KCEMS EXPOSURE WORKSHEET (E)
advertisement

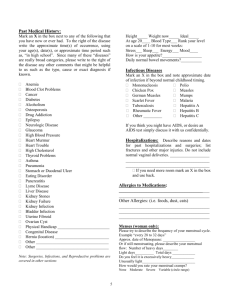
KCEMS EXPOSURE WORKSHEET This form and any information entered into this form, is the property of Kent County EMS, Inc. and are considered privileged and confidential Quality Improvement information. This information may not be shared or disclosed without the express consent of KCEMS, Inc. Patient information contained on this form is also subject to HIPPA protections. This form is to be used as an initial exposure management data collection tool and must be included as a supplement with DCH-1179 or DCH1169 forms. Source patient information is not permitted on the DCH forms under statute. 1. Name of individual with a potential exposure 2. Agency of the potentially exposed individual 3. Exposure Date 4. 5. Where is the exposed person now?* 6. Source Patient Name PM 7. Age: 8. D.O.B Exposure Time : AM Yrs 9. Where is the patient now? Mon 10. Location where exposure occurred (or report number of call) 11. Who called in the exposure report? 12. Callback # 13. Alternate callback # 14. Name of Infection Control Liaison (ICL) receiving the report of the exposure (ambulance supervisor or GRFD supervisor) 15. Agency of ICL 16. Contact # of ICL 17. Name of charge nurse at hospital 18. Primary # 19. Secondary # Tell the caller that the appropriate exposure form* must be completed by the exposed provider and must be faxed to the ICL – provide your fax number. Forms are available online at www.kcems.org/forms . 20. Exposure Information – check those that apply Source Substance Skin Contact Blood Saliva Vomit Urine Feces Semen Vaginal secretions Amniotic fluid Cerebrospinal fluid Other Intact Non-intact N/A Needle stick Membrane Yes No Does the source patient have Eye(s) Nose Mouth N/A HIV/AIDS Hepatitis B (HBV) Hepatitis C (HCV) Unknown Has the exposed individual received HBV Vaccinations? Yes No Unknown 21. Summary of potential exposure: 20. Exposed person reported to own agency supervisor : AM PM 24. ICL reported to hospital or Public Health : AM PM 21. Agency Supervisor reported to Ambulance Dispatch : AM PM 25. Exposure forms received from exposed to ICL : AM PM 22. Dispatch notified Infection Control Liaison (Sup) : AM PM 26. Forms reviewed and sent to hospital (including this) : AM PM 23. Infection Control Liaison (Supervisor) contacted person reporting exposure : AM PM 27. Test Results received by initial agency supervisor from hospital : AM PM Notes: * If the source went to the jail, this falls under Public Act 57 and DCH-1169 form should be used (see www.kcems.org/forms). If the source went to the hospital, morgue, or funeral home, or was not transported, this falls under Public Act 419 and DCH-1179 form should be used. Determination of Exposure and Follow-up The individual must have come into contact with the blood or other potentially infectious material (OPIM) from a source patient. An exposure can be defined as a percutaneous injury (e.g., needlestick or cut with a sharp object) or contact of mucous membrane or nonintact skin (e.g., exposed skin that is chapped, abraded, or with dermatitis) with blood, saliva, tissue, or other body fluids that are potentially infectious. When evaluating occupational exposures to fluids that might contain hepatitis B virus (HBV), hepatitis C virus (HCV), or human immunodeficiency virus (HIV), health care workers should consider that all blood and other potentially infectious materials as infectious. OPIM includes: (A) Semen, (B) Vaginal secretions, (C) Amniotic fluid, (D) Cerebrospinal fluid, (E) Peritoneal fluid, (F) Pleural fluid, (G) Pericardial fluid, (H) Synovial fluid, (I) Saliva in dental procedures, (J) Any body fluid that is visibly contaminated with blood, (K) All body fluids in situations where it is difficult or impossible to differentiate between body fluids. Note that sweat, urine and saliva are not included unless they have visible blood in them. Examples of things not considered to be exposures: 1. Individual gets bit by a source patient and the bite breaks the skin. Unless the biter had blood in his/her mouth, this is not considered to be an exposure to the person being bit. 2. If blood or OPIM splatters on intact skin, there is no exposure. 3. Spit in the eyes and mouth is not considered to be an exposure unless there is blood in the saliva. If the person spitting was involved in an altercation and was bleeding from the mouth and then spit into a person’s mouth, nose or eyes it would be an exposure. 4. During the delivery of a baby, if the amniotic fluid gets onto a person’s hands and there are no penetrations through the skin, then an exposure did not occur. However, if the person getting amniotic fluid on them had bleeding hangnails, dermatitis or cuts/abrasions to their skin, it would be considered to be an exposure. 5. A foley bag which breaks open dumping urine onto your pants/legs, etc. would not be an exposure unless there was blood in the urine and there was non-intact skin exposed. The statues which regulate when source patients may be tested are fairly broad and instruct the receiver of an exposure report to assume it is valid unless it obviously is not an exposure. Testing is expensive so those reports which are obviously not exposures should not be tested. The purpose of evaluating a reported exposure is to first determine if an exposure occurred. Many times healthcare workers are not certain what constitutes an exposure. If it is reasonable to believe that an exposure did occur, based on the description of the incident, the next step is to facilitate having the source patient tested. This will provide test results for HBV, HCV and HIV. If any of these are found to be positive, the exposed person must consult with a healthcare worker trained in evaluating the risk of the exposure, the nature of the infectious material and then making a determination as to the need to provide post exposure prophylaxis. As the infection Control Liaison, our job is to rule out obvious non-exposures then help facilitate source testing and promote follow-up when infectious materials are present. Our job is not to determine if post exposure prophylaxis is indicated, nor is it to provide the exposed individual with test results of the source patient. We merely confirm that the incident is or is not an exposure, help them complete the proper paperwork, ensure that the source is tested, ensure documentation gets to where it needs to be and then provide a link from the hospital person who will receive test results with the supervisor of the exposed person. We also can help to provide some direction to the supervisor of the exposed person. Since we ultimately don’t get test results, it is best to have the person call you back immediately after getting the results from the hospital so you can help them with the next steps. If all tests are negative, they should be instructed to let the exposed person know the results and to complete any required MiOSHA recordkeeping forms (see www.michigan.gov/mioshastandards part 554 – Bloodborne Infectious Diseases and R 408.22101 et seq., being Part 11. Recording and Reporting of Occupational Injuries and Illnesses). If any of the tests are positive (an infectious material was detected), the exposed person should be sent to Occupational Medicine for a work related injury/exposure. The individual should report the exposure to Occupational Medicine and provide copies of incident reports, DCH forms, Exposure worksheets, etc. Occupational Medicine staff will assist with getting copies of the source test results and will consult with the patient on the need for post exposure prophylaxis. Thus, the supervisor should be directed to get the person to Occ. Med. Once completed, the documentation should be saved in a secure location. A copy of the Exposure worksheet and the DCH form should be sent to KCEMS via email to dobiden@kcems.org; the email should be titled “CONFIDENTIAL PSRO – EXPOSURE”. Frequently, healthcare workers worried about exposures inquire about risk related to their potential exposure. This was taken from the CDC site for bloodborne exposures What is the risk of infection after an occupational exposure? Hepatitis B Virus (HBV) Health care workers who have received hepatitis B vaccine and have developed immunity to the virus are at virtually no risk for infection. For an unvaccinated person, the risk from a single needlestick or a cut exposure to HBV-infected blood ranges from 6%–30% and depends on the hepatitis B e antigen (HBeAg) status of the source individual. Individuals who are both hepatitis B surface antigen (HBsAg) positive and HBeAg positive have more virus in their blood and are more likely to transmit HBV. Hepatitis C Virus (HCV) Based on limited studies, the estimated risk for infection after a needlestick or cut exposure to HCV-infected blood is approximately 1.8%. The risk following a blood splash is unknown but is believed to be very small; however, HCV infection from such an exposure has been reported. Human Immunodeficiency Virus (HIV) The average risk for HIV infection after a needlestick or cut exposure to HlV-infected blood is 0.3% (about 1 in 300). Stated another way, 99.7% of needlestick/cut exposures to HIV-contaminated blood do not lead to infection. The risk after exposure of the eye, nose, or mouth to HIV-infected blood is estimated to be, on average, 0.1% (1 in 1,000). The risk after exposure of the skin to HlV-infected blood is estimated to be less than 0.1%. A small amount of blood on intact skin probably poses no risk at all. There have been no documented cases of HIV transmission due to an exposure involving a small amount of blood on intact skin (a few drops of blood on skin for a short period of time). The risk may be higher if the skin is damaged (for example, by a recent cut), if the contact involves a large area of skin, or if the contact is prolonged.