VATS Simulator Project
advertisement

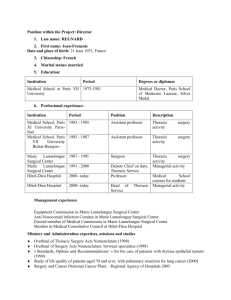
VATS Simulator Project Prof. Vinesh Raja (WMG), Prof. Babu Naidu (Heart of England Regional Thoracic Surgery Department) and Tracey Starkey-Moore (Hollier Medical Simulation Centre) PhD or EngD Lung Cancer kills over 30,000 people each year in the UK, accounting for 5.6% of all UK deaths. This is greater than deaths from the next three most common malignancies combined (breast, colorectal and prostate cancers). Survival rates for lung cancer in the UK are very poor and have not improved in the last thirty years. For patients diagnosed between 1993 and 1995 and followed up to 2000, only 5.5% are alive after 5 years. Surgery remains the only cure and surgical resection rates, a marker of outcome are lower in the UK (11%) compared with the rest of Europe (17%) and North America (21%) and vary by three-fold between health authorities in England. Patients with lung cancer in the UK present at a later stage and have a higher co-morbidity than patients in comparable European cities. One approach to dealing with the poor surgical rate and overall survival is to adopt minimally invasive surgery in higher risk patients whose morbidity and mortality with open surgery may have been prohibitive. This is even more important now because the draft BTS guidelines on selection of patients with lung cancer surgery has lowered the threshold for surgery such that less fit patients will now be offered surgery Video assisted thoracic surgery (VATS) or minimally invasive surgery is associated with post operative reduction in pain, loss of lung function and Immune activation. The length of hospital stay is also reduced after specific procedures. Though VATS has become standard practice for specific procedures such as in the treatment pneumothorax, it has been slow to be adopted in the curative treatment of lung cancer. Fears that oncological clearance may be hampered resulting in a lower long term survival and higher recurrence rates following VATS have been refuted. Indeed metaanalysis suggests that long term survival may be better after lung cancer resection via VATS. Only 2.5 % of all major lung resections are performed via VATS but in individual centres in the hands of experts this approaches 80%. One of the major barriers to the use of VATS lung resection is the inadequate training available to minimize the effects of the learning curve. Though industry sponsored animal training facilities in Europe are available, access is limited as is the excellent mentorship of experienced surgeons. Current models of VATS simulation rely on physical reality ‘Box trainers’ which are inadequate at providing realistic scenarios. Hence there is a need to build more realistic simulators for training of future thoracic surgeons. This project aims to develop a realistic VATS simulator for training of new thoracic surgeons and for experienced surgeon to practice prior to a real surgery.