Center Interlibrary Loan International Student/Scholar Office (ISSO) 6 Things to Know/Get The International Student\Scholar Office (ISSO) 49er ID Card Parking Permits Financial Information Tuition & Fees Charges for tuition and fees vary according to the student's status as a resident or non-resident of North Carolina. A non-resident student pays a higher rate of tuition than a legal resident. For more details, see the heading for Residence Status for Tuition Purposes later in this section. We strongly encourage all out-of-state students to immediately work towards earning North Carolina residency. This process should be started immediately upon arrival in North Carolina. Financial Aid: Information on the following programs can be found under financial aid. Graduate Financial Assistance Programs: To be considered for these awards, students must be nominated by their academic department. Awards may consist of Tuition and Health Insurance Grants, Graduate Assistantships, and Fellowships/Scholarships. Graduate Assistantships: Graduate Assistantships are available in the Department of Kinesiology and throughout the university. Graduate assistantships are typically awarded prior to enrollment but students interested in obtaining a graduate assistantship should contact the Graduate Program Coordinator about availability and eligibility. Graduate School Fellowships/Scholarships: There are a number of fellowships that are administered by the Graduate School. If you are interested in these fellowships, please contact the Graduate Program Coordinator since individual graduate programs must determine student eligibility and submit nominations to the Graduate School. Veterans Benefits Children of Veterans 7 Degree Requirements The MS in Kinesiology program adheres to the Master’s Degree Requirements outlined by the Graduate School of UNC Charlotte. Both concentrations within the MS in Kinesiology program require 36 credit hours approved by the Department of Kinesiology and a minimum of 15 credit hours presented for the degree must be in the courses numbered 6000 and above. Both concentrations require the same 12 hours of core courses but differ in their specific concentration courses and the number of elective hours. Courses for which undergraduate credit has been awarded may not be repeated for graduate credit. Early-Entry students must submit an Earlyhttp://graduateschool.uncc.edu/sites/graduateschool.uncc.edu/files/media/Funding/Early-Entry-ProgramForm-2013.pdfEntry Program Form to allow up to 12 graduate credit hours to be counted towards both the MS in Kinesiology and the student’s undergraduate degree. A minimum grade point average of 3.0 is required on all coursework attempted for the degree or they will be dismissed from the program. Similarly, a student who earns to “C” grades will be dismissed from the program. At the time of admission, up to 6 credit hours of graduate transfer credit may be accepted if approved by the Department of Kinesiology and the Graduate School. Core Courses for Both Concentrations (12 hours) KNES 6115 Research Methods in Kinesiology (3) KNES 6232 Physiology of Human Aging (3) KNES 6280 Advanced Exercise Physiology (3) KNES 6285 Advanced Cardiopulmonary Physiology (3) Applied Physiology and Neuromechanics Concentration-Specific Courses (15 hours) ____ XXXX A graduate level statistics course (3) KNES 6170 Neuromechanics of Gait and Posture (3) KNES 6800 Directed Independent Study (3) 8 KNES 6900 Research & Thesis in Kinesiology (6) Clinical Exercise Physiology Concentration-Specific Courses (18 hours) KNES 6120 Advances in Clinical Exercise Physiology (3) KNES 6121 Clinical Practice in Exercise Physiology (3) KNES 6134 Exercise Prescription for Cardiopulmonary and Metabolic Disorders (3) KNES 6151 Exercise Testing Methods (3) KNES 6292 Exercise Prescription for Musculoskeletal Disorders (3) KNES 6490 Advanced Practicum in Clinical Exercise Physiology (1) (taken 3 times) Each Practicum credit is equivalent to 200 clinical hours. Clinical practicum courses usually begin in the third semester of the student’s program and are arranged through the Practicum Coordinator within the Department of Kinesiology. For further information regarding the Advanced Practicum courses and their requirements, please see Appendix B: Practicum Handbook. Applied Physiology and Neuromechanics Elective Courses (9 hours) Clinical Exercise Physiology Elective Courses (6 hours) Below is a list of electives taken by previous students but any graduate course can be counted toward the MS degree as long as two conditions are met: 1) the student’s advisor approves the course prior to course registration and 2) the course allows for at least 15 hours of course credit to be at the 6000 level as outlined in Degree Requirements above. KNES 6260 Clinical Exercise Nutrition (3) KNES 6800 Directed Independent Study (3) HLTH 5299 Epidemiology (3) HLTH 6222 Health Promotion Analysis (3) BIOL 5171 Cell Physiology (3) BIOL 5199 Molecular Biology (3) 9 BIOL 5260 BIOL 6050 Population Genetics (3) BIOL 6050 Pathophysiology (Special topics) (3) Advanced Human Physiology (Special Topics) (3) 10 Progression of Classes Traditional APN Progression st Spring: 1st year Fall: 1 year KNES 6115 Research Methods 3cr KNES 6280 Advanced Exercise Physiology 3cr KNES 6170 Neuromechanics of Gait & Posture 3cr KNES 6800 Independent Study 3cr KNES 5232 Physiology of Human Aging 3cr Elective 3cr Fall: 2nd year KNES 6900 Spring: 2nd year Graduate Statistics course 3cr KNES 6285 Advanced Cardiopulmonary Physiology 3cr Thesis 3cr KNES 6900 Thesis 3cr Elective 3cr Elective 3cr Traditional CEP Progression st Spring: 1st year Fall: 1 year KNES Research Methods 3cr 6115 KNES Advances in Clinical Exercise 3cr 6120 Physiology Elective 3cr Fall: 2nd year KNES 6280 KNES 6134 KNES 6151 Summer: 1st year Advanced Exercise Physiology 3cr Exercise Prescription for Cardiac and Metabolic Disorders Exercise Testing Methods 3cr Spring: 2nd year 3cr KNES Exercise Prescription for 6292 Musculoskeletal Disorders KNES Advanced Practicum 6490 3cr 1cr KNES Clinical Practice in Exercise 3cr KNES Advanced Cardiopulmonary 6121 Physiology 6285 Physiology KNES Physiology of Human Aging 3cr KNES Advanced Practicum 5232 6490 KNES Advanced Practicum 1cr Elective* 6490 * If the student is completing a thesis, it is recommended to take KNES 6900: Thesis. 3cr 1cr 3cr Revised 5/13 (SA), 9/14 (EAW), 10/14 (EAW), 11/14 (EAW), 02/15 (EAW) Early-Entry APN Progression st Spring: 1st year Fall: 1 year KNES 6115 KNES 6170 UG** Research Methods Neuromechanics of Gait & Posture KNES 4121, KNES 4286, KNES 4293 Fall: 2nd year 3cr 3cr 9cr KNES 6280 KNES 6800 UG** Advanced Exercise Physiology Independent Study KNES 3900 Spring: 2nd year 3cr 3cr 3cr KNES 5232 KNES 6900 Physiology of Human Aging 3cr KNES 6285 Advanced Cardiopulmonary Physiology 3cr Thesis 3cr KNES 6900 Thesis 3cr Graduate Statistics course 3cr Elective 3cr Elective 3cr Elective 3cr ** The courses listed here are an example aduate only. All early-entry students must consult with both the Graduate and their Undergraduate Program Coordinator to determine which undergr courses can be substituted. Those listed here are for Exercise Science students. Early Entry CEP Progression st Spring: 1st year Fall: 1 year KNES Research Methods 6115 3cr KNES 6280 Advanced Exercise Physiology Summer: 1st year 3cr KNES Exercise Prescription for 6292 Musculoskeletal Disorders 3cr KNES Advances in Clinical Exercise 3cr 6120 Physiology UG** KNES 4121, KNES 4286, 9cr KNES 4293 Fall: 2nd year KNES 6134 UG** KNES 6121 KNES 5232 KNES 6490 KNES 6285 KNES 6490 KNES 6151 Clinical Practice in Exercise Physiology Physiology of Human Aging 3cr Advanced Practicum 1cr Elective 3cr 3cr Exercise Prescription for Cardiac and Metabolic Disorders KNES 3900 3cr KNES Advanced Practicum 6490 3cr Spring: 2nd year Advanced Cardiopulmonary Physiology Advanced Practicum 3cr Exercise Testing Methods 3cr Elective* 3cr 1cr * If the student is completing a thesis, it is recommended to take KNES 6900: Thesis. ** The courses listed here are an example only. All earlyentry students must consult with both the Graduate and their Undergraduate Program Coordinator to determine which undergraduate courses can be substituted. Those listed here are for Exercise Science students. 11 1cr Comprehensive Examination All candidates for the degree must pass a comprehensive examination as outlined by the Graduate School at UNC Charlotte. A student selecting the Applied Physiology and Neuromechanics concentration must present credit for at least 6 credit hours of KNES 6900 and pass a thesis defense. A student selecting the Clinical Exercise Physiology concentration has two options: 1) present credit for at least 3 credit hours of KNES 6900 and pass a thesis defense, 2) must pass the Registered Clinical Exercise Physiologist examination (RCEP), administered by the American College of Sports Medicine, or 3) must pass a faculty driven competency exam. Please note that this option is only available for CEP students and only having failed the RCEP exam multiple times. The thesis and non-thesis approaches are designed to meet the needs of students preparing for different types of careers and represent qualitatively different educational experiences. Consequently, the Department of Kinesiology and the Dean of the Graduate School strongly discourage any switching from one concentration to another. Such a switch almost always delays graduation. If a switch from the APN or CEP concentration is approved, the grade of I for any thesis work completed will be changed to W on the transcript with no refund of tuition for the course(s) as outlined under the Thesis section of the UNC Charlotte Graduate Catalog. Research Thesis Work on the Research Thesis begins in the student’s first semester and will culminate in a thesis defense during their final semester of enrollment. Throughout this process, there are a number of soft and hard deadlines to consider as well as a number of forms that must be completed. Below is a general timeline, designed for fulltime students graduating in a spring term, but the exact dates of many of the below deadlines will be established by the student and his/her thesis advisor. Students who fail to make satisfactory progress on their thesis may be dropped by their advisor. If a student is dropped, they will have 1 academic month to find a new advisor. If a new advisor cannot be found, the student will be removed from the program at the end of the current term. Revised 5/13 (SA), 9/14 (EAW), 10/14 (EAW), 11/14 (EAW), 02/15 (EAW) General Research Thesis Timeline Thesis milestone Initial formulation of thesis topic (in consultation with thesis advisor) Formulation of specific thesis question(s)/aim(s) Establishment of thesis committee (in consultation with thesis advisor) Complete draft of Chapters 1, 2, and 3 of the thesis Pre-proposal meeting with thesis committee (if working on a novel project) Submit IRB or IACUC protocols for approval (if needed). ** Ethics board approval is now needed prior to the submission of the topic approval form.** Schedule Proposal Meeting with full committee -Materials should be distributed to the committee at least 10-working days in advance of the meeting. -Materials should be formatted according to the Graduate School guidelines. -Bring the Petition for Topic Approval Form -If a committee member is participating from a remote location, bring the Remote Participation Form. Start data collection Recommend deadline No later than 3rd week of 1st fall term. No later than mid-October of the 1st fall term. No later than November of the 1st fall term. End of 1st fall term. No later than early February of the 1st spring term. No later than early-March of the 1st spring term. No later than the end of the 1st spring term. No later than the 3rd week of the 2nd fall term Complete data collection No later than the 3rd week of the 2nd spring term. Complete data analysis No later than the 5th week of the 2nd spring term. Schedule a pre-defense formatting consultation with the Graduate School. Usually mid-April. See the **This is to check for formatting accuracy only. The thesis can still be in draft Official Academic Calendar format.** for the exact date. Schedule Defense Meeting with full committee Defense deadline is usually -Materials should be distributed to the committee at least 10-working the last day of classes for the days in advance of the meeting. spring term. See the Official -Materials should be formatted according to the Graduate School Academic Calendar for the guidelines. exact date. -Bring the Defense Report Form -Bring the ETD Signature Form 15 -If a committee member is participating from a remote location, bring the Remote Participation Form. Schedule a post-defense formatting consultation with the Graduate School if Usually early-May. See the needed. Official Academic Calendar for the exact date. Submit the thesis document via the electronic submission system. -Submit Usually early-May. See the Binding Instructions Official Academic Calendar for the exact date. Celebrate! Registered Clinical Exercise Physiology Exam For those CEP students that choose not to do a thesis, the comprehensive exam is the Registered Clinical Exercise Physiologist examination (RCEP), administered by the American College of Sports Medicine. Passing the RCEP examination will earn the student the Registered Clinical Exercise Physiologist credential upon graduation. An application must be submitted during the student’s last semester before graduation, usually in conjunction with their 3rd practicum (KNES 6490) course. The student may need a letter from the Graduate Coordinator confirming your enrollment in our program and your timeline to graduation since ACSM requires a Master’s Degree to sit for the exam. Upon approval (usually takes 3-4 weeks), they will receive a voucher number and can register to take the exam. The student may take the RCEP exam as many times as needed but please be aware that ACSM requires a 2 week sit-time between each test attempt. Additionally, the exam costs $239 for ACSM members and $299 for non-members. Retests cost $155.50. The RCEP exam is a national certification exam and as such requires adequate preparation. Data from past students has demonstrated that successful completion of the CEP didactic and practicum coursework prepares the student for the exam but additional preparation is needed and should be started no later than 3 months prior to the scheduled test date. The MS in Kinesiology program recommends using the ACSM Resource Manual for Guidelines for Exercise Testing and Prescription as an exam preparation guide. Additional preparation materials can be seen below: ACSM’s Resources for Clinical Exercise Physiology, 2nd Edition 16 ACSM’s Resource Manual for Guidelines for Exercise Testing and Prescription, 6th Edition ACSM’s Guidelines for Exercise Testing and Prescriptions, 8th Edition ACSM’s Exercise Management for Person’s with Chronic Diseases and Disabilities, 3rd Edition The RCEP must be passed by the last day of classes for the spring term. For Summer term, the last day to take the RCEP exam is the last day of class prior to finals. See the Official Academic Calendar for the exact date. Upon passing the exam, CEP students must complete the Report of Comprehensive Exam form. Comprehensive Competency Exam Should a CEP student fail the RCEP examination multiple times, the student has an option to take a comprehensive competency examination prepared by the faculty. The student has one attempt to take the faculty-prepared comprehensive exam. The faculty-driven comprehensive exam is not available during the Summer term. The competency exam is an 8 hr, one-day exam in which the student is given 1 question from each of the core courses taken. Responses are graded by the instructors who teach the respective course. Failing the faculty-prepared comprehensive competency exam, the student will be dismissed from the MS in Kinesiology program. If a student chooses to pursue this option, they must allow at least four-weeks from when they notify the Graduate Program Coordinator of their intent and the date that the exam can be taken. The latest that the student can take the faculty-driven comprehensive competency exam is week 15 of the semester (to allow for grading prior to Graduate School deadlines). The faculty driven competency exam must be passed (graded) by the last day of classes for the spring term. See the Official Academic Calendar for the exact date. Upon passing the exam, the student must complete the Report of Comprehensive Exam form. Graduation The following items must be completed prior to graduation: 17 - Application for Candidacy: To apply for candidacy for a graduate certificate, masters, or doctoral degree: log into 49erExpress, select Banner Self-Service, Student Services, Student Records, and Apply for Candidacy for Graduate Students. After completing all sections, the application is printed and taken to the department for the Graduate Coordinator's approval Signature. This should be started on the 1st day of classes during the student’s final term. -Application for Graduation: To apply to graduate with a graduate certificate, masters, or doctoral degree: log into 49erExpress, select Banner Self-Service, Student Services, Student Records, and Online Graduation Application. Click "Continue" if this is the first time a graduation application has been submitted, or "Create a New Application" if one has been submitted previously. After completing all sections, click the "Submit” button. This should be started on the 1st day of classes during the student’s final term. -Exit Survey: An electronic survey will be distributed during the 2nd spring term and must be completed prior to the last day of class to receive final approval for graduation. All answers are anonymous and we want brutal honesty about the courses, program, etc. -Pass or fail, each CEP student must submit their domain scores for each RCEP attempt. -Each CEP student must also conduct an exit interview with the Graduate Coordinator. General information about graduation and the associated fees can be found here. Additional Academic Regulations Advising Information: Upon acceptance into the program, each student is assigned an advisor. For all students in the MS in Kinesiology program, the Graduate Program Coordinator is an advisor. For those in the CEP concentration, the Graduate Program Coordinator is your primary advisor. For those in the APN 18 concentration, the Graduate Program Coordinator is considered your co-advisor with your thesis advisor. Any course substitution and all electives must be approved by the academic advisor. Continuous Registration: Students in graduate degree programs are required to maintain continuous registration (fall and spring semesters) for thesis, dissertation, project, or directed study until work is completed. If you have completed all of the course requirements and Practicums, you may register for the KNES 7999 (Graduate Residency). Complete a graduate petition form to register for the course. Grading Policies: The MS in Kinesiology program follows all grading policies set forth by UNC Charlotte. Please reference the Graduate Catalogue for specific information related to any grading policy questions. The grade of I is assigned at the discretion of the instructor when a student who is otherwise passing has not, due to circumstances beyond his/her control, completed all the work in the course. The missing work must be completed within 12 months (exact date determined by instructor) or the I will be changed to a U. Academic Standing: The MS in Kinesiology program follows all academic standing, suspension, and appeal policies set forth by UNC Charlotte with one exception. Students who receive 2 C’s will be suspended from the program and will need to perform the appeal procedure. University policy requires that no course listed on a master’s student’s candidacy form be older than six years at the time of graduation. Courses that exceed this time limit must be revalidated or retaken. Complete a graduate petition form to request a course revalidation. Letters of Recommendation: Before any faculty or staff member can submit a letter of recommendation on your behalf to potential employers or scholarship agencies, etc a FERPA form must be completed. This form allows the recommender to discuss your academic performance in their classes and general academic information like your GPA. 19 Appendix A: KSA Matrix KSA’s are a list of required competencies to be covered in one or more classes within the CEP concentration. This list is information that is crucial to the practice of clinical exercise physiology, as laid out by our governing body (ACSM). By reviewing this complete list of KSA’s, you will gain a solid understanding of what is to be expected of you throughout the program, as well as what you can expect to learn throughout the program. KSA KSA Description DOMAIN GENERAL POPULATION/CORE: EXERCISE PHYSIOLOGY AND RELATED EXERCISE SCIENCE 1.1.1 Describe the acute responses to aerobic, resistance, and flexibility training on the function of the cardiovascular, respiratory, musculoskeletal, neuromuscular, metabolic, endocrine, and immune systems. 1.1.2 Describe the chronic effects of aerobic, resistance, and flexibility training on the structure and function of the cardiovascular, respiratory, musculoskeletal, neuromuscular, metabolic, endocrine, and immune systems. 1.1.3 Explain differences in typical values between sedentary and trained persons in those with chronic diseases for oxygen uptake, heart rate, mean arterial pressure, systolic and diastolic blood pressure, cardiac output, stroke volume, rate pressure product, minute ventilation, respiratory rate, and tidal volume at rest and during submaximal and maximal exercise. 1.1.4 Describe the physiological determinants of VO2, mVO2, and mean arterial pressure and explain how these determinants may be altered with aerobic and resistance exercise training. 1.1.5 Describe appropriate modifications in the exercise prescription due to environmental conditions in individuals with chronic disease. Explain the health benefits of a physically active lifestyle, the hazards of sedentary behavior, and summarize key 1.1.6 recommendations of US national reports of physical activity (e.g. US Surgeon General, Institute of Medicine, ACSM, AHA) 1.1.7 Explain the physiological adaptations to exercise training that may result in improvement in or maintenance of health, including cardiovascular, pulmonary, metabolic, orthopedic/musculoskeletal, neuromuscular, and immune system health. Course KNES 6280 KNES 6280 KNES 6134, KNES 6280 KNES 6280 KNES 6280 KNES 6120 KNES 6120, KNES 6280, KNES 6134, KNES 6292 1.1.8 Explain the mechanisms underlying the physiological adaptations to aerobic and resistance training including those resulting in changes in or maintenance of maximal and submaximal oxygen consumption, lactate and ventilatory (anaerobic) threshold, myocardial oxygen consumption, heart rate, blood pressure, ventilation (including ventilatory threshold), muscle structure, bioenergetics, and immune function. Revised 5/13 (SA), 9/14 (EAW), 10/14 (EAW), 11/14 (EAW), 02/15 (EAW) 1.1.9 1.1.10 Explain the physiological effects of physical inactivity, including bed rest, and methods that may counteract these effects. Recognize and respond to abnormal signs and symptoms during exercise. DOMAIN GENERAL POPULATION/CORE: PATHOPHYSIOLOGY AND RISK FACTORS 1.2.1 Describe the epidemiology, pathophysiology, risk factors, and key clinical findings of cardiovascular, pulmonary, metabolic, orthopedic/musculoskeletal, neuromuscular, and NIH diseases DOMAIN GENERAL POPULATION/CORE: HEALTH APPRAISAL, FITNESS AND CLINICAL EXERCISE TESTING 1.3.1 Conduct pre-test procedures including: explaining test procedures, obtaining informed consent, obtaining a focused medical history, reviewing results of prior tests and physical exam, assessing disease-specific risk factors, and presenting concise information to other health care providers and third party payers. 1.3.2 1.3.4 Conduct a brief physical examination including evaluation of peripheral edema, measuring blood pressure, peripheral pulses, respiratory rate, and ausculating heart and lung sounds. Calibrate lab equipment used frequently in the practice of clinical exercise physiology (e.g. motorized/computerized treadmill, mechanical cycle ergometer and arm ergometer, electrocardiograph, spirometer, respiratory gas analyzer (Metabolic cart). Administer exercise tests consistent with US nationally accepted standards for testing. 1.3.5 Evaluate contraindications to exercise testing. 1.3.3 21 KNES 6280 KNES 6280 KNES 6285, KNES 6151 KNES 6134, KNES 6280, KNES 6292, KNES 6120 KNES 6121, KNES 6134, KNES 6151, KNES 6120 KNES 6285, KNES 6151 KNES 6134, KNES 6151 KNES 6134, KNES 6151, KNES 6120 KNES 6134, KNES 6292, KNES 6120 1.3.6 Appropriately select and administer functional tests to measure individual outcomes and functional status including the 6 minute walk, Get Up and Go, Berg Balance Scale, Physical Performance Test, etc. 1.3.8 Interpret the variables that may be assessed during clinical exercise testing including maximal oxygen consumption, resting metabolic rate, ventilatory volumes and capacities, respiratory exchange ratio, ratings of perceived exertion and discomfort (chest pain, dyspnea, claudication), ECG, heart rate, blood pressure, rate pressure product, ventilatory (anaerobic) threshold, oxygen saturation, breathing reserve, muscular strength, muscular endurance, and other common measures employed for diagnosis and prognosis of disease. 1.3.9 Determine atrial and ventricular rate from rhythm strip and 12-lead ECG and explain the clinical significance of abnormal atrial or ventricular rate (e.g. tachycardia, bradycardia). 1.3.10 Identify ECG changes associated with drug therapy, electrolyte abnormalities, subendocardial and transmural ischemia, myocardial injury, and infarction, and explain the clinical significance of each. 1.3.11 Identify SA, AV, and bundle branch blocks from a rhythm strip & 12-lead ECG, and explain the clinical significance of each. Identify sinus, atrial, junctional, and ventricular dysrhythmias from a rhythm strip & 12-lead ECG, and explain the clinical significance of each. Determine an individual's pre-test and post-test probability of CHD, identify factors associated with test complications, and apply appropriate precautions to reduce risks to the individual. 1.3.12 1.3.14 1.3.16 Identify probable disease-specific endpoints for testing in an individual with cardiovascular, pulmonary, metabolic, orthopedic/musculoskeletal, neuromuscular, and NIH disease. 1.3.17 Select and employ appropriate techniques for preparation and measurement of ECG, heart rate, blood pressure, oxygen saturation, RPE, symptoms, expired gases, and other measures as needed before, during, and following exercise testing. 22 KNES 5232, KNES 6134, KNES 6120, KNES 6151 KNES 6134, KNES 6285, KNES 6280, KNES 6120 KNES 6285, KNES 6134, KNES 6151 KNES 6285, KNES 6151, KNES 6134 KNES 6285, KNES 6151 KNES 6285, KNES 6151 KNES 6134, KNES 6285, KNES 6120 KNES 6292, KNES 6134, KNES 6285, KNES 6151, KNES 6120 KNES 6134, KNES 6285, KNES 6151, KNES 6120 1.3.18 1.3.19 Select and administer appropriate exercise tests to evaluate functional capacity, strength, and flexibility in individuals with cardiovascular, pulmonary, metabolic, orthopedic/musculoskeletal, neuromuscular, and NIH disease. Discuss strengths and limitations of various methods of measures and indices of body composition. 1.3.20 Appropriately select, apply, and interpret body composition tests and indices. 1.3.21 Discuss pertinent test results with other health care professionals. DOMAIN GENERAL POPULATION/CORE: EXERCISE PRESCRIPTION AND PROGRAMMING 1.7.3 Determine the appropriate level of supervision and monitoring recommended for individuals with known disease based on disease-specific risk stratification guidelines and current health status. 1.7.4 Develop, adapt, and supervise appropriate aerobic, resistance, and flexibility training for individuals with cardiovascular, pulmonary, metabolic, orthopedic/musculoskeletal, neuromuscular, and NIH disease. 1.7.6 Instruct individuals with cardiovascular, pulmonary, metabolic, orthopedic/musculoskeletal, neuromuscular, and NIH disease in techniques for performing physical activities safely and effectively in an unsupervised exercise setting. Modify the exercise prescription or discontinue exercise based upon individual symptoms, current health status, musculoskeletal limitations, and environmental considerations. 1.7.7 1.7.8 Extract and interpret clinical information needed for safe exercise management of individuals with cardiovascular, pulmonary, metabolic, orthopedic/musculoskeletal, neuromuscular, and NIH disease. 1.7.9 Evaluate individual outcomes from serial outcome data collected before, during, and after exercise interventions. DOMAIN GENERAL POPULATION/CORE: 23 KNES 6292, KNES 6134, KNES 6120 KNES 6120, KNES 6151 KNES 6120, KNES 6151 KNES 6121, KNES 6490 KNES 6121, KNES 6134, KNES 6120, KNES 6292 KNES 6120, KNES 6134, KNES 6292 KNES 6120, KNES 6134, KNES 6292 KNES 6120, KNES 6134, KNES 6292 KNES 6134, KNES 6292, KNES 6120 KNES 6134, KNES 6292, KNES 6120 HUMAN BEHAVIOR AND COUNSELING 1.9.1 1.9.2 1.9.3 Summarize contemporary theories of health behavior change including social cognitive theory, theory of reasoned action, theory of planned behavior, transtheoretical model, health belief model, and apply techniques to promote healthy behaviors including physical activity. Describe characteristics associated with poor adherence to exercise programs. Describe the psychological issues associated with acute and chronic illness such as anxiety, depression, social isolation, hostility, aggression, and suicidal ideation. 1.9.4 Counsel individuals with cardiovascular, pulmonary, metabolic, orthopedic/musculoskeletal, neuromuscular, and NIH disease on topics such as disease processes, treatments, diagnostic techniques, and lifestyle management. 1.9.6 Explain factors that may increase anxiety prior to or during exercise testing and describe methods to reduce anxiety. 1.9.7 Recognize signs and symptoms of failure to cope during personal crises such as job loss, bereavement, and illness. DOMAIN GENERAL POPULATION/CORE: SAFETY, INJURY PREVENTION, AND EMERGENCY PROCEDURES 1.10.1 List routine emergency equipment, drugs, and supplies present in an exercise testing laboratory and therapeutic exercise session area. 1.10.2 Provide immediate responses to emergencies including basic cardiac life support, AED, activation of EMS, and joint immobilization. 1.10.3 Verify operating status of emergency equipment including defibrillator, laryngoscope, oxygen, etc. 1.10.4 1.10.5 1.10.6 DOMAIN 1.11.1 1.11.2 Explain Universal Precautions procedures and apply as appropriate. Develop and implement a plan for responding to emergencies. Knowledge of advanced cardiac life support procedures. GENERAL POPULATION/CORE: PROGRAM ADMINISTRATION, QUALITY ASSURANCE AND OUTCOME ASSESSMENT Describe appropriate staffing for exercise testing and programming based on factors such as individual health status, facilities, and program goals. List necessary equipment and supplies for exercise testing and programs. 24 KNES 6121 KNES 6121 KNES 6121, KNES 6120, KNES 5232 KNES 6120, KNES 6134, KNES 6292 KNES 6134, KNES 6151 KNES 6121 KNES 6121 KNES 6121 KNES 6121 KNES 6121 KNES 6121 KNES 6121 KNES 6121 KNES 6121, KNES 6151 1.11.3 Select, evaluate, and report treatment outcomes using individual-relevant results of tests and surveys. 1.11.4 Explain legal issues pertinent to health care delivery by licensed and non-licensed health care professionals providing rehabilitative services and exercise testing and legal risk management techniques . Identify individuals requiring referral to a physician or allied health services such as physical therapy, dietary counseling, stress management, weight management, and psychological and social services. 1.11.5 1.11.6 Develop a plan for individual discharge from therapeutic exercise program, including community referrals. DOMAIN CARDIOVASCULAR: EXERCISE PHYSIOLOGY AND RELATED EXERCISE SCIENCE 2.1.2 Describe the potential benefits and hazards of aerobic, resistance, and flexibility training in individuals with cardiovascular diseases. 2.1.4 Explain how cardiovascular diseases may affect the physiologic responses to aerobic and resistance training. 2.1.5 Describe the immediate and long-term influence of medical therapies for cardiovascular diseases on the responses to aerobic and resistance training. DOMAIN CARDIOVASCULAR: PATHOPHYSIOLOGY AND RISK FACTORS 2.2.1 Describe the epidemiology, pathophysiology, rate of progression of disease, risk factors, and key clinical findings of cardiovascular diseases. 2.2.2 Explain the ischemic cascade and its effect on myocardial function. 2.2.4 Explain methods of reducing risk in individuals with cardiovascular diseases. 25 KNES 6120, KNES 6134, KNES 6121, KNES 6292 KNES 6120, KNES 6121 KNES 6121, KNES 6134, KNES 6120 KNES 6121 KNES 6134 KNES 6134, KNES 6280, KNES 6285 KNES 6134 KNES 5232, KNES 6285, KNES 6134, KNES 6280 KNES 5232, KNES 6285, KNES 6134, KNES 6280 KNES 6285, KNES 6134 DOMAIN CARDIOVASCULAR: HEALTH APPRAISAL, FITNESS AND CLINICAL EXERCISE TESTING 2.3.1 Describe common techniques used to diagnose cardiovascular disease, including graded exercise testing, echocardiography, radionuclide imaging, angiography, pharmacologic testing, and biomarkers (e.g., Troponin, CK, etc), and explain the indications, limitations, risks, and normal and abnormal results for each. 2.3.2 Explain how cardiovascular disease may affect physical examination findings. 2.3.4 Recognize and respond to abnormal signs and symptoms in individuals with cardiovascular diseases such as pain, peripheral edema, dyspnea, fatigue. 2.3.5 Conduct and interpret appropriate exercise testing methods for individuals with cardiovascular diseases. DOMAIN CARDIOVASCULAR: MEDICAL AND SURGICAL MANAGEMENT 2.6.2 Explain the common medical and surgical treatments of cardiovascular diseases. 2.6.3 2.6.4 2.6.5 Apply key recommendations of current U.S. clinical practice guidelines for the prevention, treatment, and management of cardiovascular diseases (e.g., AHA, ACC, NHLBI). List the commonly used drugs (generic and brand names) in the treatment of individuals with cardiovascular diseases, and explain the indications, mechanisms of actions, major side effects, and the effects on the exercising individual. Explain how treatments for cardiovascular disease, including preventive care, may affect the rate of progression of disease. DOMAIN CARDIOVASCULAR: EXERCISE PRESCRIPTION AND PROGRAMMING 2.7.2 Design, adapt, and supervise an appropriate Exercise Prescription (e.g. aerobic, resistance, and flexibility training) for individuals with cardiovascular diseases. 26 KNES 6285, KNES 6134 KNES 6285, KNES 6134 KNES 6134, KNES 6285, KNES 6151 KNES 6134, KNES 6151, KNES 6285 KNES 6121, KNES 6285, KNES KNES 6121, KNES 6134 KNES 6121, KNES 6134 KNES 6121, KNES 6285, KNES 6134 KNES 6134 2.7.4 2.7.5 Instruct an individual with cardiovascular disease in techniques for performing physical activities safely and effectively in an unsupervised setting. Counsel individuals with cardiovascular disease on the proper uses of sublingual nitroglycerin. DOMAIN PULMONARY: (e.g. Obstructive and Restrictive Lung Diseases) EXERCISE PHYSIOLOGY AND RELATED EXERCISE SCIENCE 3.1.1 Describe the potential benefits and hazards of aerobic, resistance, and flexibility training in individuals with pulmonary diseases. 3.1.2 Explain how pulmonary diseases may affect the physiologic responses to aerobic, resistance, and flexibility training. 3.1.3 3.1.5 Explain how scheduling of exercise relative to meals can affect dyspnea Describe the immediate and long-term influence of medical therapies for pulmonary diseases on the responses to aerobic, resistance, and flexibility training. DOMAIN PULMONARY: PATHOPHYSIOLOGY AND RISK FACTORS 3.2.1 Describe the epidemiology, pathophysiology, rate of progression of disease, risk factors, and key clinical findings of pulmonary diseases. 3.2.3 Explain methods of reducing risk in individuals with pulmonary diseases. DOMAIN PULMONARY: HEALTH APPRAISAL, FITNESS AND CLINICAL EXERCISE TESTING 3.3.1 Explain how pulmonary disease may affect physical examination findings. 3.3.3 Have knowledge of lung volumes and capacities (e.g., tidal volume, residual volume, inspiratory volume, expiratory volume, total lung capacity, vital capacity, functional residual capacity, peak flow rate, diffusion capacity) and how they may differ between normals and individuals with pulmonary disease. 3.3.4 Recognize and respond to abnormal signs and symptoms to exercise in individuals with pulmonary diseases. 3.3.5 Describe common techniques and tests used to diagnose pulmonary diseases, and explain the indications, limitations, risks, and normal and abnormal results for each. 3.3.6 Conduct and interpret appropriate exercise testing methods for individuals with pulmonary diseases. DOMAIN PULMONARY: MEDICAL AND SURGICAL MANAGEMENT 27 KNES 6134, KNES 6280 KNES 6134, KNES 6121 KNES 6280, KNES 6134 KNES 6280, KNES 6134 KNES 6285 KNES 6134 KNES 5232, KNES 6285, KNES 6134 KNES 6134 KNES 6134 KNES 6285, KNES 6134, KNES 6280 KNES 6285, KNES 6134 KNES 6134 KNES 6134 3.6.3 Explain how treatments for pulmonary disease, including preventive care, may affect the rate of progression of disease. 3.6.5 3.6.6 Explain the common medical and surgical treatments of pulmonary diseases. List the commonly used drugs (generic and brand names) in the treatment of individuals with pulmonary diseases, and explain the indications, mechanisms of actions, major side effects, and the effects on the exercising individual. 3.6.7 Apply key recommendations of current U.S. clinical practice guidelines (e.g. ALA, NIH, NHLBI) for the prevention, treatment, and management of pulmonary diseases. DOMAIN PULMONARY: EXERCISE PRESCRIPTION AND PROGRAMMING 3.7.2 Design, adapt, and supervise an appropriate exercise prescription (e.g. aerobic, resistance, and flexibility training) for individuals with pulmonary diseases. 3.7.4 Instruct an individual with pulmonary diseases in proper breathing techniques and exercises and methods for performing physical activities safely and effectively. 3.7.5 Knowledge of the use of supplemental oxygen during exercise and its influences on exercise tolerance. DOMAIN METABOLIC: (e.g. Diabetes, Hyperlipidemia, Obesity, Frailty, Chronic Renal Failure, Metabolic Syndrome) EXERCISE PHYSIOLOGY AND RELATED EXERCISE SCIENCE 4.1.1 Explain how metabolic diseases may affect aerobic endurance, muscular strength and endurance, flexibility, and balance. 4.1.2 Describe the immediate and long-term influence of medical therapies for metabolic diseases on the responses to aerobic, resistance, and flexibility training. 4.1.3 Describe the potential benefits and hazards of aerobic, resistance, and flexibility training in individuals with metabolic diseases. DOMAIN METABOLIC: PATHOPHYSIOLOGY AND RISK FACTORS 4.2.1 Describe the epidemiology, pathophysiology, rate of progression of disease, risk factors, and key clinical findings of metabolic diseases. 4.2.5 Describe the probable effects of dialysis treatment on exercise performance, functional capacity, and safety, and explain methods for preventing adverse effects 28 KNES 6285, KNES 6134 KNES 6134 KNES 6134, KNES 6121 KNES 6134, KNES 6121 KNES 6134 KNES 6134 KNES 6134, KNES 6285, KNES 6280 KNES 6134 KNES 6134 KNES 6134 KNES 6134 KNES 6134 4.2.6 Describe the probable effects of hypo/hyperglycemia on exercise performance, functional capacity, and safety, and explain methods for preventing adverse effects 4.2.7 Explain methods of reducing risk in individuals with metabolic diseases. DOMAIN METABOLIC: HEALTH APPRAISAL, FITNESS AND CLINICAL EXERCISE TESTING 4.3.1 Describe common techniques and tests used to diagnose metabolic diseases, and explain the indications, limitations, risks, and normal and abnormal results for each. 4.3.3 Explain appropriate techniques for monitoring blood glucose before, during, and after an exercise session. 4.3.4 Recognize and respond to abnormal signs and symptoms in individuals with metabolic diseases. 4.3.5 Conduct and interpret appropriate exercise testing methods for individuals with metabolic diseases. DOMAIN METABOLIC: MEDICAL AND SURGICAL MANAGEMENT KNES 6280, KNES 6134 KNES 6134 4.6.2 KNES 6121 4.6.3 4.6.4 4.6.5 Apply key recommendations of current U.S. clinical practice guidelines (e.g. ADA, NIH, NHLBI) for the prevention, treatment, and management of metabolic diseases Explain the common medical and surgical treatments of metabolic diseases. List the commonly used drugs (generic and brand names) in the treatment of individuals with metabolic diseases, and explain the indications, mechanisms of actions, major side effects, and the effects on the exercising individual. Explain how treatments for metabolic diseases, including preventive care, may affect the rate of progression of disease. DOMAIN METABOLIC: EXERCISE PRESCRIPTION AND PROGRAMMING 4.7.2 Design, adapt, and supervise an appropriate Exercise Prescription (e.g. aerobic, resistance, and flexibility training) for individuals with metabolic diseases. 4.7.4 Instruct individuals with metabolic diseases in techniques for performing physical activities safely and effectively in an unsupervised exercise setting. 4.7.5 Adapt the exercise prescription based on the functional limits and benefits of assistive devices (e.g. wheelchairs, crutches, and canes). 29 KNES 6134 KNES 6134 KNES 6134 KNES 6134 KNES 6120, KNES 6121, KNES 6134 KNES 6121, KNES 6134 KNES 6121, KNES 6134 KNES 6134 KNES 6134 KNES 6134 DOMAIN ORTHOPEDIC/MUSCULOSKELETAL: (e.g. low back pain, osteoarthritis, rheumatoid arthritis, osteoporosis, amputations, vertebral disorders) EXERCISE PHYSIOLOGY AND RELATED EXERCISE SCIENCE 5.1.1 Describe the potential benefits and hazards of aerobic, resistance, and flexibility training in individuals with orthopedic/musculoskeletal diseases. 5.1.4 Explain how orthopedic/musculoskeletal diseases may affect aerobic endurance, muscular strength and endurance, flexibility, balance, and agility. 5.1.5 Describe the immediate and long-term influence of medical therapies for orthopedic/musculoskeletal diseases on the responses to aerobic, resistance, and flexibility training. DOMAIN ORTHOPEDIC/MUSCULOSKELETAL: PATHOPHYSIOLOGY AND RISK FACTORS 5.2.1 Describe the epidemiology, pathophysiology, risk factors, and key clinical findings of orthopedic/musculoskeletal diseases. DOMAIN ORTHOPEDIC/MUSCULOSKELETAL: HEALTH APPRAISAL, FITNESS AND CLINICAL EXERCISE TESTING 5.3.1 Recognize and respond to abnormal signs and symptoms to exercise in individuals with orthopedic/musculoskeletal diseases. 5.3.2 Describe common techniques and tests used to diagnose orthopedic/musculoskeletal diseases. 5.3.3 Conduct and interpret appropriate exercise testing methods for individuals with orthopedic/musculoskeletal diseases. DOMAIN ORTHOPEDIC/MUSCULOSKELETAL: MEDICAL AND SURGICAL MANAGEMENT 5.6.1 List the commonly used drugs (generic and brand names) in the treatment of individuals with orthopedic/musculoskeletal diseases, and explain the indications, mechanisms of actions, major side effects, and the effects on the exercising individual. 5.6.2 Explain the common medical and surgical treatments of orthopedic/musculoskeletal diseases. 5.6.3 Apply key recommendations of current U.S. clinical practice guidelines (e.g. NIH, National Osteoporosis Foundation, Arthritis Foundation) for the prevention, treatment and management of orthopedic/musculoskeletal diseases. 5.6.4 Explain how treatments for orthopedic/musculoskeletal disease may affect the rate of progression of disease. DOMAIN ORTHOPEDIC/MUSCULOSKELETAL: EXERCISE PRESCRIPTION AND PROGRAMMING 30 KNES 6292 KNES 6292 KNES 6292 KNES 5232, KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6121, KNES 6292 KNES 6292 KNES 6292 KNES 6292 5.7.1 Explain exercise training concepts specific to industrial or occupational rehabilitation, which includes work hardening, work conditioning, work fitness, and job coaching. 5.7.2 Design, adapt, and supervise an appropriate Exercise Prescription (e.g. aerobic, resistance, and flexibility training) for individuals with orthopedic/musculoskeletal diseases. 5.7.3 Instruct an individual with orthopedic/musculoskeletal disease in techniques for performing physical activities safely and effectively in an unsupervised exercise setting. 5.7.4 Adapt the Exercise Prescription based on the functional limits and benefits of assistive devices (e.g. wheelchairs, crutches, and canes). DOMAIN NEUROMUSCULAR: EXERCISE PHYSIOLOGY AND RELATED EXERCISE SCIENCE 6.1.1 Describe the potential benefits and hazards of aerobic, resistance, and flexibility training in individuals with neuromuscular diseases. 6.1.4 Explain how neuromuscular diseases may affect aerobic endurance, muscular strength and endurance, flexibility, balance, and agility. 6.1.5 Describe the immediate and long-term influence of medical therapies for neuromuscular diseases on the responses to aerobic, resistance, and flexibility training. DOMAIN NEUROMUSCULAR: PATHOPHYSIOLOGY AND RISK FACTORS 6.2.1 Describe the epidemiology, pathophysiology, risk factors, and key clinical findings of neuromuscular diseases. DOMAIN NEUROMUSCULAR: HEALTH APPRAISAL, FITNESS AND CLINICAL EXERCISE TESTING 6.3.1 Recognize and respond to abnormal signs and symptoms to exercise in individuals with neuromuscular diseases. 6.3.2 Describe common techniques and tests used to diagnose neuromuscular diseases. 6.3.3 Conduct and interpret appropriate exercise testing methods for individuals with neuromuscular diseases. DOMAIN NEUROMUSCULAR: MEDICAL & SURGICAL MANAGEMENT 6.6.1 Explain the common medical and surgical treatments of neuromuscular diseases. 6.6.2 List the commonly used drugs (generic and brand names) in the treatment of individuals with neuromuscular disease, and explain the indications, mechanisms of actions, major side effects, and the effects on the exercising individual. 31 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6292 6.6.3 6.6.4 DOMAIN 6.7.1 6.7.3 6.7.4 DOMAIN 7.1.1 7.1.2 7.1.3 DOMAIN 7.2.1 DOMAIN 7.3.1 7.3.2 7.3.3 DOMAIN 7.6.1 7.6.2 Apply key recommendations of current U.S. clinical practice guidelines (e.g. NIH) for the prevention, treatment and management of neuromuscular diseases. Explain how treatments for neuromuscular disease may affect the rate of progression of disease. NEUROMUSCULAR: EXERCISE PRESCRIPTION AND PROGRAMMING Adapt the Exercise Prescription based on the functional limits and benefits of assistive devices (e.g. wheelchairs, crutches, and canes). Design, adapt, and supervise an appropriate Exercise Prescription (e.g. aerobic, resistance, and flexibility training) for individuals with neuromuscular diseases. Instruct an individual with neuromuscular diseases in techniques for performing physical activities safely and effectively in an unsupervised exercise setting. NEOPLASTIC, IMMUNOLOGIC, & HEMATOLOGIC: EXERCISE PHYSIOLOGY AND RELATED EXERCISE SCIENCE Explain how NIH diseases may affect the physiologic responses to aerobic, resistance, and flexibility training. Describe the immediate and long-term influence of medical therapies for NIH on the responses to aerobic, resistance, and flexibility training. Describe the potential benefits and hazards of aerobic, resistance, and flexibility training in individuals with NIH diseases. NEOPLASTIC, IMMUNOLOGIC & HEMATOLOGIC: PATHOPHYSIOLOGY AND RISK FACTORS Describe the epidemiology, pathophysiology, risk factors, and key clinical findings of NIH diseases. NEOPLASTIC, IMMUNOLOGIC & HEMATOLOGIC: HEALTH APPRAISAL, FITNESS AND CLINICAL EXERCISE TESTING Recognize and respond to abnormal signs and symptoms to exercise in individuals with NIH diseases. Describe common techniques and tests used to diagnose NIH diseases. Conduct and interpret appropriate exercise testing methods for individuals with NIH diseases. NEOPLASTIC, IMMUNOLOGIC & HEMATOLOGIC: MEDICAL AND SURGICAL MANAGEMENT List the commonly used drugs (generic and brand names) in the treatment of individuals with NIH disease, and explain the indications, mechanisms of actions, major side effects, and the effects on the exercising individual. Apply key recommendations of current U.S. clinical practice guidelines (e.g. ACS, NIH) for the prevention, treatment, and management of NIH diseases. 32 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6292 KNES 6120 KNES 6120 KNES 6120 KNES 6120 KNES 6120 KNES 6120 KNES 6120 KNES 6120, KNES 6121 KNES 6120, KNES 6121 7.6.3 Explain the common medical and surgical treatments of NIH diseases. 7.6.4 Explain how treatments for NIH disease may affect the rate of progression of disease. DOMAIN NEOPLASTIC, IMMUNOLOGIC & HEMATOLOGIC: EXERCISE PRESCRIPTION AND PROGRAMMING 7.7.1 Design, adapt, and supervise an appropriate exercise prescription (e.g. aerobic, resistance, and flexibility training) for individuals with NIH diseases. 7.7.4 Instruct an individual with NIH diseases in techniques for performing physical activities safely and effectively in an unsupervised exercise setting. 33 KNES 6120, KNES 6121 KNES 6120 KNES 6120 KNES 6120 Appendix B: Practicum Handbook Clinical Exercise Physiology program accredited by the Commission on Accreditation of Allied Health Education Programs (CAAHEP) through the American College of Sports Medicine TABLE OF CONTENTS Welcome ....................................................................................................................................................... 35 Brief History of the Program ........................................................................................................................ 35 How the Clinical experience is incorporated into the program .................................................................... 36 Items to be covered in the Practicum ............................................................................................................ 36 Qualifications of students assigned to Clinical Sites .................................................................................... 37 Assignment of students to Clinical Sites ...................................................................................................... 37 Documents the Clinical Student will keep .................................................................................................... 38 Regulations regarding students ..................................................................................................................... 38 Drug Screening and Criminal Background Checks ...................................................................................... 40 Attachment 1 – Practicum Course Syllabus.................................................................................................. 42 Attachment 2 – Student Clinical Experience Schedule agreement .............................................................. 46 Attachment 3 – Example format for Student Hour Logbook ....................................................................... 47 Attachment 4 – Example format for Student Clinical Journal ...................................................................... 48 Attachment 5 – Preceptor evaluation of Student .......................................................................................... 49 Attachment 6 – ACSM RCEP Code of Ethics .............................................................................................. 51 Attachment 7 – RCEP Scope of Practice ...................................................................................................... 52 Attachment 8 – Drug Screening and Criminal Background Check Form .................................................... 52 Attachment 9 CHHS Clinical Agency Requirements Form ........................................................................ 53 Created 9/14 (EAW) Welcome The faculty of Kinesiology believes strongly that an appropriate educational experience, especially one that purports to train clinical practitioners, should have a large clinical component. Therefore, the MS in Kinesiology has a large clinical component. Fulfilling this requirement will mean that you will experience at least 600 clinical hours in a variety of different areas where Clinical Exercise Physiologists practice. The purpose of this handbook is to give an overview of the Practicum (see course syllabus in Attachment 1). While you will see that the Knowledge, Skills and Abilities (KSAs) required will vary by clinical site, the end result of your clinical experience, whether it be 600 or 1200 hours, will be a broad exposure to the common experiences that a Clinical Exercise Physiologist (CEP) will face in practice. We harbor no illusions that this handbook will answer all of your questions. Therefore, we strongly encourage you to maintain contact with both your advisor and Practicum Coordinator. Brief History of the Program The UNC Charlotte Kinesiology program followed the national implementation of the national ACSM Registry of Clinical Exercise Physiologists (RCEP) by implementing a concentration area in CEP within the Health Promotion M.S. degree in 2000. Within two years, the CEP concentration area was attracting 50% of the students in the Health Promotion degree and coupled with a departmental reorganization, it was decided to seek permission to establish a stand-alone Master’s degree program in Kinesiology. After two years of planning and considerable effort on the part of the departmental faculty and the Departmental Advisory Board, the University Faculty Council approved the new program and associated curriculum in April 2004 and in October 2004, the State Board of Governors granted permission to implement a M.S. program in KNES starting in January, 2005. 35 How the Clinical experience is incorporated into the program When designing the MS KNES curriculum, the faculty not only used examples from other universities (e.g. Virginia Tech, University of Florida, and Northeastern) but also suggestions from our Advisory Board. What we heard repeatedly was that integration of practical, clinical experiences with academic learning was critical to the development of a successful Clinical Exercise Physiologist. Therefore, we have incorporated a minimum of 600 hours of clinical experience into the degree program. The clinical experience is delivered in 200 hour segments, with the student receiving a one-academic credit for each segment. These one-hour courses are titled “Practicum” courses and the student is required to take at least three before they are allowed to graduate. The graduate exit survey must be completed at the end of the student’s third practicum in order to receive the practicum grade. Items to be covered in the Practicum The UNC Charlotte MS KNES program was developed to meet the knowledge, skills, and abilities (KSAs) delineated by the American College of Sports Medicine for its Registered Clinical Exercise Physiologist (RCEP) national registry. The RCEP KSAs (see ACSM’s Resources for Clinical Exercise Physiology. Lippincott Williams & Wilkins, Philadelphia, PA) consist of both didactic and experiential items that are split into six (6) practice areas. The KSAs for each practice area that we would like covered within the Practicum experience are listed in Appendix 1: KSA Matrix and can be identified as those taught in KNES 6490. As you will note by perusing these KSAs, they are quite extensive and it is likely that some KSAs will be covered by several sites and some will only be covered by individual clinical sites. IMPORTANT: It is not expected that any one Clinical Site will necessarily cover ALL of the KSAs listed in one practice area. Each clinical site is unique and will deliver specific learning experiences that fall within the KSAs. The Practicum coordinator will meet with the Clinical Preceptor (see next section) at each site to determine the appropriate KSAs for each site. 36 Qualifications of students assigned to Clinical Sites Each student that presents for a Clinical Experience will have the following qualifications: 1. Completion of at least 9 credit hours in the program; 2. Current CPR certification (either Red Cross or American Heart Association); 3. Current professional liability insurance; 4. Current immunizations; 5. Criminal background check; 6. Bloodborne pathogens training. Proof of each of these items will be delivered to the Practicum Coordinator and the Clinical Preceptor on the first day of the student’s clinical experience. NOTE: Some clinical sites also require an additional criminal background check, immunizations, and/or a drug screening. The Clinical Preceptor will notify you of these requirements and then it will be the student’s responsibility to complete these items (i.e. the University is not involved in these requirements). Assignment of students to Clinical Sites One of the program’s goals is to insure that students with appropriate levels of training, professional skill, and demeanor are assigned to each Clinical Site. Whereas students can begin their clinical experiences as early as the second term they are in the program, each student will have a variety of knowledge accumulated regarding Clinical Exercise Physiology. The knowledge level of the student will be factored into the initial determination as will the KSAs each student needs to fulfill. Thus, the following procedure will be used to match each student with a clinical site. 1. Upon determination that the student meets the three qualifications listed above, threefour weeks before the beginning of each academic semester, the Practicum Coordinator (UNC Charlotte) will initially assign each student to a Clinical Site. 2. The student will immediately arrange an interview with the Site Preceptor. 37 3. The Site Preceptor will interview the student and will communicate to the Practicum Coordinator via letter or email, whether they wish to have the student at their site. 4. If the Preceptor approves the student, the student and Preceptor agree upon a start date and the weekly clinical schedule and the Preceptor signs the student’s clinical experience schedule (Attachment 2). Copies of this schedule are then immediately distributed to the student, the preceptor, and the practicum coordinator. 5. The student begins the clinical experience on the agreed upon date. 6. If the Preceptor does not approve the student, the student will be assigned to another clinical site where possible, and if there are available students, another student may be assigned to the Preceptor’s site. Documents the Clinical Student will keep Given that this clinical experience is part of an academic program, we must complete evaluations to determine whether you are making progress in learning the material. Therefore, there are a number of documents that you will be required to keep, in addition to two evaluations we will ask each Preceptor to complete. Each student will be required to maintain and present to the Practicum Coordinator the following documents: 1. A log book of all clinical hours that also contains a brief description of the activities of those hours (example format in Attachment 3); 2. A journal detailing the activities of the clinical experience (example format in Attachment 4); NOTE: Each Preceptor will be asked to complete an evaluation of the student (Attachment 5) midway and at the end of the clinical experience and subsequently submit this evaluation to the Practicum Coordinator. Regulations regarding students It is well understood that the modern health-care setting has a large number of privacy and confidentiality requirements. You as a clinical student are expected to respect and follow those requirements as if you were a professionally practicing Clinical Exercise Physiologist. As such, you are required to abide by all appropriate federal, state, and local laws as well as the RCEP Professional Code of Ethics (Attachment 6) and to work solely within your defined scope of practice (Attachment 7). 38 In addition to these stipulations, when a clinical site agrees to accept you, the clinical site becomes an arm of the University and as such, must treat you in accordance with all aspects of student policies at UNC Charlotte. In particular, the following policies should be noted: 39 1. In general, graduate students (i.e. you) should spend no more than 20 hours per week at the clinical site; 2. You are at the clinical site for educational purposes; tasks given to you should be commensurate with their skill and knowledge level and should contribute directly to the accomplishment of the KSAs of the program; 3. You should not be assigned menial tasks that do not progress you toward fulfillment of the KSAs; 4. Proper interactions with students are governed by student policies at UNC Charlotte (e.g. sexual harassment, student conduct, etc.). These policies can be found at: http://www.legal.uncc.edu/policies/studpol.html. 5. If you are taken advantage of in any way at your Clinical Site, you should immediately notify the Practicum Coordinator. Drug Screening and Criminal Background Checks You should be aware that some clinical sites require drug screening and criminal background checks before you can do a Practicum at that site. These items are your responsibility, much like immunizations, and as such, you should take care of them as quickly as possible. For your information, here is the full policy and the form that you are required to sign and return to me. UNC CHARLOTTE COLLEGE OF HEALTH AND HUMAN SERVICES CRIMINAL BACKGROUND CHECK AND DRUG SCREENING POLICY STUDENT 1. Introduction It is a condition of initial enrollment in the College of Health and Human Services (CHHS) Programs, and a condition of eligibility to continue enrollment, that CHHS students meet all academic and other requirements imposed by CHHS, as well as all requirements of each external health and human service agency where CHHS attempts to place the student in a given semester. CHHS must secure the cooperation of independent external health and human service agencies (“Agencies”) to provide appropriate educational, internship, clinical, or field experiences for its students. Increasingly, those Agencies will not accept students who do not meet requirements that apply to employees at the Agency, including drug tests and criminal background checks. Because criminal background checks are now required by the North Carolina Board of Nursing for all licensure applicants, and because of recommendations from the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), many Agencies now require that CHHS students who will intern at their sites successfully complete criminal background checks and drug screening. Many public and private schools and social services agencies also require criminal background and drug screening of CHHS students who interact with elementary/high school students and social service clients. Thus, in addition to meeting all CHHS academic and other requirements, students have the additional responsibility to meet requirements imposed by each Agency where they will receive clinical or field education, including internships. 35 A student who is rejected by one or more Agencies because of failure to meet that Agency’s criminal background and/or drug testing requirements may be subject to dismissal from the CHHS Program in accordance with the CHHS Academic Dismissal Policy. 2. Agency Criminal Background Check Requirements a. Comply with the criminal background check requirements at each agency to which students are assigned. In some cases, the Agency will facilitate criminal background checks. Students will usually bear all expense associated with meeting these requirements. CHHS will receive notice only that the student has been accepted or rejected by the Agency. If a student is rejected, CHHS will attempt to assign the student to another Agency. If no Agency accepts a student, he/she will be subject to dismissal from the CHHS Program in accordance with the CHHS Academic Dismissal Policy. b. Undergo a criminal background check by a CHHS-approved agency. Some Agencies require that students obtain criminal background checks on their own. In these cases, students should apply to a CHHS-approved criminal investigation agency for a criminal background check to be conducted at the student’s expense. The criminal investigation agency will provide the background check results to the student. Students are responsible for keeping the original criminal background check and sharing the results with each Agency that they are assigned to. If a student is rejected from an Agency, CHHS will attempt to assign the student to another Agency. If no Agency accepts a student, he/she will be subject to dismissal from the CHHS Program in accordance with the CHHS Academic Dismissal Policy. 3. Agency Drug Screening Requirements a. Comply with the drug screening requirements at each agency to which students are assigned. In some cases, the Agency will facilitate drug screening. Students will usually bear all expense associated with meeting these requirements. CHHS will receive notice only that a student has been accepted or rejected by the Agency. If a student is rejected from a Agency, CHHS will attempt to assign the student to another Agency. If no 41 Agency accepts a student, he/she will be subject to dismissal from the CHHS Program in accordance with the CHHS Academic Dismissal Policy. b. Undergo drug testing by a CHHS-approved drug screening laboratory. Some Agencies require that students obtain a drug screening on their own. In these cases, students should apply to a CHHS-approved independent drug screening laboratory for a drug test to be conducted at the student’s expense. Students will be given the original results, which they are responsible for sharing with the Agency. If the result is positive, and the Agency rejects the student, CHHS will attempt to place the student at another Agency. If no Agency accepts a student, he/she will be subject to dismissal from the CHHS Program in accordance with the CHHS Academic Dismissal Policy. Attachment 1 – Practicum Course Syllabus University of North Carolina at Charlotte College of Health and Human Services Department of Kinesiology Course Number and Title: KNES 6490 – Advanced Practicum in Clinical Exercise Physiology (1 credit) Faculty Information: Dr. Trudy Moore-Harrison, Rm. 240M Belk Gym tlmoore2@uncc.edu, 704-687-0862 Catalog Description: KNES 6490. Advanced Practicum in Clinical Exercise Physiology. (1) Acquisition and application of knowledge, skills, and abilities necessary for the Registered Clinical Exercise Physiologist while gaining experiential hours in an appropriate clinical setting. Three (3) credit hours of Advanced Practicum is required for graduation; this course may be repeated for up to 6 credit hours. (Fall, Spring, Summer) Rationale: Clinical Exercise Physiologists (CEP) normally practice in a clinical environment. Thus, a necessary part of a CEP’s education is exposure to and time in a clinical environment. Additionally, registration as a Clinical Exercise Physiologist requires the completion of a certain number of clinical hours. This Practicum is a method by which to expose students to the clinical environment as well as helping them fulfill the clinical hour requirements of the Registry. Course Objectives: At the completion of the course the student will have gained experience in providing clinical exercise services for patients with chronic diseases and conditions as specified in the Clinical Exercise Physiologist Scope of Practice. Students will gain experiential hours that count towards satisfying the American College of Sports Medicine’s requirement for 600 hours of clinical experience in the following areas. • Cardiovascular: 120 hours required 42 • Pulmonary: 30 hours required • Metabolic: 60 hours required • Orthopedic/Musculoskeletal: 60 hours required • Neuromuscular: 30 hours required • Immunological/Hematological: 30 hours required • Additional hours from any of the above: 270 hours required Clinical Site Assignment: Students will be matched with a clinical site dependent upon their skill level, their interests, and their level within the program. The perceived convenience of a clinical site will not be a factor in matching a student with a clinical site. Students may request a particular site, but are not guaranteed to be assigned to the requested site. The Practicum Coordinator will attempt to complete the initial clinical site assignment 3-4 weeks before the beginning of the semester. Upon notification of the site assignment, the student should immediately call and make an interview appointment with the Clinical Site Preceptor. After the interview, the Preceptor will then notify the Practicum Coordinator as to the acceptability of the student. If you are accepted at your site, you should immediately complete a scheduling agreement with the site, which will then be forwarded to the Practicum Coordinator. Items needed for Practicum: Given that in all of the clinical sites, the student will working with populations with chronic conditions, it is imperative that several standard clinical precautions be in place before the student is allowed to begin the clinical experience. Copies of each of these items should be provided to the Practicum Coordinator and to the Clinical Site Preceptor. Questions about any of these items can be directed to the Practicum Coordinator. Items needed: 1. Copy of Immunization Records including Recent Tuberculosis Skin Test 2. Current and Valid CPR certification 3. Copy of Professional Liability Insurance 4. Bloodborne Pathogens Tutorial and Test 5. Criminal Background Check 6. Drug Screening Additional copies of immunization records, current CPR certification, and a copy of professional liability insurance should be provided to the Clinical Site Preceptor. Furthermore, some clinical sites require an additional criminal background check, immunizations, and/or drug screening. Your Clinical Preceptor will inform you if either is required. Both items should be handled between the student and the Clinical Site (i.e. the University is not involved in these requirements). COURSE POLICIES ITEMS INVOLED IN DETERMINING YOUR GRADE Attendance In conjunction with the Clinical Site, students are required to develop and submit a work schedule indicating the number of hours per week they will be gaining experiential hours in a particular setting (see Appendix E). Three unexcused absences during a clinical rotation will result in the lowering of the final practicum course grade by one letter. Five unexcused absences will result in failure of the practicum course. It is the student’s responsibility to keep up with their scheduled clinical responsibilities and events. If a student cannot make a scheduled clinical responsibility or event, it is his or her responsibility to communicate directly with their 43 supervising Clinical Preceptor in a timely fashion. Students are to be prompt and on time for all clinical responsibilities and events. Showing up late for 3 clinical assignments will equal one unexcused absence. Grading Scale and Criteria The student’s final grade will be based on the cumulative point totals from each of the following evaluation techniques: Evaluation Type Number Points Each Total Schedule Agreement 1 set 10 10 Clinical experience journal 8 entries 10 80 Midterm and Final Preceptor Evaluation 2 sets 100 200 Log Book of Clinical Hours 1 set 10 10 Total 300 The student’s final grade will be awarded based on the following scale: A 90-100% B 80-89% C 70-79% D 60-69% F <60% Clinical Education Journal Students are required to keep track of their daily clinical experiences in a journal format (Appendix G). Students are required to submit their journal entries via e-mail every 2 weeks. Midterm and Final Preceptor Evaluations A large component of this course is the clinical evaluation of the student’s knowledge, skills, and abilities (KSA) while working in the clinical setting (see Appendix B). The student’s clinical preceptor will complete a formal evaluation of their skills, professional attributes and likelihood for success at the midpoint and end of the clinical experience. Syllabus Subject to Change: The instructor reserves the right to alter this syllabus based on best practices that fit changing circumstances. UNIVERSITY POLICIES Code of Student Responsibility: “The UNC Charlotte Code of Student Responsibility (the Code) sets forth certain rights and responsibilities in matters of student discipline. The Code defines these responsibilities and guarantees you certain rights that ensure your protection from unjust imposition of disciplinary penalties. You should familiarize yourself with the provisions and procedures of the Code” (Introductory statement from the UNC Charlotte brochure about the Code of Student Responsibility). The entire document may be found at this Internet address: http://legal.uncc.edu/policies/ps-104.html Academic Integrity: 44 Students have the responsibility to know and observe the requirements of The UNC Charlotte Code of Student Academic Integrity. This code forbids cheating, fabrications, or falsification of information, multiple submission of academic work, plagiarism, abuse of academic materials, and complicity in academic dishonesty. Academic evaluations in this course include a judgment that the student’s work is free from academic dishonesty of any type; and grades in this course therefore should be and will adversely affected by academic dishonesty. Students who violate the code can be expelled from UNC Charlotte. The normal penalty for a first offense is zero credit on the work involving dishonesty and further substantial reduction in the course grade. In almost all cases the course grade is reduced to F. Copies of the code can be obtained from the Dean of Students Office or http://legal.uncc.edu/policies/ps-105.html. Students are expected to report cases of academic dishonesty to the course’s instructor. Special Needs: If you have a documented disability and require accommodation in this course, contact Disability Services, Fretwell 230, phone: 687 4355 voice/TDD) the first week of the semester. Information about available services may be found at http://legal.uncc.edu/policies/ps-51.html. Accommodations for learning will be arranged by that office and communicated to the Instructor. If you speak English as a second language, please inform the instructor. Diversity Statement: UNC Charlotte strives to create an academic climate in which the dignity of all individuals is respected and maintained. Therefore, we celebrate diversity that includes, but is not limited to ability/disability, age, culture, ethnicity, gender, language, race, religion, sexual orientation, and socio-economic status. All students are required to abide by the UNC Charlotte Sexual Harassment Policy (http://www.legal.uncc.edu/policies/ps-61.html) and the policy on Responsible Use of University Computing and Electronic Communication Resources (http://www.legal.uncc.edu/policies/ps-66.html). Sexual harassment, as defined in the UNC Charlotte Sexual Harassment Policy, is prohibited, even when carried out through computers or other electronic communications systems, including course-based chat rooms or message boards. Religious Accommodation: It is the obligation of students to provide faculty with reasonable notice of the dates of religious observances on which they will be absent by submitting a Request for Religious Accommodation Form to their instructor prior to the census date for enrollment for a given semester http://legal.uncc.edu/policies/ps-134.html . The census date for each semester (typically the tenth day of instruction) can be found in UNC Charlotte’s Academic Calendar (http://registrar.uncc.edu/calendars/calendar.htm). 45 – Attachment 2 Student Clinical Experience Schedule agreement By this agreement, (Preceptor Name) and (Student Name) state that the clinical experience for (Student Name) will begin on (date) and will conclude (date). Within this timeframe, (student name) will be present at the Clinical Site on (days of week) at the following times: (hours of presence). This schedule will result in a total of (number of hours) hours per week of the clinical experience*. This schedule can be amended by agreement of the Preceptor and Student at any time during the semester. Agreed to on (date) by: ________________________________________ Signature of Preceptor _______________________________________ Signature of Student Reviewed by Practicum Coordinator:____________________________ ______________ Signature of Practicum Coordinator Date *Students should not generally commit to more than 20 hours of clinical experience per week. Exceptions to this policy can be requested via a written request from the student to the Practicum Coordinator. Generally, failure of the student to complete sufficient hours earlier in the semester will not be considered a valid reason for suspension of the 20 hr/week policy. 46 – Attachment 3 Example format for Student Hour Logbook Student Name: Date Time Start Time End Total Time Clinical Site General Activities/Practice Area 47 Running Hour Total – Signature and Title of Verifying Professional: Attachment 4 Example format for Student Clinical Journal Student Name: Date(s): Clinical Site: Total Clinical Hours: Journal of Clinical Activity: Include in this journal, a discussion of any activities that you participated in during each day of your clinical experience. Explain the activity, what you did, how your performance was with respect to expectations, and how many clinical hours you worked that day. You can also discuss other observations or personal feelings that were experienced during the day. On Fridays, after discussing the activities for that day, write a paragraph summarizing the week’s activities and how you feel about your performance as a professional. 48 Attachment 5 – Preceptor evaluation of Student Student Evaluation by Clinical Preceptor MS in Kinesiology Department of Kinesiology Student’s Name: Date: Clinical Site: Clinical Site Preceptor: Practicum Coordinator: Please check the appropriate box that best represents your evaluation of the student. Excellent (5) Good (4) Average (3) Below Average (2) Working relationship with On-site Preceptor Working relationship with staff Working relationship with employees Dependability Attitude towards tasks Initiative Trustworthy? Judgment Professional appearance? Acceptance of criticism Sets realistic goals Identifies new opportunities to contribute Follows instructions from coordinator Ability to learn Quality of work Discuss the student’s performance during the clinical experience. 49 Poor (1) Not Applicable – What are the student’s greatest weaknesses? What are the student’s greatest strengths? Describe the student’s performance since the midterm evaluation (NA on midterm evaluation): Other comments: Your overall evaluation of the student as a potential employee (5 = high and 1 = low)? 5 4 3 2 1 Clinical Site Preceptor Date Student Date 50 Attachment 6 ACSM RCEP Code of Ethics A. Principles and purposes: Preamble—These principles are intended to aid Fellows and members of the College individually and collectively to maintain high level of ethical conduct. These are not laws but standards by which a Fellow or a member may determine the propriety of his/her conduct, relationship with colleagues, with members of allied professions, with the public, and with all persons in which a professional relationship has been established. The principal purpose of the College is the generation and dissemination of knowledge concerning all aspects of persons engaged in exercise with full respect for the dignity of people. Section 1: members should strive continuously to improve knowledge and skill and make available to their colleagues and the public the benefits of their professional expertise. Section 2: members should maintain high professional and scientific standards and should not voluntarily collaborate professionally with anyone who violates this principle. Section 3: The College, and its members, should safeguard the public and itself against members who are deficient in ethical conduct. Section 4: The ideals of the College imply that the responsibilities of each Fellow or member extend not only to the individual, but also to society with the purpose of improving both the health and wellbeing of the individual and the community. B. Maintenance of Good-standing in Regulated Professions: Any Fellow or member required by law to be licensed, certified or otherwise regulated by any governmental agency in order to practice his or her profession must remain in good-standing before that agency as a condition of continued membership in the College. Any expulsion, suspension, probation or other sanction imposed by such governmental agency on any Fellow or member is grounds for disciplinary action by the College. C. Public Disclosure of Affiliation: Other than for commercial venture, any member or Fellow (FACSM) may disclose his/her affiliation with the College in any context, oral or documented, provided it is currently accurate. In doing so, no member or Fellow may imply College endorsement of whatever is associated in context with the disclosure, unless expressly authorized by the College. Disclosure of affiliation in connection with a commercial venture may be made provided the disclosure is made in a professionally dignified manner, is not false, misleading or deceptive, and does not imply licensure for the attainment of specialty or diploma status. Members who are currently ACSM Certified or Registered may disclose their certification status and Fellows may disclose their Fellow status. Because membership and fellowship in ACSM is granted to individuals, disclosure of affiliation and/or use of the initials ACSM are not to be made as part of a firm, partnership or corporate name. Violation of this article may be grounds for disciplinary action. D. Discipline: Any Fellow or member of the College may be disciplined or expelled for conduct which, in the opinion of the Board of Trustees, is derogatory to the dignity of or inconsistent with the purposes of the College. The expulsion of a Fellow or member may be ordered upon the affirmative vote of two-thirds of the members of the Board of Trustees present at a regular or a special meeting, and only after such Fellow or member has been informed of the charges preferred against him and has been given an opportunity to refute such charges before the Board of Trustees. Other disciplinary action such as reprimand, probation, or censure may be recommended by the Committee on Ethics and Professional Conduct and ordered following the affirmative vote of two-thirds of the members of the Board of Trustees present at a regular or special meeting or by mail ballot, provided a quorum takes action. (American College of Sports Medicine – 10/9/04) 51 – Attachment 7 RCEP Scope of Practice The Clinical Exercise Physiologist is an allied health professional who uses exercise and physical activity to assess and treat patients at risk of or with chronic diseases or conditions where exercise has been shown to provide therapeutic and/or functional benefit. Patients for whom RCEP services are appropriate may include, but are not limited to, persons with cardiovascular, pulmonary, metabolic, cancerous, immunologic, inflammatory, orthopedic, musculoskeletal, neuromuscular, gynecological, and obstetrical diseases and conditions. The RCEP provides scientific, evidence-based primary and secondary preventive and rehabilitative exercise and physical activity services to populations ranging from children to older adults. The RCEP performs exercise screening, exercise testing, exercise prescription, exercise and physical activity counseling, exercise supervision, exercise and health education/promotion, and evaluation of exercise and physical activity outcome measures. The RCEP works individually and as part of an interdisciplinary team in clinical, community, and public health settings. The practice and supervision of the RCEP is guided by published professional guidelines, standards, and applicable state and federal regulations. The practice of clinical exercise physiology is restricted to patients who are referred by and are under the care of a licensed physician. (American College of Sports Medicine – 10/9/04) Attachment 8 Drug Screening and Criminal Background Check Form DRUG SCREENING AND CRIMINAL BACKGROUND CHECK ACKNOWLEDGEMENT AND AGREEMENT UNC CHARLOTTE COLLEGE OF HEALTH AND HUMAN SERVICES EDUCATION PROGRAMS REQUIRING EXTERNAL HEALTH OR HUMAN SERVICE AGENCIES Student’s Printed Name 1. CHHS Program I understand and acknowledge that the UNC Charlotte College of Health and Human Services (CHHS) has affiliated with several health care and human services facilities (hereinafter “ Agencies”) to provide internships, field placements or clinical experiences for students in the CHHS (hereinafter “Students”). I further understand and acknowledge that the Agencies have a compelling interest in the integrity of their services and the health and safety of their patients, others who may come into contact with Students, and the Students themselves. 52 2. I understand and acknowledge that in order to protect their interests, many Agencies require Students to comply with their drug testing and/or criminal background check policies and to undergo drug testing and/or criminal background checks as conditions of participating in their education programs. In addition, such Agencies often require that Students submit to the required drug testing and/or criminal background checks at the Students’ own expense. I understand that the CHHS will provide Students with information to obtain the drug testing and/or criminal background checks required by the Agencies. 3. I understand and acknowledge that a Agency may, in accordance with its policies, reject or expel a Student from its Agency based on the results of the drug testing and/or criminal background checks. 4. I am or will be enrolled as a student in the CHHS, and I plan to participate as a Student in a educational experience at an Agency . 5. Because participation in agency-related educational programs is a degree requirement for students in the CHHS program indicated above, I understand that I may be required to undergo a criminal background check and/or drug screening as a condition of my participation in an internship, field placement or clinical experience at an external health and human service agency. 6. As a condition of participating as a Student in an education program, I hereby agree to comply with the criminal background check requirements at each Agency to which I am assigned. If the Agency facilitates criminal background checks, I agree to comply with such requirements and follow the procedures set forth by the Agency . If the Agency requires that I undergo a criminal background check prior to my placement, I agree to undergo a criminal background check by a CHHS-approved agency at my own expense. I will then submit my original results to the Agency, which shall determine whether the results of my criminal background check are acceptable. 7. I hereby agree to comply with the drug screening test requirements at each Agency to which I am assigned. If the Agency facilitates drug screening, I agree to comply with such requirements and follow the procedures set forth by the Agency . If the requires that I undergo drug screening prior to my placement, I agree to undergo drug testing by a CHHS approved testing laboratory at my own expense. I will then submit my original results to the, which shall determine whether the results of my drug screening are acceptable. 8. I have read both the CHHS Criminal Background Check and Drug Screening Policy and this Acknowledgement and Agreement, and I understand its contents. I have had the opportunity to ask questions of and discuss the Policy and this Acknowledgement and Agreement with appropriate administrators in the College of Health and Human Services. I understand that I am responsible for meeting the requirements set forth in the Policy and this Acknowledgment and Agreement. Student’s Signature Date Attachment 9 CHHS Clinical Agency Requirements Form College of Health and Human Services Clinical Agency Requirements As part of the affiliation agreements between the different agencies and the College of Health and Human Services, you are required to provide specific compliance records to the college (in addition to those you provide to the university) before you can start your clinical/practicum/internship. Please complete this form by recording the immunization and other dates and attaching proof where required. When complete, turn a copy to Sandra Mann in the CHHS Advising Center, located in Health and Human Services Building, Room 103, or if you would like to fax this form and any attachments, the fax number is 704-687-1655. If you have any questions, please contact Sandra Mann at 704-687-7922. 53 – Name: Immunization Student ID: Mo/day/year Mo/day/year Mo/day/year 3 DPT (diphtheria, tetanus, pertussis) #1 #3 #2 DOB: Mo/day/year Tetanus Booster within 10 yrs. MMR #1 #2 or Titer date & results (attach Measles, Mumps, Rubella proof) Hepatitis B Series #1 #2 #3 or Form to decline of 3 Varicella #1 #2 or Titer date & results (chicken pox)series of two doses or (attach proof) titer *Tuberculin Skin Test (PPD) Annual requirement. If PPD is positive, a one-time chest x-ray is required. Chest x-ray documentation to include date, results and recommendation(s) for future testing. Some agencies require a two-step testing process that requires a second PPD to be administered and read within 1-3 weeks of the initial test. You will be notified if you need a two-step test by your program coordinator. Date Results (attach proof and submit documentation annually) Additional Compliance Requirements- (All of these may not be required by your agency, or additional requirements may be needed. Check with your program coordinator.) Date completed: Criminal Background Check Date received: Drug Screening Date completed: Bloodborne Pathogens Training (Annual) Coverage dates: Liability Insurance Certification dates: CPR Always make a copy for your records before turning in to the CHHS Advising Center If you plan to use the Student Health Center to receive any of your immunizations, please call 704-687-7400 to schedule an appointment. Doing this will save you time and trips to the SHC. 54 Appendix C: Graduate Assistantship Handbook Appendix C: Graduate Assistantship Handbook .................................................................................................. 50 Clauses in all GA Contracts .......................................................................................................................... 51 Graduate Assistant Dress Code Policy ......................................................................................................... 52 KNES Teaching Assistant Dress Code Policy .............................................................................................. 52 Attitude: ........................................................................................................................................................ 55 Teaching Assistant Handbook: ..................................................................................................................... 55 Punctuality: ................................................................................................................................................... 56 External jobs/work: ....................................................................................................................................... 56 Academic Expectations ................................................................................................................................. 56 Notice of Assistantship Status ...................................................................................................................... 57 Created 9/14 (EAW) Clauses in all GA Contracts • Because of the nature of this appointment Graduate Assistants are not eligible for benefits offered by the State to employees and Student's employment is not subject to the North Carolina State Personnel Act. • All Graduate Assistants are limited to employment not to exceed a total of twenty hours per week for all jobs, on or off campus, with the exception of summer hours which must be pre-approved by the Graduate School. Failure to abide by this restriction may result in the termination of this appointment. • If for any reason Student is unable to, or otherwise does not, complete the term of appointment, compensation will be prorated on the basis of duties actually performed and the time worked. • Student must enroll for a minimum of six graduate credit hours (or nine if receiving GASP) during each academic semester that this appointment is in effect and continuation of this appointment is contingent upon satisfactory performance in all courses and maintenance of a 3.0 Graduate GPA. Continuing students are eligible to hold summer appointments provided that the student is registered for the fall semester or concurrent summer session. • Student also agrees to perform the duties and responsibilities set forth in Attachment A to this Agreement, which is attached hereto and incorporated herein as if fully set forth. • Student agrees to carry out all duties and responsibilities in compliance with all federal and state laws and regulations and with the provisions of the University's Policy Statements. Said policy statements include, but are not limited to, Policy Statement # 105 Code of Student Academic Integrity and Policy Statement # 104 Code of Student Responsibility. A violation of any law, regulation, or policy statement may result in termination of this Agreement. The University's policy statements are available here. • Any academic dishonesty by students in any class for which Student is responsible must be handled in accordance with the provisions of the Code of Student Academic Integrity. • Student is required to participate in the Graduate School's Graduate Teaching Assistant Orientation program. International Teaching Assistants are also required to attend the ITA Orientation and Language 56 Assessment program. Failure to attend the Graduate Teaching Assistant Orientation program may lead to termination of this Agreement. The complete set of University policies regarding Graduate Assistantship appointments can be found at the Office of the Provost. Graduate Assistant Dress Code Policy For the purposes of this policy, a Graduate Assistant is defined as any student enrolled in the MS in Kinesiology program that holds the following positions: 1. A Graduate Assistantship (GA) position through an agency outside of UNC Charlotte. 2. A Graduate Assistantship (GA) through a unit (academic or otherwise) within UNC Charlotte but outside of the Department of Kinesiology. 3. A Research Assistantship (RA) through a Research Laboratory either within or external to UNC Charlotte (e.g. RA position within the Laboratory of Systems Physiology). 4. A Teaching Assistantship (TA) through an academic program outside of the Department of Kinesiology (e.g. LBST TA position). It is our policy that such students dress as required by their employer. The requirements of the employer should be sought out prior to the initiation or employment and should be maintained at all times. When in doubt, the dress for any and all students on a GA, RA, or TA should be professional, promote UNC Charlotte and/or the respective agency, lab, or program they are employed by and be appropriate for work being conducted. KNES Teaching Assistant Dress Code Policy Policy Motto: No shirts, no shoes, no money! For the purposes of this policy, a Teaching Assistant (TA) is defined as any individual who assists with the delivery of an academic course (i.e. interacting with enrolled students) under any of the following conditions: 1) 57 as a volunteer, 2) as a student enrolled in an independent study style course, or 3) as a paid employee of the department of Kinesiology. Given the breadth of academic courses offered by the department of Kinesiology, several dress codes have been developed and will be explained in greater detail below. In general, the dress for any and all TAs should be professional, promote UNC Charlotte whenever possible, and be appropriate for the instructional setting. Dress Code for TAs of activity based courses. 1. If participating in the activities of the day, then clean and appropriate workout clothes should be worn. Preference should be given to UNC Charlotte attire with secondary preference given to neutral attire. 2. Hair is to be kept neat and clean and of appropriate length. Men should keep facial hair neatly trimmed and clean. 3. If not participating in the activities of the day, then clean and appropriate casual to professional dress clothes should be worn. This includes polo and t-shirts for tops and nice jeans (no holes and must be worn above your hips), slacks, dresses, skirts, or khaki style shorts for bottoms. Preference should be given the UNC Charlotte attire with secondary preference given to neutral attire. 4. Clean and appropriate jackets, sweatshirts, sweaters, etc. are allowed during colder weather but should adhere to the same guidelines listed above for shirts when both participating and not participating in activities. 5. The following items are not allowed: sandals/flip-flops, hats (when indoors), tops without sleeves when worn as outerwear (e.g. sleeveless shirts, tank tops, sports bras), any article of clothing with tears and/or holes, any articles of clothing that may be considered revealing at any time during the required duties of a TA (e.g. low cut tops, overly short shorts, etc), and articles of clothing promoting non-UNC Charlotte academic institutions. 58 6. If questions arise regarding the appropriateness of attire, please seek the guidance of the Mrs. Linda Probst, the Lifetime Activity Course Supervisor. Final discretion of attire appropriateness lies with the Lifetime Activity Course Supervisor. Dress Code for TAs of didactic and/or psychomotor based labs and courses. 1. Clean and appropriate casual to casual dress clothes should be worn at all times. This includes polo (preferred) or t-shirts for tops and nice jeans (no holes and must be worn above your hips), slacks, dresses, skirts, or khaki style shorts for bottoms. Preference should be given to UNC Charlotte attire with secondary preference given to neutral attire. Casual to professional footwear should also be worn at all times. 2. Hair is to be kept neat and clean and of appropriate length. Men should keep facial hair neatly trimmed and clean. 3. The following items are not allowed: sandals/flip-flops, hats (when indoors), tops without sleeves when worn as outerwear (e.g. sleeveless shirts, tank tops, sports bras), any article of clothing with tears and/or holes, any articles of clothing that may be considered revealing at any time during the required duties of a TA (e.g. low cut tops, overly short shorts, etc), and articles of clothing promoting non-UNC Charlotte academic institutions. 4. Clean and appropriate jackets, sweatshirts, sweaters, etc. are allowed during colder weather but should adhere to the same guidelines listed above for shirts. 5. If questions arise regarding the appropriateness of attire, please seek the guidance of the faculty member that you are assisting. Final discretion of attire appropriateness lies with the faculty member you are assisting. Dress Code for TAs that serve as the lead/sole instructor of a didactic and/or psychomotor based labs and courses. 59 1. Clean and appropriate casual dress clothes must be worn at all times. This includes button down or polo shirts for tops and nice jeans (no holes and must be worn above your hips), slacks, dresses, or skirts for bottoms. Preference should be given to UNC Charlotte attire with secondary preference given to neutral attire. Casual to professional footwear should also be worn at all times. 2. Hair is to be kept neat and clean and of appropriate length. Men should keep facial hair neatly trimmed and clean. 3. The following items are not allowed: sandals/flip-flops,, hats (when indoors), t-shirts, shorts, any article of clothing with tears and/or holes, any articles of clothing that may be considered revealing at any time during the required duties of a TA (e.g. low cut tops, overly short shorts, etc), and articles of clothing promoting non-UNC Charlotte academic institutions. 4. Clean and appropriate jackets, sweatshirts, sweaters, etc. are allowed during colder weather but should adhere to the same guidelines listed above for shirts. 5. If questions arise regarding the appropriateness of attire, please seek the guidance of the faculty member that you are assisting. Final discretion of attire appropriateness lies with the faculty member that serves as your supervisor. This specific policy was approved by the Kinesiology faculty on 9/14 (Created by JM & EW) Attitude: This program requires a substantial commitment on the part of the faculty, staff and students. If you have an attitude of being willing to learn and enjoying the fields of Kinesiology you will be successful here. Be active and take advantage of the many opportunities offered. View your responsibilities as an opportunity to learn and advance your own personal skill sets rather than just more work. Practice developing a positive attitude; this will rub off on others and help in dealing with clients/research subjects, students, and your peers. Develop a professional, yet friendly and positive manner when working and dealing with others. This program is your chance to work on this important aspect of being professional. 60 Teaching Assistant Handbook: For helpful hints at how to begin your teaching duties, please see the Teaching Assistant Handbook Punctuality: Be on time for all meetings and events (Being on time means arriving 10-15 minutes early for any appointment). When you have a job, show up early and make sure everything is ready prior to actual performance. External jobs/work: An assistantship involves 20 hours/week of scheduled work plus active participation in other weekly activities. Another 20+ hours/week will be spent attending classes, studying/writing for classes, learning new techniques, and assisting with other activities. This is easily a 40+ hour work week; any additional outside work can have a negative effect on your academic success and/or success in your assistantship duties. While we will not stop students from obtaining outside employment, it is very important for students to understand the important of not spreading themselves too thin. Academic Expectations To qualify for full assistantship money and be considered a full time student, you must be enrolled in nine graduate credit hours each Fall and Spring semester. During summer sessions a stipend can be given when no classes are being taken. However, you are often required to be registered for 9 graduate credit hours for the following Fall semester to earn your paycheck. It will be your responsibility to balance your assistantship commitments and your coursework, research thesis, and/or preparation for your comprehensive examination. You will not be excused from your assistantship duties because of an upcoming classroom assignment or issues relating to your thesis or comprehensive 61 examination (RCEP exam). Each semester it is expected that you communicate with the Program Coordinator about your upcoming class schedule and progress towards graduation. Notice of Assistantship Status Any and all assistantships can be revoked at any time if procedures in this manual or faculty recommendations/requests are not adhered to. Assistantship contracts and letters will be signed at the beginning of each academic year and at the beginning of the summer. An assistantship will generally be provided for two full academic years (year 1 - Fall, Spring; year 2 - Fall, Spring) but depends on the exact contract. 62 Appendix D: Certification Opportunities ACSM Certified Clinical Exercise Specialist (CES) The ACSM Certified Clinical Exercise Specialist® is proficient in: working with individuals with controlled cardiovascular pulmonary and/ or metabolic disease, performing clinical exercise testing and data interpretation, Conducting and interpreting ECGs at rest and during exercise. ACSM/ACS Certified Cancer Exercise Trainer (CET) A CET is a fitness professional who trains men and women who were recently diagnosed with cancer and have not yet begun treatment, are receiving treatment, have completed treatment or are a survivor experiencing chronic or late effects from disease or treatment; and are apparently healthy or have the presence of known stable cardiovascular disease with low risk for complications with vigorous exercise and do not have any relative or absolute contraindications for exercise testing. ACSM Health Fitness Specialist (HFS) The ACSM Certified Health Fitness Specialist (HFS) is a degreed health and fitness professional qualified to pursue a career in university, corporate, commercial, hospital, and community settings. ACSM Certified Personal Trainer (CPT) The ACSM Certified Personal Trainer is a fitness professional involved in developing and implementing an individualized approach to exercise leadership in healthy populations and/or those individuals with medical clearance to exercise. 63 NSCA Certified Strength & Conditioning Specialist ® (CSCS ®) This certification identifies individuals who possess the knowledge and skills to design and implement safe and effective strength and conditioning programs. NSCA-Certified Personal Trainer ® (NSCA-CPT ®) The NSCA-CPT ® credential is designed for professionals who work one-on-one with their clients in a variety of environments, including YMCA’s, schools, health/fitness clubs and clients’ homes. NSCA- Certified Special Population Specialist (CSPS) The NSCA-CPT ® credential is designed for professionals who, using an individualized approach, assess, motivate, educate, and train special population clients of all ages regarding their health and fitness needs, preventively, and in collaboration with healthcare professionals. 64