Anti-inflammatory steroids
advertisement
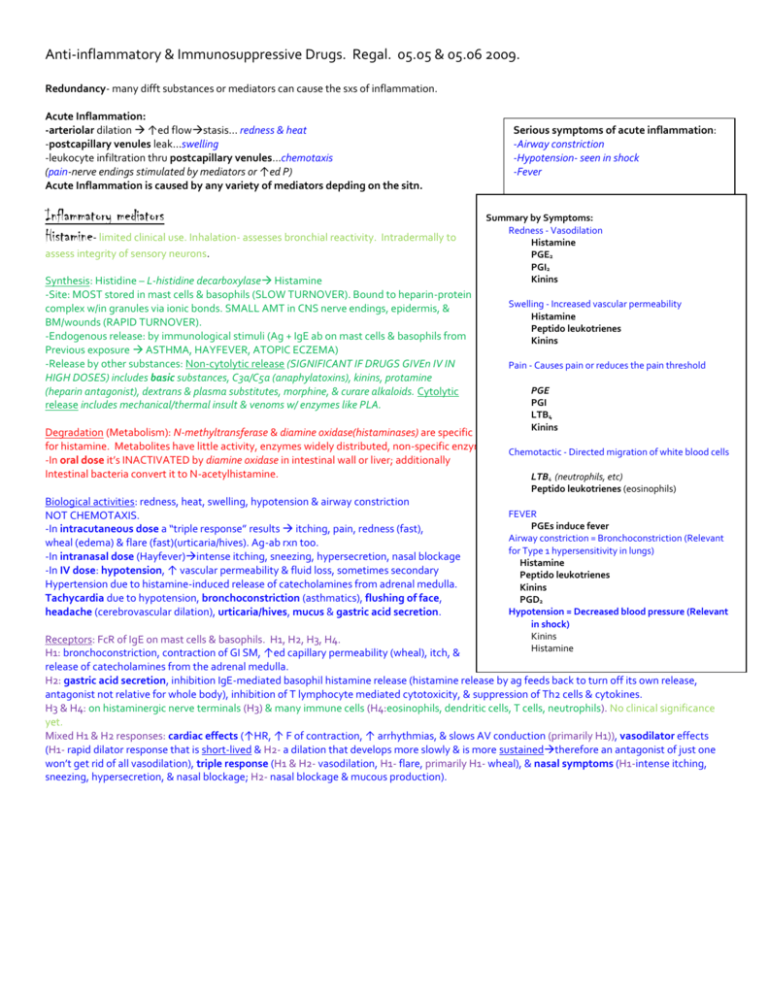
Anti-inflammatory & Immunosuppressive Drugs. Regal. 05.05 & 05.06 2009. Redundancy- many difft substances or mediators can cause the sxs of inflammation. Acute Inflammation: -arteriolar dilation ↑ed flowstasis… redness & heat -postcapillary venules leak…swelling -leukocyte infiltration thru postcapillary venules…chemotaxis (pain-nerve endings stimulated by mediators or ↑ed P) Acute Inflammation is caused by any variety of mediators depding on the sitn. Inflammatory mediators Histamine- limited clinical use. Inhalation- assesses bronchial reactivity. Intradermally to assess integrity of sensory neurons. Synthesis: Histidine – L-histidine decarboxylase Histamine -Site: MOST stored in mast cells & basophils (SLOW TURNOVER). Bound to heparin-protein complex w/in granules via ionic bonds. SMALL AMT in CNS nerve endings, epidermis, & BM/wounds (RAPID TURNOVER). -Endogenous release: by immunological stimuli (Ag + IgE ab on mast cells & basophils from Previous exposure ASTHMA, HAYFEVER, ATOPIC ECZEMA) -Release by other substances: Non-cytolytic release (SIGNIFICANT IF DRUGS GIVEn IV IN HIGH DOSES) includes basic substances, C3a/C5a (anaphylatoxins), kinins, protamine (heparin antagonist), dextrans & plasma substitutes, morphine, & curare alkaloids. Cytolytic release includes mechanical/thermal insult & venoms w/ enzymes like PLA. Serious symptoms of acute inflammation: -Airway constriction -Hypotension- seen in shock -Fever Summary by Symptoms: Redness - Vasodilation Histamine PGE2 PGI2 Kinins Swelling - Increased vascular permeability Histamine Peptido leukotrienes Kinins Pain - Causes pain or reduces the pain threshold PGE PGI LTB4 Kinins Degradation (Metabolism): N-methyltransferase & diamine oxidase(histaminases) are specific for histamine. Metabolites have little activity, enzymes widely distributed, non-specific enzymes exist too. Chemotactic - Directed migration of white blood cells -In oral dose it’s INACTIVATED by diamine oxidase in intestinal wall or liver; additionally Intestinal bacteria convert it to N-acetylhistamine. LTB4 (neutrophils, etc) Peptido leukotrienes (eosinophils) Biological activities: redness, heat, swelling, hypotension & airway constriction NOT CHEMOTAXIS. -In intracutaneous dose a “triple response” results itching, pain, redness (fast), wheal (edema) & flare (fast)(urticaria/hives). Ag-ab rxn too. -In intranasal dose (Hayfever)intense itching, sneezing, hypersecretion, nasal blockage -In IV dose: hypotension, ↑ vascular permeability & fluid loss, sometimes secondary Hypertension due to histamine-induced release of catecholamines from adrenal medulla. Tachycardia due to hypotension, bronchoconstriction (asthmatics), flushing of face, headache (cerebrovascular dilation), urticaria/hives, mucus & gastric acid secretion. FEVER PGEs induce fever Airway constriction = Bronchoconstriction (Relevant for Type 1 hypersensitivity in lungs) Histamine Peptido leukotrienes Kinins PGD2 Hypotension = Decreased blood pressure (Relevant in shock) Kinins Histamine Receptors: FcR of IgE on mast cells & basophils. H1, H2, H3, H4. H1: bronchoconstriction, contraction of GI SM, ↑ed capillary permeability (wheal), itch, & release of catecholamines from the adrenal medulla. H2: gastric acid secretion, inhibition IgE-mediated basophil histamine release (histamine release by ag feeds back to turn off its own release, antagonist not relative for whole body), inhibition of T lymphocyte mediated cytotoxicity, & suppression of Th2 cells & cytokines. H3 & H4: on histaminergic nerve terminals (H3) & many immune cells (H4:eosinophils, dendritic cells, T cells, neutrophils). No clinical significance yet. Mixed H1 & H2 responses: cardiac effects (↑HR, ↑ F of contraction, ↑ arrhythmias, & slows AV conduction (primarily H1)), vasodilator effects (H1- rapid dilator response that is short-lived & H2- a dilation that develops more slowly & is more sustainedtherefore an antagonist of just one won’t get rid of all vasodilation), triple response (H1 & H2- vasodilation, H1- flare, primarily H1- wheal), & nasal symptoms (H1-intense itching, sneezing, hypersecretion, & nasal blockage; H2- nasal blockage & mucous production). Synthesis: AA comes from phospholipids in the cell membrane. PLA2 is needed. In future may see PLA2 inhibitors. IMPT limiting step. Note: OOH & epoxide in first two steps. FLAP- transport of 5-lipoxygenase from cytosol to the membrane LTC 4 synthase (mast cell or basophil) OR glutathione S transferase (endothelial cell, SM cell, etc) Site: lipoxygenase products are in many cells & tissues. Other enzymes are found in myelomonocytic origin as well as endothelial cells/platelets, which do not have 5-lipoxygenase. LTA4 is made in 5-lipoxygenase containing cells & has 3 difft fates: -LTB4 formation in a cell which contains LTA4 hydrolase (PMN). -LTC4 formation in a cell which contains either LTC4 synthase (mast cell or basophil) or glutathione S transferase (endothelial cell, SM cell).It is then transported out of cell & converted to LTD4 or LTB4. -transcellular metabolism in other cells to LTC4 (endothelial cell, SM cell) or LTB4 (rbc & platelet). LTB4 Biological activities: chemotactic (PMNs), leukocyte adhesion, enzyme release, ROS production & ↓es pain threshold. Found in synovial fluid of RA & gout. Degradation: oxidized by enzymes in PMN’s & other oxidative enzymes to inactive cmpds. Receptors: LTB4 Receptor on other cell types. LTC4, LTD4, LTE4 (Peptido leukotrienes) Biological activities: Cys LTR1bronchoconstriction, ↑ vascular permeability (swelling), chemotaxis (eosinophils), ↑ mucous production, dendritic cell maturation & migration, SM proliferation. Cys LTR2 endothelial cell & macrophage activation, as well as fibrosis. LTC4/LTD4impt in asthma. SLOW REACTING SUBSTANCE OF ANAPHYLAXIS (SRS-A). Degradation: LTE4 is excreted in the urine or acetylated & excreted in the bile. Receptors: Cys LTR1 preferentially w/ LTD4 airway constriction; is blocked by current receptor antagonists, while cys LTR2 preferentially w/ LTC4 & LTD4 cell activation. Phospholipids in cell membrane Prostanoids Synthesis: By phospholipase A2, which takes off the FA at C2. Other acylhydrolases release AA from memb phospholipids. The availability of AA is a control step in the production of prostaglandins & thromboxane; these are derivatives of prostanoic acid (20C FA w/ cyclopentane ring). Subscripts = # doubles bonds. For PG2’s the precursor is AA. For PG1’s the precursor is 8,11,14 – eicosatrienoic acid (ddddihomo-gammalinolenic acid). COX-1: found in platelets, CONSTITUTIVELY EXPRESSED in most cells & protects gastric Mucosa. COX-2: Not found in platelets, expressed constitutively in brain & kidney, but can be INDUCED BY certain serum factors, cytokines, & gfs in other tissues & at sites of inflam. MORE IMPT ISOZYMEPROSTAGLANDINS & THROMBOXANE in inflammation. Prostaglandins can also be the mediators of the mediators. Degradation of cyclooxygenase products: unstable molecules w/ short half lives. Spontaneous chemical hydrolysis. Uptake into cells by transport protein & subsequent enzymatic degradation. Biological activities: local actions (autocoids). Receptors: On cell membrane- dictate action of cyclooxygenase product. Five major types of receptors for prostaglandins (seven transmemb G protein coupled) -DP (PGD), FP (PGF), IP (PGI2), TP (TXA2) & EP (PGE). -Unique Gs,GiGq G-proteins for difft PG receptor subtypes -Unique second messangers for difft PG receptor subtypes Phospholipase A2 Epoxygenase products (vasodilators) Isoprostanes (vasoconstrictors?) Cyt P450 Arachidonic Acid Cyclooxygenase COX Prostanoids (PG & TX) Lipoxygenase LOX Leukotrienes PGD2 Synthesis: produced by MAST CELLS Biological activities: bronchoconstriction Receptor: DP PGE2 Biological activities: vasodilate (redness), ↑ vascular permeability (& synergize w/ PGI2), CAUSE pain (lower threshold- synergizes w/ PGI2), & FEVER (IL-1Pg’sFever). Receptor: EP PGF2 Direction PGH2 goes dpds on what is in the cell. Cytokines Bradykinin Receptor: FP Prostaglandins Pain Other mediators PGI2 (prostacyclin)- Synthesis: produced by ENDOTHELIUM Biological activities: vasodilate (redness), ↑ vascular permeability (& synergize w/ PGE), CAUSE pain (lower threshold- synergizes w/ PGE), OPPOSE platelet aggregation, & vasodilation (SM dilation). Second messanger is cAMP. Receptor: IP, Gs TXA2 (thromboxane)- Synthesis: produced by PLATELETS. Biological activities: bronchoconstriction, CAUSE platelet aggregation & vasoconstriction. Second messanger is IP3/DAG/Ca2+. Receptor: TP, Gq Kinins- relevance to be detmd. Deficiency of HMW kininogen or prekallikreinclotting & fibrinolytic defects w/ ↓ kinin. Kallikrein inhibitors & kinin receptor antagonists are useful in C1 inhibitor deficiency (HAE)- recurrent episodes of localized edema in skin, GI, or larynx. C1INH is primary inhibitor of kallikrein. Excess kinin also is assoctd w/ pain in dental extractions, nasal allergy or rhinitis assoctd w/ rhinoviral infection. Interrelationship btwn Kinin, complement, coagulation & fibrinolytic pathways- all intertwined. Synthesis-NOT in cells rather in extracellular blood or interstitial fluid. Injury initiates this pathway. HFa Plasmin Prekallikrein Plasma kallikrein HMW kininogen Kininase I & II Tissue kallikrein LMW kininogen Hfa=activated Hageman factor, part of clotting cascade. Plasmin digests fibrin. Bradykinin (9 a.a.) Kallidin (10 a.a.) Biological activities: everything + strong vasodilator resulting in hypotension. NOT A MAJOR CHEMOTACTIC AGENT. Degradation: Kininase I- Carboxypeptidase N or anaphylatoxin inactivator removes the carboxy terminal arginine Kininase II- Angiotensin converting enzyme (ACE) or dipeptide dihydrolase cleaves btwn Pro-Phe. Works at both sites, inhibiting vasoconstriction & allowing vasodilation. Bradykinin (Arg….ProPheArg) Biological activities: Mediators w/ inflammatory activities. Kallidin (LysArg…..ProPheArg) Biological activities: Mediators w/ inflammatory activities. Receptors: Via B2 Receptor: Kallidin & Bradykinin more active than w/o removal of arg. Potent vasodilators, hypotension, ↑ed capillary permeability & edema formation, CAUSE pain, slowly contract the gut SM, bronchoconstriction, release catecholamines form the adrenal medulla, & release PGs. Via B1 Receptor: Des-arg Bradykinin & Kallidin are more active. Chronic inflammatory effects, induced after trauma, maybe involved in cytokine production & more long term effects, hypotension & pain. Antihistamines (H1) Mechanisms of action- target a single mediator & are inverse agonists (preferential affinity for inactive state of histamine 1 Gprotein receptor”nothing happens”) Note: historically referred to as competitive antagonists of histamine. THINK OF SHIFT DOSE RESPONSE CURVE. NO BENEFITS FOR COLDS! Mostly, antihistamines shift the agonist doseresponse curve to the right & look like a competitive antagonist. Response Histamine Old Antihistamines: Mechanism of action: blockade of H1, muscarinic, alpha adrenergic, & SE receptors. Used as ophthalmic solutions, for allergies (allergic rhinitis, urticaria, atopic dermatitis), motion sickness, & NOT FOR ASTHMA. Side effects: -Sedation including potentiation of CNS depressants such as barbs or alcohol, dizziness, incoordination, blurred vision, nervousness, insomnia, tremors, & may interfere w/ learning or work productivity. -Drying of secretions: due to anticholinergic properties (atropine-like) -GI disturbances: reduced by giving the drug w/ meals & not necessarily related to H1 antagonism. Distribution: Well absorbed orally, widely distributed including CNS. Not recognized by the P-glycoprotein efflux pump on the endothelial cells in the vasculature of the CNS. Therefore, they are NOT PUMPED OUT OF THE CNS. Metabolism/excretion: transformed to inactive metabolites in the liver & excreted in the urine. Toxicity: topical application not recommended bc allergic dermatitis can devp. Acute poisoning resembles atropine poisoning w/ fixed-dilated pupils, flushed face, fever, & dry mouth; also includes excitation, hallucinations, incoordination, convulsions; terminal use results in coma & cardiorespiratory collapse. Tx for acute poisoning is symptomatic and supportive. Diphenhydramine - Tylenol PM: low incidence of GI side effects & sedation. Good for motion sickenss (has to do w/ ACh antagonis) bc of antimuscarinic properties. Use if want sedation. Tripelennamine – GI side effects are common, less central effects, fewer anti-cholinergic effects. Chlorpheniramine – Suitable for daytime use. Newer Non-sedating Antihistamines: Mechanism of action: Used for allergies (allergic rhinitis, urticaria, atopic dermatitis), & NOT FOR ASTHMA. Side effects: -Minimal anticholinergic properties -No sedation or drying of secretions -Do not potentiate effects of CNS depressants such as alcohol or barbs. Distribution: ONLY SMALL AMTS CROSS THE BBB. These do have an affinity for P-glycoprotein efflux pump in endothelium of vasculature in CNS, therefore they are pumped out. Toxicity: CARDIOTOXICITY W/ ORIGINAL NON-SEDATIN ANTIHISTAMINES, drugs currently used are NOT cardiotoxic. Cetirizine Fexofenadine Loratadine (now over the counter) Newer H2 antihistamines: used for ulcers & gastric hypersecretory states. Inverse agonists. Leukotriene modifiers Mechanism of action- target a single mediator/inhibitors. Tx of chronic bronchial asthma & allergic rhinitis. Zileuton Mechanism of action- INHIBITS THE ENZYME 5-LIPOXYGENASE & thus prevents synthesis of LTB4 as well as the peptide-leukotrienes. Second line for tx of chronic asthma. Metabolism/Elimination: cyt P450 Toxicity: drug interactions, hepatic toxicity. Zafirlukast Mechanism of action- leukotrine receptor antagonists (esp LTD4 receptor, Cys LTR1). INHIBITS CYT P450 isozyme. Use in chronic asthma. Toxicity: drug interactions Montelukast Mechanism of action- leukotrine receptor antagonists (esp LTD4 receptor, Cys LTR1). Use of asthma. NSAID Mechanism of action- target multiple mediators, but mostly stop cyclooxygenase synthesis & inhibit COX-1 & COX-2. Analgesic, antipyretic (Inflammationcytokines (IL-1)PGE2HypothalamusFever, so inhibit PGE2 production to prevent fever), & anti-inflammatory (don’t arrest the progression of pathological injury). Side effects: -GI ulceration bc of inhibition of PG synthesis, sometimes a secondary anemia can result, alcohol increases GI bleeding, can be reduced w/ COX 2 inhibitors) -Prolongation of gestation bc PGs help initiate labor & inhibiting COX1 or COX2 PREVENTS LABOR. -COX1 inhibition in the plateletPREVENTS PLATELET AGGREGATION & TXA FORMATION. INCREASES BLEEDING TIME. -COX2 inhibition does not do this to same extent. Toxicity- Large daily doses for years can result in analgesic abuse nephropathy- fluid retention, diminished sodium excretion, nitrogen retention, hyperkalemia, oliguria (scanty urine), anuria. May lead to papillary necrosis & chronic interstitial neprhritis. Hepatitis can happen too. Acetylsalicylate (aspirin) Mechanism of action: Irreversibly acetylates COX 1 (inactivates). The platelet cannot make more cyclooxygenase. The effect of aspirin lasts the lifetime of the platelet (8-10 days). Toxicity: Hypersensitivity- in 3-10% of asthmatics, sxs include rhinitis, urticaria, asthma, & laryngeal edema. Possible mechanisms include shift to lipoxygenase pathway resulting in increase leukotriene production. Have also seen upregulation of Cys LTR1. Decreases in PGE2 may also decrease the blockage of 5-lipoxygenase. Also associated w/ REYE SYNDROME bc anti-inflammatory does are close to toxic dosesencephalopathy & fatty liver following viral infection in kids. Can result in central hyperventival & intoxication & tinnitus w/ overdose. Ibuprofen-OTC Side effects: fewer GI than aspirin Toxicity: Hepatitis. Naproxen-OTC Toxicity: Hepatitis Diflunisal (also a salicylate) Indomethacin Most potent NSAID, severe frontal headache & blood dxs Toxicity: Hepatitis Sulindac Toxicity: Hepatitis Ketoprofen- related to Ibuprofen Piroxicam- once a day administration, can cause serious GI bleeding Drugs that inhibit cyclooxygenase: -NSAIDs -Cyclo-oxygenase inhibitors -Aspirin-like drugs -Analgesic, anti-inflammatory, anti-pyretic. Names of drugs that Inhibit COX: -Aspirin -tNSAIDs Ibuprofen (OTC) Naproxen (OTC) Diflunisal Indomethacin Sulindac Ketoprofen Piroxicam -Selective COX2 inhibitors: Celecoxib -Acetaminophen- not antiinflammatory COX2 Inhibitor Celecoxib-risk of thrombosis 200mb/day Mechanism of action: 10-20X MORE SELECTIVE FOR COX2 inhibition. Safe in aspirin hypersensitive indls. No inhibition of platelet fxn, so thromboxane can be produced. Less likely gastric ulceration & intolerance. Toxicity: Reduce the production of prostacyclin (inhibitor of platelet aggregation) by endothelial cells. Balance favors platelet aggregation due to ↓ed PGI2 (prostacyclin). Acetaminophen-not anti-inflammatory, not a NSAID. Mechanism of action: Analgesic & antipyretic. Very weak inhibitor of cyclcooxygenase. Effectively inhibits COX in the BRAIN, but not at sites of inflammation. Toxicity: SERIOUS hepatic injury w/ large doses. Analgesic abuse nephropathy. Anti-inflammatory steroids- Glucocorticoids Mechanism of action- Target multiple mediators. We want to minimize drug Action on the mineralcorticoid receptor. In response to ACTH adrenal cortex synthesizestwo classes: corticosteroids & androgens. Corticosteroids have glucocorticoid (carb metabolism regulating) activity (& immune systemfamilies are regulated) & mineralcorticoid (electrolyte balance regulating) activity. Given orally, parenterally, & topically. Major Classes of Immunosuppressive Drugs: -Glucocorticoids – anti-inflammatory steroids -Calcineurin Inhibitors -Antiproliferative/antimetabolic drugs -Antibodies. Primary uses: -Autoimmune dx -Transplantation -Hemolytic anemia of the newborn Activity Prototype Compound Sodium Retention Liver Glycogen Deposition AntiInflammatory Mineralocorticoids Glucocorticoids Aldosterone Cortisol + - + + Inhaled glucocorticoids- enhanced uptake & prolonged tissue binding in airway w/ nearly CRH=corticotrophin releasing complete hepatic first pass inactivation. hormone Steroid GR complex also interacts w/ transcription factors such as NF-kB & AP-1 to repress gene expression. Numerous effects on the immune system: -cell movt: neutrophils (↑, yet blockage into inflammatory sites), lymphocytes (↓- moved to spleen, LNs, BM), monocytes & eosinophils (↓ peripheral blood). -synthesis &/or release of inflammatory mediators: ↓ expression of COX 2, inhibits AA from phospholipids ↓ing PG & leukotriene formation, inhibits degranulation of mast cells & basophils, & inhibits synthesis & release of TNF, IL 1, IL 2 & IFN. UNDERLYING CAUSE OF THE DX REMAINS, W/ SYSTEMIC ADMINSTRATION, SIDE EFFECTS ARE COMMON & CAN BE LIFE-THREATENING. Also lowers resistance to microbial & fungal infections. Numerous uses in NONENDOCRIN DXs: arthritis, renal dxs, systemic lupus, bronchial asthma, eczema, malignancies, etc. Elimination/metabolism: In general, metabolized in liver & excreted by kidney. Receptors: steroid receptors- time lag Toxicity: prolongation of th ↑es the incidence of potentially lethal effects. There is also risk of adrenal insufficiency w/ abrupt cessation of prolonged, high-dose thfever, myalgia, arthralgia, malaise, & death w/ hypotension & shock. Primarily assoctd w/ SYSTEMIC ADMINISTRATION & large doses ↑ED SUSCEPTIBILITY TO INFECTIONIMMUNOSUPPRESSIVE, peptic ulceration, bxal disturbances, cataracts, osteoporosis & vertebral compression fractures, & inhibition of growth. Cortisol/Hydrocortisone- main glucocorticoid in humans. Mechanism of action- endogenous. T ½= 8-12 hrs. Betamethasone Mechanism of action- synthetic, good anti-inflammatory. T ½= 36-72 hrs. Dexamethasone Mechanism of action- synthetic, good anti-inflammatory. T ½= 36-72 hrs. Methylprednisolone Mechanism of action- synthetic, okay anti-inflammatory. T ½= 12-36 hrs. Prednisone Mechanism of action- Synthetic, okay anti-inflammatory. T ½= 12-36 hrs Drug of choice for autoimmune dxs (ITP), autoimmune hemolytic anemia, & acute glomerulonephritis. Also used for “autoreactive” tissue dxs & renal, heart, liver, & BM transplantation. Immunosuppressive drugs Mechanism of action- Target multiple mediators. Dampen the immune response (primary more so than secondary) in organ transplantation, autoimmune dx, & hypersensitivity. The immune response is more likely to be inhibited if th is begun before exposures to immunogen. Limitations include ↑ed risk for infections & lymphomas/malignancies. Calcineurin Inhibitors: two drugs that stop T-cell activation Cyclosporine Mechanism of action- used in “autoreactive” tissue dxs. Also used in long term th for renal, heart, liver, & BM transplantation. Binds to cytoplasmic receptor protein called cyclophilin, resulting in the inhibition of calcineurin activity. This blocks the dephosphorylation events critical for cytokine gene expression & T cell activation. Metabolism/Elimination: Metabolized in the liver. Toxicity: potl for numerous drug interactions. RENAL TOXICITY, which must be distinguished from GRAFT REJECTION IN KIDNEY TRANSPLANTATION. In as many as 75% of patients txd w/ cyclosporine. Tacrolimus (FK506) Mechanism of action- Used in renal, heart, liver, & BM transplantation. Binds to cytoplasmic receptor protein called FKBP, resulting in inhibition of calcineurin activity. This blocks the dephosphorylation events critical for cytokine gene expression & T cell activation. 100X MORE POTENT THAN CYCLOSPORINE. Toxicity: ~ to cyclosporine w/ nephrotoxicity. Muromonab CD3 Anti IL-2 abs T cell w/ TCR. ↓ Antiproliferative/Antimetabolic Drugs: prevent the clonal expansion of both B & T lymphocytes Sirolimus (also known as rapamycin) Mechanism of action- Used in combination th for renal, heart, liver, & BM transplant rejection. Binds to FKBO to inhibit a key enzyme in cell cycle progression (mammalian kinase target of rapamycin, mTOR), blocking cell cycle progression from G1 to S phase. Toxicity: Dose dpdt ↑ in cholesterol & triglycerides. NEPHROTOXICITY in combination w/ CYCLOSPORINE. ↑ed risk of LYMPHOMAS & INFECTIONS. A substrate for cytochrome CYP3A4 w/ potl for DRUG INTERACTIONS. Mycophenolate mofetil Mechanism of action- Used in organ transplantation. A metabolite that is an inhibitor of inosine monophosphate dehydrogenase (IMPDH), an impt enzyme in the de novo pathway of guanine nucleotide synthesis. B & T CELLS ARE HIGHLY DEPDT on this pathway for cell proliferation, while other cell types can use salvage pathways. Toxicity- Hematologic & GI. LEUKOPENIA, DIARRHEA, & VOMITING. A RELATIONSHIP EXSISTS BTWN IMMUNOSUPPRESSIVE TH & CANCER CHEMOTHERAPY. For cancer drugs are administered in high dose pulses. Anti-thymocyte globulin (ATG) Mechanism of action- Purified Igs prepared commercially from hyperimmune serum of animals following immunization w/ human thymocytes. The Ig binds to the thymocytes in circulation, resulting in LYMPHOPENIA & impaired T cell immune responses. Toxicity- when Ig is recognized as foreign resulting in serum sickness & nephritis. Anaphylaxis is rare. Muromonab-CD3 Mechanism of action- Used to prevent acute rejection of kidney, liver & heart transplants. A mouse monoclonal ab that binds to the ε chain of CD3 glycoprotein that is part of the TCR complex on T lymphocytes. When this happens, the TCR complex is internalized preventing further ag recognition. Initial interactions leads to cytokine release by activating T cells (CYTOKINE RELEASE SYNDROMEmild flu-like illness to lifethreatening shock). Administration of glucocorticoids prior reduces symptoms.) Toxicity: repeated use can cause immune response. Newer drug that lacks Fc portion is being devpd to prevent cross-linking & cytokine release syndrome. Daclizumab & Basiliximab Mechanism of action- Renal & heart transplantation. ANTI-IL-2 RECEPTOR ABS, “humanized” in part. Bind to the IL-2 receptor present on activated, but not resting, T cells & block IL-2 mediated T cell activation events. Toxicity: No cytokine release syndrome. Lower incidence of lymphoproliferative dxs & opportunistic infections than many other immunosuppressive drugs. Anaphylactic rxns can occur. Site of Action of Selected Immunosuppressive Agents on T Cell Activation DRUG SITE OF ACTION Glucocorticoids Glucocorticoid response elements in DNA (regulate gene transcription) Muromonab-CD3 T-cell receptor complex (blocks antigen recognition) Cyclosporine Calcineurin (inhibits phosphatase activity) Tacrolimus Calcineurin (inhibits phosphatase activity) Mycophenolate Mofetil Inosine monophosphate dehydrogenase (inhibits activity) Daclizumab, Basiliximab Sirolimus IL-2 receptor (block IL-2-mediated T-cell activation) Protein kinase involved in cell-cycle progression (mTOR) (inhibits activity) MEDIATORS: 1.Synthesis Know the pathway for synthesis including the important enzymes and the primary site of synthesis. 2.Degradation Know how the mediator is inactivated, whether by enzymes or unstable chemical structure, as well as where the degradation occurs. 3.Biological Activities Know the important biological activities of the mediator as they relate to inflammation. 4.Receptors Know which receptor the mediator activates to result in the biological activity. DRUGS: 1. Generic name of the drugs in the drug class i.e. diphenhydramine is a H1 antihistamine 2. Mechanism of action Learn the general mechanism of action of the drug class and be able to associate a certain drug with the drug class 3. Distribution - how it may affect the use of the drug i.e. non-sedating antihistamines do not cross the blood brain barrier and thus are not as likely to cause sedation 4. Elimination - how it dictates the use of the drug 5. Toxicity - major toxicities which limit the usefulness of each drug class Example: Systemic use of the anti-inflammatory steroids is limited by major side effects such as increased susceptibility to infection and osteoporosis. 6. Identify differences between individual drugs in each class or unique pharmacological properties of particular drugs in a class. Example: Indomethacin is the most potent NSAID and can cause severe frontal headache.

![Shark Electrosense: physiology and circuit model []](http://s2.studylib.net/store/data/005306781_1-34d5e86294a52e9275a69716495e2e51-300x300.png)