[B] E1 Lec 12 Imaging of the KUB
advertisement
![[B] E1 Lec 12 Imaging of the KUB](http://s3.studylib.net/store/data/006896100_1-2240a5b8d7cc3e4dfeaeb035ef096125-768x994.png)
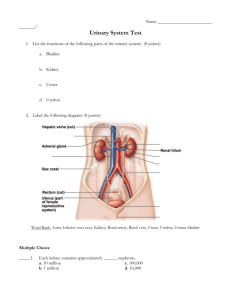
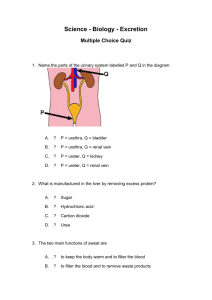
OS 214 [B]: Digestion and Excretion 1 Lec 12: Imaging of the KUB December 5, 2013 Dr. Rosanna Fragante TOPIC OUTLINE I. Introduction to KUB Imaging A. KUB X-ray film B. Intravenous Pyelography C. Ultrasound D. CT Scan II. Renal Anatomical Abnormalities A. Ptotic kidney B. Horseshoe Kidney, Pelvic Kidney C. Vesico-ureteral Reflux III. Infections A. Acute Pyelonephritis B. Chronic Pyelonephritis C. Renal Abscess D. Renal Tuberculosis IV. Calculi and Obstructive Uropathy A. Stones and Calculi B. Hydronephrosis C. Ureteral Stricture V. Renal Parenchymal Diseases A. Acute Renal Parenchymal Disease B. Masses/Tumors and Cysts VI. Urinary Bladder A. Cystolithiasis B. Prostatic Enlargement withChronic Bladder Obstruction/Cystitis C. Emphysematous Cystitis D. Chronic Cystitis E. Contracted Bladder F. Post-traumatic Bladder Extrophy G. UB Malignancy VII. Adrenal Glands A. Adrenal Gland Hyperplasia B. Pheochromocytoma VIII. Renal Vascular Lesions Renal Artery Stenosis Advise the patient to have empty bowel (e.g. take Dulcolax first) to visualize the outlines of the kidneys and the psoas Legends: From the Powerpoint presentation From the lecturer and other sources (textbook, Internet, etc.) Note: Dra Fragante said that she will use the same pics in the exam. I. INTRODUCTION TO KUB IMAGING Before using imaging modalities, make sure to perform a good history and physical examination (PE) first, as these will give you a working impression and guide you in choosing the appropriate modalities. The different modalities used for visualizing the KUB are: o X-ray film o Intravenous pyelography (IVP) o Ultrasound (UTZ) o Computerized Tomography (CT) Scan o Magnetic Resonance Imaging (MRI) History Taking o Working Impression o Renal Function: Serum BUN and Creatinine results (to make sure that the kidney can fully excrete the iodinated contrast medium) o History of Allergies (in case patient is allergic to contrast like iodine; may lead to anaphylactic shock) o Take note also of comorbidities, e.g. diabetes mellitus, hypertension Review on the anatomy of the kidney o The rectum, uterus, and vagina all had the same origin, with one opening, the cloaca o The superior pole of the kidney is oriented medially, while the lower pole is oriented outward/laterally o The kidney is a retroperitoneal organ located in the paravertebral area o The bladder, however, is extraperitoneally located. That is why if ever there is a leakage of urine, it does not mix with the intraabdominal space and organs “(sometimes may go unnoticed by patients) o Flow of urine: tubulescalycesureter o The renal artery enters beside the medullary pyramids and form the arcuate vessels Figure 1. Review of the Anatomy of the Kidney. The upper pole is medially oriented while the lower pole is laterally oriented. The glomeruli are found in the cortex, while the collecting tubules are found in the medulla. A. KUB (KIDNEY, URETER, BLADDER) X-RAY FILM KUB X-ray is a plain film evaluation of the abdominal area Lorvin, Roms, Deni Figure 2. Normal KUB Film showing the psoas lines and the outlines of the kidneys. Psoas lines are fat planes that outline the psoas muscles. Fat is black, bone is white. Note that the right kidney (RK) is normally lower than the left because of the liver. B. INTRAVENOUS PYELOGRAPHY Series of films with contrast material to better visualize the urinary system To see if there is retention of urine REQUIREMENTS FOR IVP Evaluate renal function o Get the serum BUN and creatinine to be assured that the contrast material will be excreted History Taking: o Diabetes, HPN o Inquire about the allergy history of the patient to foresee allergic reactions to the contrast material that will be used o To know what to look for in IVP CONTRASTS Ionic- hyperallergenic and hyperosmolar (may cause pain); gives a burning feeling when given intravenously; more affordable (Php 300 in PGH) Non-ionic- hypoallergenic with low osmolarity; more expensive (Php 1500) IVP PROCEDURE Scout film→inject contrast→film 3 minutes after contrast→film again after 10 minutes→during full bladder→post-void Can be used to assess kidney function Figure 3. IV Pyelogram Longer, more complete IVP Procedure: 1. Plain film/Scout film o Calcific densities→stones o Used as reference figure Page 1 / 9 Lec 12: Imaging of the KUB 2. Inject contrast material 3. Film at 3 minutes o Kidney and upper collecting systems visualized o The contrast in the cortex and the medulla is seen 4. Film at 5 minutes o Visualize pelvis (collecting system and ireters are opacifying) 5. Contrast at 10 minutes o Contrast has reached the pelvocalyceal system, ureters o This is the time to look for stones ion these areas o If you drink water, you expect to feel full at 10 minutes 6. Film at 15 minutes o Whole abdomen profile o Kidneys are still evaluated o Bladder is starting to fill 7. Full bladder film at 20 minutes o Full bladder has very smooth borders o “dapat bilog na” 8. Post-void film o To check urinary retention o <50 cc o You can still see some degree of contrast in the various areas of the GU system C. ULTRASOUND Trivia: The ultrasound originated from sonar waves in the ocean emitted by submarines The image is produced through sonar waves that bounce back Generally available, non-invasive, inexpensive Used to see the kidney morphology (oval configuration) You place the probe on top or at the back of the patient OS 214 Figure 5. Ptotic right kidney- notice that it is almost completely at the level of the pelvis. B. HORSESHOE KIDNEY, PELVIC KIDNEY Congenital malrotation/ Ectopia Horseshoe kidney- lower poles of the kidneys are medially connected with an isthmus→malrotation of kidneys The central portions are fused and medially rotated, leading to poor drainage o Patients with this are prone to infections, stones, and malignancies so take care of patient’s risk factors o Horseshoe kidney is medially located Pelvic kidney- at the level of the pelvis. Left kidney failed to go up, and right kidney is displaced upward (not only upon standing);prone to UTI because the path is shorter Pregnancy (an enlarging uterus) may be problematic: prone to hydronephrosis and can make labor very difficult o In pregnancy, there is extrinsic compression of the ureter, making the female more prone to infection o Other symptoms are bedwetting and recurrent UTI Figure 4. Sagittal (left) and transverse (right) views of the kidney through ultrasonography. The outer hypoechoic area denotes the renal parenchyma, while the inner hyperechoic area denotes the renal pelvis (collecting system) – white fatty area. D. CT SCAN A CT Scan emits high energy beams of X-ray that image the whole abdomen Has more detail than the other modalities, but more expensive Patient is scanned in the supine or decubitus position. Occasionally, a prone position may prove useful The best images are obtained with the patient’s respiration suspended; frequently, the end of partial or full inspiration brings the kidney to better view Allows us to see cortex, medulla, and renal drainage also the vascular structures Able to see axial or coronal sections Better visualization of kidney and adjacent structures II. ANATOMICAL ABNORMALITIES A. PTOTIC KIDNEYS Kidney is descended by at least two vertebral levels during standing position; “drooping lily sign” The calyceal system is downwardly displaced Prone to having obstruction and infection Clinical presentation: when the patient goes from a supine position to an upright position, there is intermittent pain (because the kidneys descend) “Kapag nakahiga po ako, ok lang po. Kapag tumatayo po ako, sumasakit po likod ko.” Because the ptotic kidney falls down=intermittent pain Mostly asymptomatic. If symptomatic, surgery is needed to attach it upward It can also lead to stenosis or bleeding at the level of the ureteropelvic junction Lorvin, Roms, Deni Figure 6. Horseshoe Kidney (left) and Pelvic/Ectopic Kidney (right) C. VESICO-URETERAL REFLUX Urine goes back to the kidneys (renal pelvis); patients are prone to pyelonephritis (if there are bacteria in the bladder) One of the most common causes of infections in the kidneys Early detection is the key- prevent chronic pyelonephritis (from infected urine) Reflux increases risk for infection, recurrent infection leads to scarring Results in dilatation of the collecting system when hydronephrosis is severe Common in children, causing UTI In a voiding cystourethrogram (VCUG), you put the contrast in the bladder and ask the baby to void Premature babies are prone to reflux due to the immaturity of the GU system. When the babay voids, there is upward displacement of the urine, making him/her prone to nephritis If the urine continues to go up and down, and up and down, hydronephrosis eventually occurs and this could lead to renal failure Page 2 / 9 Lec 12: Imaging of the KUB OS 214 White arrow-enlarged kidney. Enlargement of the kidney is due to edema of inflammation. Areas of avascularity are due to toxic secretions from bacteria (most common is E.coli) which cause vasoconstriction. Vasoconstriction could cause hypoperfusion in the kidney which makes it prone to infection and abscess formation. And liquefaction necrosis, and eventually, kidney dies. B. CHRONIC PYELONEPHRITIS May have cortical irregularities or scarring Atrophied kidney and cortical abnormalities. If not treated, renal abscess forms Figure 7. Vesico-ureteral Reflux. Black arrows point to the reflux (right) Note: Female GU Tract Wiping from back to front after a bowel movement may force germs into urethra Always do it from front to back III. INFECTIONS Females are more prone to infection due to close proximity of vagina, uterus, and urinary bladder to each other, A. ACUTE PYELONEPHRITIS Inflammation of the kidney Normal findings in almost all various imaging modalities (IVP), so this is difficult to diagnose using imaging modalities Can have enlargement of one kidney, hypodense on CT Scan Nuclear scan provides earlier detection “mahapding balakang” Presentation: flank pain, fever, dysuria Extra-painful if kidney-punched; Pain can be elicited even with kidney tap “jerking movement” Risk factors- e.g. stones Extrusion of contrast may not be as much because bacteria produce enzymes that may vasoconstrict (lower RBF→ lower GFR) Seen as hypodensities (poor excretion of contrast due to not much contrast reaching that area) Red cup project- spot check of urinalysis of children from grades 1-6 showed that 25% of them have undiagnosed UTI Figure 10. Cortical scarring which can be a sign of chronic pyelonephritis. Distance at poles should not differ by greater than 2mm. on the left kidney, there is thinning of the cortex. The kidneys get smaller and smaller as they are continually scarred. C. RENAL ABSCESS The only way to treat is to aspirate the renal abscess Abscess is hypodense/hypoechoic Predispoding factors: immunocompromised state, chronic steroid intake, diabetes Figure 11. Ultrasound (left ) and CT Scan (right) showing renal abscess. White arrows show fluid densities (due to pus). In UTZ, the abscess is hyperechoic. In CT Scan, it is dark. It happens when you do not treat your chronic pyelonephritis. D. RENAL TUBERCULOSIS Figure 8. KUB Film showing acute pyelonephritis. Left kidney is shown to be edematous and larger than the right. TB in the Philippines is still a problem Usually from hematogenous spread from liver and spleen leading to bacilli deposition in the kidney Potty kidney- areas of necrosis and calcifications Presents with “sterile pyuria”- pus on urinalysis, but organism can’t be isolated Patients already come when they are in the late stage of TB If you get UTI unresponsive to most antibiotics, rule out TB With renal tuberculosis, the kidney becomes one bif putty mass of pus, which eventually calcifies. There is multiple involvement of the liver and both kidneys, as seen in the photo on the CT Scan photos Figure 9. Ultrasound (left) and CT Scan (right) showing Acute Pyelonephritis (pointed by their respective arrows). Black arrow-stone. Lorvin, Roms, Deni Page 3 / 9 Lec 12: Imaging of the KUB Figure 12. KUB Film (left) and CT Scan (right) with foci of renal tuberculosis, shown by white arrows. Multiple calcific densities are seen. In the ureter, there are stones. CT scan (upper right) shows presence of multiple granuloma in the liver (possible source of genitourinary TB). OS 214 Figure 14. Staghorn calculi in both plain (left) and contrast (right) films. They can occupy a whole collecting system. They conform to the configuration of the pelvocalyceal system. IV. CALCULI AND OBSTRUCTIVE UROPATHY A. STONES AND CALCULI Stones are spiculated and cause extreme pain (stones with high calcium content are more radio-dense) Analogy of pain from stones in ureter: glass rubbed on palate Uric acid stones o intake of beans, beer, meat, oats (eating oatmeal 3x a day, since it is high in uric acid) o usually not radioopaque or radiolucent on xray (along with cystine stones) because of low calcium content Calcium stones o from salty foods ( ie. junk food), calcium tablets, mineral water with lots of minerals o very radioopaque (appears very white on xray film because it is calcified) o hard stones o hard to treat – need surgery Stones form in the calyx may be transported to the renal pelvis and then to the ureter; obstruction may lead to hydronephrosis Staghorn calculi o Stones can occupy an entire collecting system, conforming to the pelvocalyceal system; thus, the “reindeer configuration”. o Clinical presentation: “nangangalay ang balakang” o Can be detected by ultrasound and CT scan regardless of composition (calcium, uric acid etc) o Avoid calcium supplements when not menopausal yet, as it can be a predisposing factor. Drink milk instead. Figure 15. Renal Calculi as shown in UTZ. The stones are hyperechoic, with shadowing behind (below) them. Does not depend on the stone composition, whatever it is, you’ll see it on UTZ. . Black arrow on the left photo shows a stone in the proximal ureter Figure 16. CT-stonogram showing the stones. Black arrows point to stones found in the renal pelvis. This is requested when X-ray is not enough; better image quality than UTZ. Composition of the stone can also be identified using CT-stonogram. If >500 HFU (high frequency ultrasound) – Calcium stones, <500 HFU – Uric acid or cystine stone You can assign a CT number based in the appearance of the stone which can determine the type of management for the patient (cystine and uric acid stones can be melted by alkalinizing the urine while calcium stones need shockwave or surgery) Figure 13. Renal calculi, as shown by arrows (white calcified structures hence calcium stones) – hyper dense laminated calcifications Lorvin, Roms, Deni UTZ and CT – good modalities for stone detection because they are not dependent on the composition of the stone, can be easily visualized. Page 4 / 9 Lec 12: Imaging of the KUB OS 214 C. URETERAL STRICTURE An area of narrowing in the ureter Stones and inflammation are more common causes can lead to fibrosis and scarring, leading to stricture “Parang zesto straw yung normal caliber ng ureter.” But it is much less in stricture Figure 17. Ureteral stones as seen in plain and contrast films using retrograde pyelography (RPG). Notice the discontinuation of the contrast because of obstruction by the stones. If patient has flank pain – in the clinics, diagnostics: stenograph. B. HYDRONEPHROSIS “Hydro meaning water and nephrosis meaning collecting system of the kidney”; accumulation of water in the kidney Obstruction in the collecting system --> urine cannot drain down to the bladder dilatation of the collecting system Too much ballooning/dilatatonparenchyma compression thinning of (cortex) parenchyma with loss of function May be uni- or bilateral KUB/IVP: Reduced excretion of contrast, enlargement of kidneys in chronic obstruction prone to infection consequent pus formation --> Hydronephrosis Figure 18. Hydronephrosis. Left film shows an enlarged right kidney. Right film shows a right kidney with diminished cortex and dilated collecting system. Ureter PCS pus/debris Figure 19. UTZ showing hydronephrosis. Note the much-dilated pelvis, and the thinned out parenchyma. PCS – pelvocalyceal system; Ur – ureter. *black areas are fluid in the collecting system; pus and debris in ureter; becomes septicaspirate for kidneys to recover. Lorvin, Roms, Deni Figure 20. Ureteral stricture. Left ureteral stone in retrograde pyelogram; stricture at the proximal segment (narrowing), dilated pelvis (stricture or scar remains even if stone has been removed) V. RENAL PARENCHYMAL DISEASE A. ACUTE RENAL PARENCHYMAL DISEASE Patients are edematous, ascitic (with pleural effusion) because the glomeruli are unable to filter; fluid can’t be excreted. “Akala ng magulang, malusog yung anak, yun pala ascites na.” Enlarged (edematous) kidneys on UTZ Hyperechogenic ball-like kidney Most common: glomerulonephritis Figure 21. UTZ showing acute renal parenchymal disease. The areas are hyperechoic (lighter/brighter than normal) because of inflammation. B. MASSES/TUMORS AND CYSTS RENAL CYSTS Most common in adults; increase in incidence with age o Fluid-filled and can cause obstruction if large enough o Seen as “fraying of the collecting system” tubules are so dilated then they pinch off o May cause obstruction o Hard to palpate due to retroperitoneal location unless the mass is enlarged o Usually benign o A 50 year old has a 50% chance of having a renal cyst o Renal tumors may metastasize to nearby organs such as the liver and spleen; first symptom is hematuria (painless). o Do not be alarmed when you already see a cyst on UTZ. Confirm first if benign or malignant. Not alarming if less than three, small and does not cause obstruction; advise to have regular check ups WILMS TUMOR o most common in the pediatric population – akala mataba, sa isang side lang pala at may tumor na o may occupy the whole kidney; o diffused, multiple masses Page 5 / 9 Lec 12: Imaging of the KUB OS 214 o Can be palpated in the abdomen of the child so don’t forget when you rotate in the wards (but not readily palpable until its very large) RENAL CELL CARCINOMA o More common in adults o Diffuse malignancies – because of cancers like lymphomas (multiple masses) o Detected late because kidneys are retroperitoneal When palpable, it is already large! o Age >50 y/o- regular checkup is recommended Figure 25. UTZ (left) and CT scan (right) showing renal involvement in diffuse malignancies (eg. lymphomas). VI. URINARY BLADDER Normal filled UB: very smooth borders, like a balloon Normal post-void UB: not more than 50cc of urine left; if more than 50cc, then UB is more prone to infection If the urine is expelled in drops, then suspect obstruction Full bladder can accommodate 200 cc of fluid (as much as 800 cc) Bladder content of 200cc: start of urge to urinate Age >50 years old urinate more often due to lessened capacity of the bladder Problem with males with enlarged prostate glands Figure 22. Cysts, as shown in IVP (left), UTZ (upper right, has fluid beside cyst) and CT scan (lower right). Cysts in IVP are white. Figure 26. Normal filled UB (left and middle) and normal post-void UB (right). A. CYSTOLITHIASIS Figure 23. Wilms tumor or nephroblastoma in UTZ (left) and CT scan (right). Most common in the pediatric population; chance of metastasis is high, common in the lungs LM Common in the Philippines because we are near the sea (high salt diet) Stones of the Urinary Bladder; calcific, rounded/ovoid opacity that have the same density as bone and may look like eggs Usually lamellated; lamellae represent times of deposition, just like in “tree rings” progression: small stones in the UB accumulates more sediment -> lamellated large stones High salt diet, like living near the sea, can be a risk factor Capacity of UB is decreased; there may also be reflux Patient becomes more prone to cystitis Moves with changes in position Usually smooth borders but can be mulitlobulated Plain Contrast SM Figure 24. CT scan images showing renal cell carcinoma (left, with arrows) and organ metastases (LM – liver metastasis, SM – splenic metastasis). Lorvin, Roms, Deni Figure 27. Plain and contrast films showing cystolithiasis. Right image is very prone to having chronic cystitis. Page 6 / 9 Lec 12: Imaging of the KUB OS 214 D. CHRONIC CYSTITIS UB may become fibrotic Prone to vesico-ureteral reflux VU Reflux: Infected urine goes back to the kidneys (due to increased pressure in the bladder) which can lead to chronic pyelonephritis Can lead to chronic renal parenchymal disease Inflammation thicker bladder wall lumen size decreases (contracted bladder) less capacity of bladder voids often VUR Figure 28. UB calculi with blood clots, as shown in UTZ. Presents most commonly with hematuria (gross/tea colored/mildly red) and dysuria B. PROSTATIC ENLARGEMENT WITH CHRONIC BLADDER OBSTRUCTION/CYSTITIS Patients have poor stream due to retention (dribbling- with obstruction, frequent urination) If large enough, can present as abdominal mass. Rectal UTZ is used to evaluate prostate (male greater than 50 years old) Figure 31. Chronic cystitis: with vesico-ureteral reflux (VUR), as shown in contrast film (left), and with thickened bladder wall (white lining of the UB located in the center), as shown in CT scan (right). Enlarged prostate Figure 29. Enlargement of the prostate, leading to UB obstruction and cystitis. Bladder is elevated by prostate (left). Sometimes appears like a Christmas tree and may lead to formation of UB diverticulum due to high pressure, prone to infection and malignancy; Note the irregular bladder wall borders Figure 32. Normal findings in UTZ (top images), compared to findings of cystitis in UTZ (bottom images). The normal UB has smooth walls, while the cystitic UB has rough edges. C. EMPHYSEMATOUS CYSTITIS E. CONTRACTED URINARY BLADDER Characterized by infection of urinary bladder (UB) and UB wall with gas-forming organisms; thus, there is air outlining the wall of the bladder. “Like inflating a balloon” Formation of UB diverticulum prone to cystitis. “Mickey Mouse” appearance because of diverticula (thinning of the muscular wall leading to outpouching) UB Div UB capacity approximately only 20cc Inflammation thicker bladder wall lumen size decreases (contracted bladder) less capacity of bladder voids often Treated with bladder augmentation: Creating a “neobladder” or ileal conduit from an ileal segment (ileal conduit) to have larger capacity of bladder UB Div Figure 30 . Emphysematous cystitis. Note the outline of air in the UB wall (shown by arrows) and the “Mickey Mouse” appearance (UB Div – UB diverticula) Lorvin, Roms, Deni Figure 33. Contracted bladder, consequence of TB (fibrosis and scarring). Can have urine output of around 2 tbsp a day Page 7 / 9 Lec 12: Imaging of the KUB OS 214 F. POST-TRAUMATIC BLADDER DYSTROPHY UB not only descends, but goes out There is widening of the symphysis pubis even separated sometimes; also, there is bilateral dilatation of the collecting systems (including ureters) Due mostly to straddle injuries (e.g. motorcycle accidents, pelvic fractures, horseback riding) May involve urethras in males Figure 36. CT scans showing normal adrenal gland (left, appears like a sliver of tissue) and hyperplastic adrenal gland (right). B. PHEOCHROMOCYTOMA Tumors/mass of the adrenal medulla, resulting in increase in catecholamine production – may result to increase in blood pressure Hypertension is one manifestation (from catecholamine secretion) Triad: Diaphoresis, palpitations, headache Extreme case: fainting (due to hypertension) while urinating. As opposed to adrenal gland hyperplasia, pheochromocytoma look like round masses; in the former, the original shape is somewhat retained Figure 34. Bladder extrophy. The ureters are dilated, and the symphysis pubis widened. G. UB MALIGNANCY There is a change from “full moon” to “half/crescent moon” UB wall may be eaten up by tumors Risk factors: chronic infection, smoking and alcohol intake, also those exposed to chemicals from working in factories, drug abuse, those who handle chemotherapeutic agents Most common history finding: gross hematuria ( urine is like iced tea or orange juice), infection, working with chemicals, illegal drug usage Most common histopathologic type: transitional cell CA (multicentric) Figure 37. Pheochromocytoma, as seen in UTZ (left) and CT scans (right) VIII. RENAL VASCULAR LESIONS Renal angiography – used for visualizing the vascular tree of the kidneys; aside from locating lesions, this is also used in screening for organ transplants In angiography, sometimes you can see many renal arteries (our professor has seen 8 renal arteries!) Philippines has one of the highest rates of kidney transplantations (up to 4 or 5 transplants a day!) Figure 35. UB malignancy as shown in CT scan (left) and contrast film (right), where the “crescent moon” is very evident. VII. ADRENAL GLANDS Normal Thickness 5-6mm to 10mm Very important cause it produces catecholamines and corticosteroids Modalities of choice: CT or MRI because of the relative small size of the adrenals A. ADRENAL GLAND HYPERPLASIA Can produce excess ACTH, causing increased blood pressure. The contralateral gland undergoes atrophy because of negative feedback. (Inc glucocorticoid production from hyperplastic adrenals, decreased ACTH, atrophy of contralateral gland due to loss of function) Lorvin, Roms, Deni Figure 38. Normal renal angiogram Page 8 / 9 Lec 12: Imaging of the KUB OS 214 A. RENAL ARTERY STENOSIS Renin-Angiotensin pathway is the cause of hypertension in patients with Renal Artery Stenosis The RAAS compensates for low renal blood flow thus retaining more fluids and causes the hypertension Before Stenting After Stenting Figure 39. The left angiogram shows renal artery stenosis, while the right angiogram shows results after stenting END OF TRANSCRIPTION Greetings! Lorvin: Merry Christmas and a Happy New Year! Roms: Hi!! Deni: AFTG! Lorvin, Roms, Deni Page 9 / 9