Seasonal Variation in Preeclampsia and Eclampsia, an Analysis of
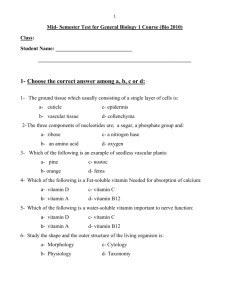
advertisement

1 Title Page 2 3 Revisiting the Link Between Preeclampsia, Eclampsia and Seasonal Variation: An 4 Analysis of over 39,000 Deliveries in West Michigan from 2005 to 2010 5 None of the authors of the paper have any personal financial interest in the work or with 6 a commercial sponsor. 7 8 9 INTRODUCTION 10 Preeclampsia (PreE) and eclampsia (E) is a syndrome affecting multiple organ systems with 11 symptoms including severe headache, vision changes, right upper-quadrant pain, nausea and 12 vomiting, dizziness, and edema. In the United States, preeclampsia and eclampsia complicate 13 2–7% of first-time pregnancies and are characterized by new-onset hypertension with 14 concurrent proteinuria after 20 weeks gestation [1]. In Canada, women who immigrated from 15 Hispanic, Sub-Saharan African or Caribbean countries were three times more likely than women 16 from industrialized nations to develop PreE/E [2]. This disorder causes significant fetal and 17 maternal morbidity and its basic pathophysiology is not well understood [3-5]. As a result, 18 preeclampsia and eclampsia present significant challenges to clinicians who seek to provide the 19 best outcomes for both their patients and their infants. 20 21 Studies have emerged that analyze the role vitamin D deficiency plays in the development and 22 progression of PreE/E [6]. Low serum vitamin D levels in pregnant women have been found to 23 increase the risk of PreE/E and vitamin D deficiency may be an independent risk factor for 24 developing PreE/E [7,8]. Similarly, studies have shown that serum Vitamin D levels fluctuate 25 with exposure to sunshine. In a group of women of childbearing age, sunlight exposure during 26 May-October were significantly and independently associated with lower prevalence ratios of 27 vitamin D deficiency and inadequacy [9]. Vitamin D levels of healthy Canadians were highest in 28 the summer and lower in the fall and spring [10]. Additionally, vitamin D levels of people living 29 in West Michigan tend to follow the same trend during the winter. A random sample of patients 30 who had their blood drawn over 12 weeks from January to April had an average vitamin D level 31 of 17.43 ng/ml, Males had a level on average of 16.3 ng/ml and women had an average of 17.6 32 ng/ml. Both of these averages are well below the accepted total vitamin D reference values of 33 25-80 ng/ml. [11] 34 35 Weather Patterns in West Michigan 36 Out of 174 U.S. cities and towns listed by the National Climatic Data Center, Grand Rapids in 37 West Michigan is number 161 in percent of annual available sunshine received (46%) [12]. The 38 area’s weather is determined by its latitude and eastern proximity to Lake Michigan; this location 39 receives lake effect snow, rain, and heavy cloud coverage. Because there is less sunshine 40 received in this region, we wanted to evaluate whether there is a strong correlation between 41 available sunlight and pregnancy complications. 42 43 This report describes the outcomes of over 39,000 births in West Michigan in relation to the total 44 available minutes of sunshine in the preceding trimester prior to the births. A strong correlation 45 between PreE/E rates and total amount of sunshine was observed. We briefly describe the 46 methods and results of the findings in this report. 47 Pathophysiology 48 Vitamin D deficiency has been implicated in many disorders including hypertension, end-stage 49 renal disease (ESRD), diabetes, heart disease, inflammatory disorders, and increased cancer 50 risk [6, 13-16]. Because the vitamin D receptor (VDR) modulates transcription of hundreds of 51 genes and is expressed in many cells in the human body [6,17], it affects multiple organ 52 systems. Low serum vitamin D levels is associated with many disease processes, including 53 those affecting the cardiovascular and renal systems. 54 55 Vitamin D deficiency is a well-established marker for cardiovascular disease [18-28] and 56 hypertension [25, 29-32]. Studies examining the link between vitamin D and cardiovascular 57 disease show an increase in cardiovascular mortality during seasons in which Ultra Violet B 58 radiation exposure is low [28, 33, 34], that there is an increase in thromboembolic events during 59 the winter months [36, 37]. Hypovitaminosis D is associated with elevated mortality from 60 cardiovascular illness [20-24, 26, 27]. Furthermore, multiple studies have linked vitamin D 61 deficiency to hypertension by vitamin D’s effect on renin [32, 38-41]. In 2007, Yuan et al. 62 showed vitamin D suppresses expression of a renin promoter gene indicating that low Vitamin D 63 levels could activate the renin angiotensin system [31]. Vitamin D’s renal effects extend beyond 64 the renin-angiotensin system. Extensive study of patients with ESRD has established low 65 Vitamin D is associated with the development of albuminuria and inflammation. . 66 Vitamin D Deficiency and the Development of Preeclampsia/Eclampsia 67 The combination of renal protein wasting and systemic inflammation is a hallmark of PreE/E and 68 has led to the hypothesis that vitamin D deficiency may be involved in the pathogenesis of 69 PreE/E [49]. Research shows that a correlation exists between hypovitaminosis D and PreE/E 70 as well as other complications of pregnancy [50-54] This relationship is supported by studies 71 that show that decidual and trophoblastic cells both make and respond to vitamin D and that 72 vitamin D aids in implantation. [55-67]. Furthermore, a Norwegian survey study indicated that 73 women who take vitamin D supplements have substantial reduction in PreE/E; however, 74 because vitamin D intake in this population is correlated with omega-3 intake it was not possible 75 to rule out a benefit from long chain fatty acids in the diet [68]. 76 77 MATERIALS AND METHODS 78 79 Using de-identified data, and adhering to IRB protocols the electronic medical record database 80 of Spectrum Health, a multi-hospital network in West Michigan predominantly serving Kent 81 County, was searched from June of 2005 through May of 2010 to construct the PreE/E rate. The 82 five most current years were used because after mid 2005, deliveries reached steady state as 83 labor and delivery was concentrated at one of the Spectrum Health hospitals. A rate was 84 calculated for each calendar month over those five years using diagnostic codes for PreE/E and 85 their ICD-9 (see table 1) derivatives from the hospital system’s medical record database. 86 Because the ICD-9 codes for both preeclampsia and eclampsia contain the 642 code number 87 series, it was not possible to reliably distinguish between the two diagnoses. The PreE/E codes 88 in each month during the five-year period were compared to total deliveries per month over the 89 same time frame to construct a PreE/E rate. 90 The PreE/E rate from this data was then compared to minutes of available sunlight in West 91 Michigan using public domain information from the National Weather Service. Specifically, the 92 total number of minutes of actual sunshine received at the Grand Rapids, Michigan weather 93 station for each month in the five-year period being examined as well as the three months prior 94 to the diagnosis of Pre/E was recorded and analyzed. This allowed for the comparison of 95 PreE/E rates in any month to the potential influence of vitamin D from accumulated sunlight 96 exposure in prior months. In order to work with positive integers, minutes of darkness were 97 derived from the sunlight data by subtracting the minutes of sunlight from the total minutes in 98 each month. The minutes of darkness for the month were then divided by the number of days in 99 each month to obtain the average minutes of darkness per day in each month. A similar 100 calculation was performed to find the average minutes of darkness per day in the three months 101 prior to the month of the PreE/E rate. 102 103 Vitamin D precursor molecules have half-lives of many weeks, which can lead to significant 104 accumulation over an extended period of sun exposure [69]. The correlation between available 105 sunlight and PreE/E rate was examined using the average minutes of darkness per day for the 106 one-month period and the three-month period prior to the month of the PreE/E rate. In order to 107 have a more powerful dataset the PreE/E rate of each month of each year was used 108 individually, giving 60 data points. 109 110 The Pearson product moment correlation coefficient was calculated as a measure of the linear 111 relationship between the of PreE/E rate for each month and the aforementioned corresponding 112 1 month and 3 month prior period’s average minutes of darkness. PreE/E rate was calculated 113 as the total of PreE/E cases in each month divided by the total live births in that month. A p 114 value <0.05 was considered to be significant. Correlations were calculated using SPSS, version 115 19, and checked for accuracy in Microsoft Excel. The 95% confidence intervals for rates were 116 calculated in Excel using the Normal Approximation Method. Graphical representations of the 117 data were created in Microsoft Excel 2003 (Bar Charts) and SPSS, version 19 (Scatter plot). A 118 confidence interval graph was created with Open Office, version 1.1. 119 120 RESULTS 121 122 There were 39,337 total live births during the five-year period under observation and 2,607 123 cases recorded as preeclampsia or eclampsia with delivery for a global rate of 6.63% (95% CIs 124 [.0638, .0688]). The rate varied from a high of 7.76% (95% CIs [.0681, .0871]) in December to a 125 low of 5.30% in September (95% CIs [.0455, .0605]); a 32% reduction from peak to trough. 126 Inversely this represents a 46% increase from September to December. The difference between 127 the peak and trough rates is statistically significant at the 95% level. The average rate from the 128 five low sun months of December through April was 7.32% (95% CIs [.0691, .0772]) and for the 129 high sun months of July through September was 5.64% (95% CIs [.0525, .0603]); these 130 numbers yield a relative increase of 30%, which is also statistically significant at the 95% level. 131 These confidence intervals can be seen in Figure 1. 132 133 Figure 1 134 135 136 The general pattern of the PreE/E rate from 2005 through 2010 and the average minutes of 137 darkness in the preceding three-month period can be seen in Figure 2. 138 Figure 2 139 140 141 There was a significant positive correlation (.r = 0.364, p = 0.004) between the PreE/E rate and 142 the prior three months’ average minutes of darkness per day. This correlation can be seen in 143 Figure 3. 144 Figure 3 145 146 147 There was also a significant positive correlation (r = 0.358, p = 0.005) between the PreE/E rate 148 and the prior month’s average minutes of darkness per day. 149 150 151 152 153 154 DISCUSSION 155 Our findings suggest a strong relationship between available sunlight in the three months and 1 156 month prior to delivery and the rate of PreE/E and further distinguish the differences in the 157 PreE/E rate when comparing summer to winter. There have also been reports of regional 158 variation around the world with reductions in pre-eclampsia the closer the region is to the 159 equator. Grand Rapids, Michigan where the data was collected is on the 43rd latitude north and 160 had an overall prevalence of 6.63%. In Beijing, China, at the 39th latitude north, the prevalence 161 of pre-eclampsia is 5.7%. [70] In Hong Kong at the 22nd latitude north the risk of pre-eclampsia 162 has been reported to be 1.6%. [71] We found a 32% increase in the PreE/E rate for births in 163 December compared to births in September. Although vitamin D levels were not obtained in 164 this study, these findings may support current theories that hypovitaminosis D plays a role in the 165 pathogenesis of PreE/E and hypovitaminosis D peaks in the fall and winter months, providing a 166 different perspective on the vitamin D connection [6-12]. Because sunshine is associated with 167 vitamin D production, vitamin D serum levels are highest in months where sunshine is most 168 prevalent, and vitamin D has been implicated in the development of hypertension and PreE/E, it 169 is likely that increased sunshine reduces the risk of preeclampsia and eclampsia. 170 Similar to findings of seasonal variation in hypertension rates in pregnant women, our findings 171 lend credence to the importance of obtaining sufficient sun exposure in the second and third 172 trimesters to help reduce a woman’s risk of PreE/E. A meta-analysis of the literature examining 173 the relationship between seasonal variation and hypertension, preeclampsia and eclampsia 174 rates reported 11 out of 14 studies showed an increase in preeclampsia in the winter months in 175 non-tropical climates [72]. Furthermore, a large Australian study has shown that the amount of 176 sunlight during the time closest to birth is a better predictor of the onset of hypertension in 177 pregnancy than the amount of sunlight at conception [73]. 178 Potential confounders 179 Future studies to evaluate the correlation between seasonal variation and PreE/E should report 180 vitamin D levels, and address potential confounders such as race, obesity, and levels of 181 exercise, depression and migraine, or maternal infection all of which may contribute to 182 hypovitaminosis D. Research so far has found considerable support for the role of diet in 183 preventing PreE/E. Studies show that the high intake of vegetables, fiber, milk, and foods rich in 184 potassium reduce the risk of PreE/E while a diet high in processed meat, calorie-rich foods, 185 sweet drinks, and salty snacks increase the risk of PreE/E [64,74-78]. Other morbidities such as 186 depression and migraine, which could have an effect on behavior, have also been examined 187 and are also associated with an increased risk of PreE/E [79]. As a consequence, while the 188 results of this study suggest an inverse association between sunlight exposure and PreE/E, this 189 may be just one factor of many contributing to this disease. 190 191 Recommendations 192 These findings suggest that pregnant women in cloudier climates may be more likely to develop 193 Pre/E in the fall and winter seasons. Due to the potentially life-threatening effects of PreE/E, it 194 may be necessary to test serum Vitamin D levels in all women at the end of the first trimester or 195 at 20 weeks gestation. Alternatively, women who have an increased risk of developing PreE/E 196 due to obesity, race, or cloudier climates should have their Vitamin D levels checked at the end 197 of the first trimester and all pregnant women should take Vitamin D supplements daily along 198 with their prenatal vitamins to help prevent hypovitaminosis D leading up to PreE/E. While the 199 cost-effectiveness of drawing vitamin D levels on pregnant women is yet to be determined, 200 lifestyle changes that promote outdoor physical activity and sun exposure may reduce the 201 morbidity associated with PreE/E. We should educate our patients to “live summer year round” 202 by encouraging pregnant women to exercise during the winter, eat more fruits and vegetables, 203 and in a region with as little sunshine as West Michigan, take a vitamin D supplement with 204 consumption guided by repeated serum blood levels. 205 206 The Institute of Medicine stated that while substantial evidence exists linking levels of vitamin D 207 with bone health, current evidence does not support other benefits of vitamin D supplementation 208 [77]. While this statement may hold true for many Americans, we believe that sufficient evidence 209 exists for the monitoring and treatment of hypovitaminosis D in specific populations. Examples 210 of such populations include African Americans, Hispanics, those with chronic kidney disease 211 and pregnant women living in areas of little sun exposure especially in the winter. Further 212 research into the role of vitamin D deficiency in the risk of PreE/E is needed. 213 214 CONCLUSION 215 216 PreE/E was 32% more common during the winter in West Michigan when compared to the 217 average during the summer. There was a moderately strong correlation with the number of 218 minutes of darkness in the three months preceding the ensuing month’s PreE/E rate. This 219 suggests a possible link to vitamin D status, but other life style influences cannot be ruled out. 220 Future studies should be carried out to assess potential confounders like race, and pregnant 221 women should be encouraged to take Vitamin D supplements daily, particularly in the fall and 222 winter seasons. Acknowledgements Ted Kuik, Kuik Computer Services Allen Shoemaker, Grand Rapids Medical Education Partners Abbreviations: ESDR = end-stage renal disease PreE/E = preeclampsia/eclampsia VDR = vitamin D receptor References: 1. Sibai BM: Hypertension. In Gabbe SG, Niebyl JR, Simpson JL. (eds): “Normal and Problem Pregnancies,” 5th ed. Philadelphia: Churchill Livingstone, pp 864-901, 2007. 2. Urquia ML, Ying I, Glazier RH, Berger H, De Souza LR, Ray JG: Serious Preeclampsia Among Different Immigrant Groups. J Obstet Gynaecol Can 34:348–352, 2012. 3. Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF: WHO analysis of causes of maternal death: a systematic review. Lancet 367:1066-1074, 2006. 4. Duley L: The global impact of pre-eclampsia and eclampsia. Semin Perinatol 33:130137, 2009 . 5. MacKay AP, Berg CJ, Atrash HK: Pregnancy-related mortality from preeclampsia and eclampsia. Obstet Gynecol 97:533-553, 2001. 6. Bikle D: Nonclassic actions of vitamin D. J Clin Endocrinol Metab 94:26-34, 2009. 7. Bodnar LM, Catov JM, Simhan HN, Holick MF, Powers RW, Roberts JM: Maternal vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab 92:3517-3522, 2007. 8. Baker AM, Haeri S, Camargo CA Jr, Espinola JA, Stuebe AM. A nested case-control study of midgestation vitamin D deficiency and risk of severe preeclampsia. J Clin Endocrinol Metab. 95(11):5105-9 2010. 9. Zhao G, Ford ES, Tsai J, Li C, Croft JB. Factors Associated with Vitamin D Deficiency and Inadequacy among Women of Childbearing Age in the United States. Obstet Gynecol 2012: 691486 2012. 10. Rucker D, Allan JA, Fick GH, Hanley DA. Vitamin D insufficiency in a population of healthy western Canadians. CMAJ 166:1517-24 2002. 11. Gostine ML, Davis FN. Vitamin D deficiencies in pain patients. Prac Pain Mgmt. (July/August): 16-19, 2006. 12. Ranking of Cities based on % annual possible sunshine in descending order from most to least average possible sunshine. 2004 [cited 2012 Feb 9]; Available from: http://www.ncdc.noaa.gov/oa/climate/online/ccd/pctposrank.txt. 13. Chambers JC, Fusi L, Malik IS, Haskard DO, De Swiet M, Kooner JS: Association of maternal endothelial dysfunction with preeclampsia. JAMA 285:1607-1612, 2001. 14. Bikle D: Nonclassic actions of vitamin D. J Clin Endocrinol Metab 94:26-34, 2009. 15. Gorham ED, Garland CF, Garland FC, Grant WB, Mohr SB, Lipkin M, Newmark HL, Giovannucci E, Wei M, Holick MF: Optimal vitamin D status for colorectal cancer prevention: a quantitative meta analysis. Am J Prev Med 32:210-216, 2007. 16. Garland CF, Garland FC, Gorham ED: Calcium and vitamin D. Their potential roles in colon and breast cancer prevention. Ann N Y Acad Sci 889:1207-1221, 1999. 17. Mizwicki MT, Norman AW: The vitamin D sterol-vitamin D receptor ensemble model offers unique insights into both genomic and rapid-response signaling. Sci Signal 2:re4, 2009. 18. Anderson JL, May HT, Horne BD, Bair TL, Hall NL, Carlquist JF, Lappé DL, Muhlestein JB; Intermountain Heart Collaborative (IHC) Study Group: Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population. Am J Cardiol 106:963-968, 2010. 19. de Borst MH, de Boer RA, Stolk RP, Slaets JP, Wolffenbuttel BH, Navis G: Vitamin D deficiency: universal risk factor for multifactorial diseases? Curr Drug Targets 12:97-106, 2011. 20. Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, Benjamin EJ, D'Agostino RB, Wolf M, Vasan RS: Vitamin D deficiency and risk of cardiovascular disease. Circulation 117:503-511, 2008. 21. Giovannucci E, Liu Y, Hollis BW, Rimm EB: 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med 168:1174-1180, 2008. 22. Pilz S, Dobnig H, Fischer JE, Wellnitz B, Seelhorst U, Boehm BO, März W: Low vitamin d levels predict stroke in patients referred to coronary angiography. Stroke 39:26112613, 2008. 23. Pilz S, März W, Wellnitz B, Seelhorst U, Fahrleitner-Pammer A, Dimai HP, Boehm BO, Dobnig H: Association of vitamin D deficiency with heart failure and sudden cardiac death in a large cross-sectional study of patients referred for coronary angiography. J Clin Endocrinol Metab 93:3927-3935, 2008. 24. Pilz Pilz S, Dobnig H, Nijpels G, Heine RJ, Stehouwer CD, Snijder MB, van Dam RM, Dekker JM: Vitamin D and mortality in older men and women. Clin Endocrinol (Oxf) 71(5):666-672, 2009. 25. Pilz S, Tomaschitz A, Ritz E, Pieber TR: Vitamin D status and arterial hypertension: a systematic review. Nat Rev Cardiol 6:621-630, 2009. 26. Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, Wellnitz B, Kinkeldei J, Boehm BO, Weihrauch G, Maerz W: Independent association of low serum 25-hydroxyvitamin d and 1,25-dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med. 168:1340-1349, 2008. 27. Ginde AA, Scragg R, Schwartz RS, Camargo CA Jr: Prospective study of serum 25hydroxyvitamin D level, cardiovascular disease mortality, and all-cause mortality in older U.S. adults. J Am Geriat 57:1595-1603, 2009. 28. Zittermann A, Gummert JF, Börgermann J: The role of vitamin D in dyslipidemia and cardiovascular disease. Curr Pharm Des 17:933-942, 2011. 29. Martini LA, Wood RJ: Vitamin D and blood pressure connection: update on epidemiologic, clinical, and mechanistic evidence. Nutr Rev 66:291-297, 2008. 30. Wu SH, Ho SC, Zhong L: Effects of Vitamin D supplementation on blood pressure. South Med J 103:729-737, 2010. 31. Yuan W, Pan W, Kong J, Zheng W, Szeto FL, Wong KE, Cohen R, Klopot A, Zhang Z, Li YC: 1,25-dihydroxyvitamin D3 suppresses renin gene transcription by blocking the activity of the cyclic AMP response element in the renin gene promoter. J Biol Chem 282:29821-29830, 2007. 32. Xiang W, Kong J, Chen S, Cao LP, Qiao G, Zheng W, Liu W, Li X, Gardner DG, Li YC: Cardiac hypertrophy in vitamin D receptor knockout mice: role of the systemic and cardiac renin-angiotensin systems. Am J Physiol Endocrinol Metab 288:E125-132, 2005. 33. Scragg R: Seasonality of cardiovascular disease mortality and the possible protective effect of ultra-violet radiation. Int J Epidemiol 10:337-341, 1981. 34. Barnett AG, de Looper M, Fraser JF: The seasonality in heart failure deaths and total cardiovascular deaths. Aust NZ J Public Health. 32:408-413, 2008. 35. cardiovascular deaths. Aust NZ J Public Health. 32:408-413, 2008. 36. Gallerani M, Boari B, de Toma D, Salmi R, Manfredini R: Seasonal variation in the occurrence of deep vein thrombosis. Med Sci Monit 10:CR191-CR196, 2004. 37. Gallerani M, Boari B, Smolensky MH, Salmi R, Fabbri D, Contato E, Manfredini R: Seasonal variation in occurrence of pulmonary embolism: analysis of the database of the Emilia-Romagna region, Italy. Chronobiol Int 24:143-160, 2007. region, Italy. Chronobiol Int 24:143-160, 2007. 38. Qiao G, Kong J, Uskokovic M, Li YC: Analogs of 1alpha,25-dihydroxyvitamin D(3) as novel inhibitors of renin biosynthesis. J Steroid Biochem Mol Biol 96:59-66, 2005. 39. Kong J, Li YC: Effect of ANG II type I receptor antagonist and ACE inhibitor on vitamin D receptor-null mice. Am J Physiol Regul integr Comp Physiol 285:R255-R261, 2003. 40. Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP: 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest 110:229-238, 2002. 41. Li YC: Vitamin D regulation of the renin-angiotensin system. J Cell Biochem 88:327-331, 2003. 42. Bucharles S, Barberato SH, Stinghen AE, Gruber B, Meister H, Mehl A, Piekala L, Dambiski AC, Souza A, Olandoski M, Pecoits-Filho R: Hypovitaminosis D is associated with systemic inflammation and concentric myocardial geometric pattern in hemodialysis patients with low iPTH levels. Nephron Clin Pract. 118:c384-c391, 2011. 43. Schleithoff SS, Zittermann A, Tenderich G, Berthold HK, Stehle P, Koerfer R: Vitamin D supplementation improves cytokine profiles in patients with congestive heart failure: a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr 83:754-759, 2006. 44. Tan X, Wen X, Liu Y: Paricalcitol inhibits renal inflammation by promoting vitamin D receptor-mediated sequestration of NF-kappaB signaling. J Am Soc Nephrol 19:1741-1752, 2008. 45. Alborzi Alborzi P, Patel NA, Peterson C, Bills JE, Bekele DM, Bunaye Z, Light RP, Agarwal R: Paricalcitol reduces albuminuria and inflammation in chronic kidney disease: a randomized double-blind pilot trial.. Hypertension 52:249-255, 2008. 46. Wang P, Anderson PO, Chen S, Paulsson KM, Sjögren HO, Li S: Inhibition of the transcription factors AP-1 and NF-kappaB in CD4 T cells by peroxisome proliferatoractivated receptor gamma ligands. Int Immunopharmacol 1:803-812, 2001. 47. Lu X, Farmer P, Rubin J, Nanes MS: Integration of the NfkappaB p65 subunit into the vitamin D receptor transcriptional complex: identification of p65 domains that inhibit 1,25dihydroxyvitamin D3-stimulated transcription. J Cell Biochem 92:833-848, 2004. 48. Guijarro C, Egido J: Transcription factor-kappa B (NF-kappa B) and renal disease. Kidney Int 59:415-424, 2001. 49. Hyppönen E: Vitamin D for the prevention of preeclampsia? A hypothesis. Nutr Rev 63:225-232, 2005. 50. Bodnar LM, Catov JM, Simhan HN, Holick MF, Powers RW, Roberts JM: Maternal vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab 92:3517-3522, 2007. 51. Mannion CA, Gray-Donald K, Koski KG: Association of low intake of milk and vitamin D during pregnancy with decreased birth weight. CMAJ 174:1273-1277, 2006. 52. Zhang C, Qiu C, Hu FB, David RM, van Dam RM, Bralley A, Williams MA: Maternal plasma 25-hydroxyvitamin D concentrations and the risk for gestational diabetes mellitus. PLoS One 3:e3753, 2008. 53. Merewood A, Mehta SD, Chen TC, Bauchner H, Holick MF: Association between vitamin D deficiency and primary cesarean section. J Clin Endocrinol Metab 94:940-945, 2008. 54. Bodnar LM, Krohn MA, Simhan HN: Maternal vitamin D deficiency is associated with bacterial vaginosis in the first trimester of pregnancy. J Nutr 139:1157-1161, 2009. 55. Barrera D, Avila E, Hernández G, Halhali A, Biruete B, Larrea F, Díaz L: Estradiol and progesterone synthesis in human placenta is stimulated by calcitriol. J Steroid Biochem Mol Biol 103:529-532, 2007. 56. Barrera D, Avila E, Hernández G, Méndez I, González L, Halhali A, Larrea F, Morales A, Díaz L: Calcitriol affects hCG gene transcription in cultured human syncytiotrophoblasts. Reprod biol Endocrinol 6:3, 2008. 57. Stephanou A, Ross R, Handwerger S: Regulation of human placental lactogen expression by 1,25-dihydroxyvitamin D3. Endocrinology 135:2651-2656, 1994. 58. Diaz Díaz L, Noyola-Martínez N, Barrera D, Hernández G, Avila E, Halhali A, Larrea F: Calcitriol inhibits TNF-alpha-induced inflammatory cytokines in human trophoblasts. J Reprod Immunol 81:17-24, 2009. 59. Liu N, Kaplan AT, Low J, Nguyen L, Liu GY, Equils O, Hewison M: Vitamin D induces innate antibacterial responses in human trophoblasts via an intracrine pathway. Biol Reprod 80:398-406, 2009. 60. Halhali A, Acker GM, Garabédian M: 1,25-Dihydroxyvitamin D3 induces in vivo the decidualization of rat endometrial cells. J Reprod Fertil 91:59-64, 1991. 61. Du H, Daftary GS, Lalwani SI, Taylor HS: Direct regulation of HOXA10 by 1,25-(OH)2D3 in human myelomonocytic cells and human endometrial stromal cells. Mol Endocrinol 19:2222-2233, 2005. 62. Zehnder D, Evans KN, Kilby MD, Bulmer JN, Innes BA, Stewart PM, Hewison M: The ontogeny of 25-hydroxyvitamin D(3) 1alpha-hydroxylase expression in human placenta and decidua. Am J Pathol 161:105-114, 2002. 63. Rigby WF, Stacy T, Fanger MW: Inhibition of T lymphocyte mitogenesis by 1,25dihydroxyvitamin D3 (calcitriol). J Clin Invest 74:1451-1455, 1984. 64. Chen S, Sims GP, Chen XX, Gu YY, Chen S, Lipsky PE: Modulatory effects of 1,25dihydroxyvitamin D3 on human B cell differentiation J Immunol 179:1634-1647, 2007. 65. Lemire JM, Adams JS, Sakai R, Jordan SC: 1 alpha,25-dihydroxyvitamin D3 suppresses proliferation and immunoglobulin production by normal human peripheral blood mononuclear cells J Clin Invest 74:657-661, 1984. 66. Lemire JM, Archer DC, Beck L, Spiegelberg HL: Immunosuppressive actions of 1,25dihydroxyvitamin D3: preferential inhibition of Th1 functions J Nutr 125:1704S-1708S, 1995. 67. Piccinni MP, Scaletti C, Maggi E, Romagnani S: Role of hormone-controlled Th1- and Th2-type cytokines in successful pregnancy. J Neuroimmunol 109:30-33, 2000. 68. Haugen M, Brantsaeter AL, Trogstad L, Alexander J, Roth C, Magnus P, Meltzer HM: Vitamin D supplementation and reduced risk of preeclampsia in nulliparous women. Epidemiology 20:720-726, 2009. 69. TePoel MR, Saftlas AF, Wallis AB. Association of seasonality with hypertension in pregnancy: a systematic review. J Reprod Immunol 89:140-152, 2011. 70. Zhonghua F, Chan K, Za Z. Study on clinical risk of maternal underlying medical conditions and onset of preeclampsia. 47(6):405-11. 2012 71. Tam WH, Sahota DS, Lau TK, Li CY, Fung TY. Seasonal variation in pre-eclamptic rate and its association with the ambient temperature and humidity in early pregnancy. Gynecol Obstet Invest. 66(1):22-6. 2008. 72. Algert CS, Roberts CL, Shand AW, et al. Seasonal variation in pregnancy hypertension is correlated with sunlight intensity. Am J Obstet Gynecol 203:215.e1-5, 2010. 73. Brantsaeter AL, Haugen M, Samuelsen SO, Torjusen H, Trogstad L, Alexander J, Magnus P, Meltzer HM: A dietary pattern characterized by high intake of vegetables, fruits, and vegetable oils is associated with reduced risk of preeclampsia in nulliparous pregnant Norwegian women. J Nutr 139:1162-1168, 2009. 74. Clausen T, Slott M, Solvoll K, Drevon CA, Vollset SE, Henriksen T: High intake of energy, sucrose, and polyunsaturated fatty acids is associated with increased risk of preeclampsia. Am J Obstet Gynecol 185:451-458, 2001. 75. Oken E, Ning Y, Rifas-Shiman SL, Rich-Edwards JW, Olsen SF, Gillman MW: Diet during pregnancy and risk of preeclampsia or gestational hypertension. Ann Epidemiol 17:663-668, 2007. 76. Qiu C, Coughlin KB, Frederick IO, Sorensen TK, Williams MA: Dietary fiber intake in early pregnancy and risk of subsequent preeclampsia. Am J Hypertens 21:903-909, 2008. 77. Frederick IO, Williams MA, Dashow E, Kestin M, Zhang C, Leisenring WM: Dietary fiber, potassium, magnesium and calcium in relation to the risk of preeclampsia. J Reprod Med 50:332-344, 2005. 78. Cripe SM, Frederick IO, Qiu C, Williams MA: Risk of preterm delivery and hypertensive disorders of pregnancy in relation to maternal co-morbid mood and migraine disorders during pregnancy. Paediatr Perinat Epidemiol 25:116-123, 2011. 79. Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Institute of Medicine: Summary. In Ross C, Taylor CL, Yaktine AL, Del Valle HB, (eds): “Dietary Reference Intakes for Calcium and Vitamin D.” Washington DC: National Academies Press, pp 1-14, 2010. Table 1 ICD-9a Codes Used to Calculate Preeclampsia/Eclampsia Rate Code Description 642.4 Mild or Unspecified Pre-eclampsia 642.5 Severe Pre-eclampsia 642.6 Eclampsia 642.7 Pre-eclampsia or eclampsia superimposed on pre-existing hypertension a International Classification of Diseases Figure Legends Figure 1 The 95% Confidence intervals for the Preeclampsia/Eclampsia rate over the five-year period of the study. Comparison of the peak rate in December to the trough rate in September and that in the low sun months of December through April to the high sun months of July through September. Figure 2 Comparison of seasonal pattern of Preeclampsia/Eclampsia rate with that of average minutes of darkness (no sunlight) per day in prior three-month period. Figure 3 Scatter plot with best-fit line showing where each of the 60 months in the five-year period analyzed fall in terms of Preeclampsia/Eclampsia rate and average minutes of darkness (no sunlight) in the prior three-month period.