The Clinical Experience of
advertisement

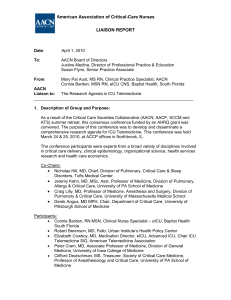
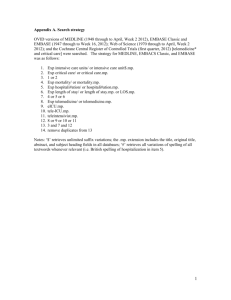
Research Student Expressions of Interest: Assessment of the Outcomes of Intensive Care Telemedicine Clinical Rounds in Bundaberg Base Hospital A/Professor Robert J Boots, Professor Jeffrey Lipman, Dr Neil Widdicombe, Dr Morne Terblanche, Dr Sunil Singh, Toni Hoffman, Geraldine Kucharski We are looking for a health science higher degree student interested in new health care delivery paradigms and their impact on patient centred and health organization outcomes. The clinical scenario involves a recently introduced, novel telemedicine service to assist in patient care at Bundaberg Base Hospital. The project intends to cover a broad spectrum of health care impacts including clinical communication, organization impacts, financial implications and direct patient outcomes. The project has enough broad focus to meet requirements for a higher degree thesis (e.g. PhD) and would be suitable for students interested in a career in health outcomes and organizational research. Research would be based within Brisbane with the possibility of several short field trips to Bundaberg. The anticipated time frame for completion would be 2 years allowing a period of 12 months of consolidated Thesis preparation. A preliminary protocol has been formulated which the student is expected to develop further and progress. An experienced team of researchers and clinicians under our Research Centre (Burns, Trauma and Critical Care Research of the University of Queensland) will support and supervise the research student. The person Candidates will have a 1st Class Honours or equivalent and should be eligible for an Australian Postgraduate Award (APA) or equivalent. Prospective students will be provided with assistance to secure either an APA or, for international students, an International Postgraduate Research Scholarship (IPRS). Remuneration The stipend will be at the APA rate of $23,728 p.a tax-free for three years (top ups available based on merit). Enquiries A/Prof Robert Boots r.boots@uq.edu.au or 3636 8897 The Research Telemedicine by the use of audiovisual technologies is increasingly being used to assist in patient care by intensive care units unable to be staffed by specialist consultant intensivists. Models of care range from complete remote 24hour surveillance requiring direct video observation to a consultation liaison service only requiring conventional telephone links. There has been a rapid adoption of such services especially in North America where access to on-site intensive care specialists is limited for the volume of intensive care being undertaken. A key task is to ascertain the most appropriate service requirements that would assist in care for a given patient circumstance. A telemedicine intensive care consultation service has been introduced into Bundaberg Base Hospital. Bundaberg Base is a regional 200-bed hospital in Queensland, Australia. The model of care is an “open ICU” with primary teams having admission rights for patients not requiring mechanical ventilation. Ventilated patients were admitted under the care of the anaesthesia staff with the primary medical teams continuing their consultation. There were no credentialed intensive care medical specialists. Patients requiring more that two days of mechanical ventilation had been traditionally referred to the nearest tertiary ICU. In 2009 a new model of care was established with equipment and staff funding support from Queensland Health. An intensive care specialist undertook regular daily formal WARD ROUNDS for one hour between Monday-Friday via a videoconference link from the Royal Brisbane and Women’s Hospital Intensive Care Unit. This specialist was available for the remainder of the day to deal with additional queries via telephone or video link consultation. Ward rounds used a mobile wireless web-camera as part of a computer videoconferencing system. Additional duties of the Intensivist including coordinating the patient transfer to a tertiary unit or organising additional specialist review where appropriate. Study Questions 1. What has been the impact of a Telemedicine ICU Ward Round in a regional hospital on patient outcomes? 2. What has been the impact on the regional intensive care unit operations since the introduction of a Telemedicine ICU Ward Round? 3. What is the nature and type of the communications between health care staff during Telemedicine ICU Ward Rounds to a regional ICU? 4. What are the staff attitudes to Telemedicine ICU Ward Rounds in both the resource and the regional intensive care unit?