Yes ____ No ____ When
advertisement

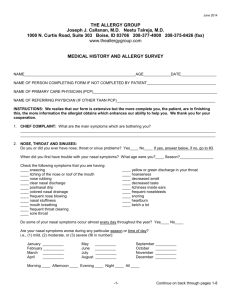
THE ALLERGY GROUP Joseph J. Callanan, M.D. Neetu Talreja, M.D. 1000 N. Curtis Road, Suite 303 Boise, ID 83706 208-377-4000 208-375-8426 (fax) www.theallergygroup.com MEDICAL HISTORY AND ALLERGY SURVEY NAME_____________________________________________________AGE_____________DATE_________________ NAME OF PERSON COMPLETING FORM IF NOT COMPLETED BY PATIENT_________________________________ NAME OF PRIMARY CARE PHYSICIAN (PCP)___________________________________________________________ NAME OF REFERRING PHYSICIAN (IF OTHER THAN PCP)_______________________________________________ INSTRUCTIONS: YOU MUST COMPLETE THIS FORM. OUR INSURANCE REQUIRES THAT IT BE DONE. YOU WILL NOT BE SEEN UNLESS IT IS COMPLETED. THERE ARE 7 PAGES. PLEASE COMPLETE ALL PAGES. 1. CHIEF COMPLAINT: What are the main symptoms which are bothering you? _____________________________________________________________________________________________ _____________________________________________________________________________________________ 2. NOSE, THROAT AND SINUSES: Do you or did you ever have nose, throat or sinus problems? Yes____ No____ If yes, answer below, if no, go to #3. When did you first have trouble with your nasal symptoms? What age were you?____ Season?________________ Check the following symptoms that you are having: ____ sneezing ____ hoarseness ____ itching of the nose or roof of the mouth ____ decreased smell ____ nose rubbing ____ decreased taste ____ clear nasal discharge ____ itchiness inside ears ____ postnasal drip ____ nose bleeding ____ colored nasal drainage ____ snore ____ frequent nose blowing ____ sore throat in the morning ____ nasal stuffiness ____ you clear your throat often ____ mouth breathing ____ heartburn ____ frequent throat clearing ____ wake up with heartburn ____ sore throat ____ belch a lot ____ yellow or green discharge in your throat Do some of your nasal symptoms occur almost every day throughout the year? Yes____ No____ Are your nasal symptoms worse during any particular season or time of day? i.e., (1) mild, (2) moderate, or (3) severe (fill in number): January __________ February __________ March __________ April __________ May June July August __________ __________ __________ __________ September __________ October __________ November __________ December __________ Morning ____ Afternoon ____ Evening ____ Night ____ All ____ -1- Continue on back through pages 1-7 Have you ever had any of the following problems? (Check) Yes ____ No ____ sinus infection Yes ____ No ____ nasal polyps Yes ____ No ____ temporomandibular joint disease (TMJ) Yes ____ No ____ frequent headaches – Where? front ____ temples ____ eyes ____ back ____ If yes, do you frequently chew gum? Yes ____ No ____ Have you had braces? Yes ____ No ____ Yes ____ No ____ aspirin-induced nasal symptoms Yes ____ No ____ nasal surgery – When? ____________________ Last? ____________________ Yes ____ No ____ frequent “bad colds” Yes ____ No ____ frequent tonsillitis – How many times per year? ____________________________ Check one of the following statements that best describes the severity of your nasal symptoms when they are at their worst? ____ mild ____ severe ____ moderate ____ very severe How many school or work days have you missed in a year’s time due to these problems? _____________________________________________________________________________________________ What medicines have you taken to control your eye and/or nose symptoms? _____________________________________________________________________________________________ Are you taking any of these medicines every day? _____________________________________________________ Generally, how much relief from your symptoms do you get by taking these medicines? ____ Excellent ____ Good ____ Moderate ____ Very little ____ None What nose drops or sprays are you using? ___________________________________________________________ Have you had a CT scan of your sinuses? Yes ____ No ____ When ______________________________________ 3. EARS: Have you ever had any of the following ear symptoms? (Check) Yes ____ No ____ If no, go to #4. Yes ____ No ____ frequent ear infections Yes ____ No ____ are you dizzy? How many within the past year? ____ Yes ____ No ____ are you lightheaded? Yes ____ No ____ is your hearing impaired? 4. EYES: Have you had any of the following eye symptoms? (Check) Yes ____ No ____ If no, go to #5. Yes ____ No ____ itching Yes ____ No ____ light hurts your eyes Yes ____ No ____ redness Yes ____ No ____ yellow discharge from eyes Yes ____ No ____ tearing Yes ____ No ____ eyelid swelling Yes ____ No ____ dryness Yes ____ No ____ eyelid irritation Yes ____ No ____ burning How often have these symptoms been a problem within the past year? Circle correct answer: never; some; a lot; extreme. 5. LUNGS: If you do or have had asthma, please answer the questions. If you have never had wheezing or lung problems, you may skip this question and proceed to #6. When did you first begin to have wheezing spells? Age? ____ Season? __________ Check the following symptoms you are having: Yes ____ No ____ mild to moderate wheezing episodes Yes ____ No ____ severe wheezing episodes Yes ____ No ____ does this limit your exercise or play? Yes ____ No ____ during or after exercise? -2- Continue on back through pages 1-7 Is your wheezing worse during any particular months or time of day? (Mark yes or no) January __________ February __________ March __________ April __________ May __________ June __________ July __________ August __________ September __________ October __________ November __________ December __________ Morning ____ Afternoon ____ Evening ____ Night ____ With your wheezing do you usually have: ____ fever ____ cough ____ tightness in your chest? Do you usually have a cold or chest infections when you wheeze? ______________________________________________________________________________________________ Can you have a normal “bad cold” without you then developing chest congestion and wheezing? _________________ How many times during the past year have you had to visit your doctor (or hospital emergency room) because of your wheezing? _____________________________________________________________________________________ How many times have you been hospitalized due to wheezing?___________________________________________ When were you last in the hospital for this?___________________________________________________________ How many school or work days have you missed this year due to your wheezing? ______________________________________________________________________________________________ What medicines are you taking to control your wheezing? _______________________________________________ ______________________________________________________________________________________________ Do you use inhaler(s)? ____ How often? ____________________________________________________________ Which one(s)? __________________________________________________________________________________ Have you required cortisone (prednisone, Medrol, etc.) drugs for control of your wheezing in the past? Yes ____ No ____ How many times? ____ Date last used: ____________________ Do you ever have any of the following symptoms? (Check) Yes ____ No ____ frequent coughing spells Yes ____ No ____ coughing on exertion Yes ____ No ____ recurrent night cough Yes ____ No ____ coughing then wheezing Yes ____ No ____ coughing up mucus (color? __________) Yes ____ No ____ coughing with laughing Yes ____ No ____ shortness of breath with exercise Yes ____ No ____ coughing with lying down Yes ____ No ____ blood in mucus Yes ____ No ____ coughing with talking on the phone 6. CHEST INFECTIONS: As an infant or child, did you have asthma? Yes ____ No ____ X-rays: Have you had a chest x-ray within 5 years? Yes ____ No ____ If so: Date of last chest film _______________ Where x-ray obtained _______________ 7. ALLERGIC SKIN PROBLEMS: Have you ever had eczema? Yes ____ No ____ If no, go to #8. When last? ____________________________________________________________________________________ What parts of your skin were affected? Arms ____ Legs ____ Face ____ Body ____ 8. PREVIOUS ALLERGY EVALUATIONS: Have you ever had an allergy evaluation in the past? Yes ____ No ____ If no, go to #9. If you have, then complete the following questions: What age were you when you had your first allergy evaluation? __________________________________________ Which doctor and where? ________________________________________________________________________ If you have had skin testing, to what were you found to be allergic? ____ trees ____ weeds ____ dust ____ grasses ____ molds ____ feathers ____ foods _____________________________ ____ others ____________________________ If you have received a series of allergy shots in the past, please give the inclusive dates: _____________________________________________________________________________________________ -3- Continue on back through pages 1-7 If you are on allergy shots now, how often are you taking them? What improvement have you (did you) note(d) in your symptoms while on allergy shots: ____ marked improvement (almost complete clearing of your symptoms) ____ moderate improvement ____ no improvement Did you ever have an allergic reaction to your shots? Yes ____ No ____ If yes, what happened? __________________________________________________________________________ _____________________________________________________________________________________________ _____________________________________________________________________________________________ 9. FACTORS WHICH MAY CONTRIBUTE TO YOUR ALLERGIC PROBLEMS: In the following questions, 1-7, check the factors that you think will make your nose symptoms or wheezing (asthma) start or become worse. Otherwise go to #10. (1) Lungs ______ ______ (2) ______ ______ ______ ______ (3) ______ ______ ______ (4) ______ ______ (5) ______ ______ ______ (6) ______ ______ ______ ______ ______ (7) ______ ______ ______ ______ ______ Infections a “viral bad cold” a respiratory infection Weather change in weather wet, rainy weather onset of cold weather being in the wind Inhalant Allergens playing in or mowing the grass musty smells exposure to house dust Hormone menstruation pregnancy Physical Factors air conditioning cold air getting up in the morning Smells exhausts, fumes smoke perfumes, cosmetics cleaning agents cooking odors Miscellaneous birds cats dogs other animals feather pillows Nasal ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ ______ 10. INGESTANTS: Do you know of any foods, drinks, or medicines that will make your nose symptoms or wheezing start or cause it to become worse? (Circle and add items). Yes ____ No ____ If no, go to #11. Foods (milk, egg, wheat, nuts, peanut, shellfish, soybean) _______________________________________________ Drinks (beer, wine) ______________________________________________________________________________ Medicines (aspirin) ______________________________________________________________________________ 11. DRUG ALLERGY: Have you ever had an allergic reaction to any of the following drugs? Yes ____ No ____ If no, go to #12. ____ penicillin ____ tetracycline ____ sulfa drugs ____ “mycins” (erythromycin) ____ aspirin ____ Levaquin, Cipro, floxin ____ Ceclor (cephalosporin) ____ codeine, morphine, Demerol -4- Others _______________ _____________________ _____________________ _____________________ Continue on back through pages 1-7 12. INSECTS: Have you ever had an allergic reaction to an insect? Yes ____ No ____ If no, go to #13. ____ bee ____ yellow jacket ____ fire ant ____ other ____ wasp ____ hornet ____ deer fly What happened? Local swelling Yes ____ No ____ Hives, swelling, itching over the entire body Yes ____ No ____ Other_________________________________________________________________________________________ When did the last reaction occur? Approximate date ___________________________________________________ ______________________________________________________________________________________________ 13. ENVIRONMENTAL FACTORS: If does not apply, go to #14. (1) Location: (*) Where your symptoms are worse. () where your symptoms are better. ____ indoors ____ outdoors ____ at home ____ at school or at work ____ in air conditioning ____ away from home ____ the same at all locations (2) Environmental Exposure: Check the following items that best describe your surroundings: Residence Bedroom How long have you lived in your ____ wall-to-wall carpet present dwelling? ____ years ____ carpets in bedroom, how old ____ ? Type of mattress? Regular ____ Water ____ Type of pillow? Dacron ____ Feather ____ Does your mattress or pillow have airtight covers? Yes ____ No ____ Is there mold growing in your house? ____ If yes, where? ___________________________________________ What kind of animals (birds also) do you have? ____________________________________________________ Are they indoors at any time? Yes ____ No ____ How many years? _________________________________ 14. PERSONAL-SOCIAL FACTORS: (EVERYONE MUST ANSWER COMPLETELY) What is your occupation? Does anyone practice any hobbies or occupations in your home that produce vapors, or dust, or strong odors? Yes ____ No ____ If yes, what? Do you smoke cigarettes? Yes ____ No ____ How many cigarettes per day? ____ Did you ever smoke? Yes ____ No ____ How long? ____ years. Average of how many packs per day? ____ Does anyone smoke in your home? Yes ____ No ____ How many persons? ____ Do you abuse alcoholic beverages? Yes ____ No ____ More than 2-3 drinks per day? ____ Do you use illicit drugs (confidential)? Yes ____ No ____ 15. FAMILY HISTORY: (EVERYONE MUST ANSWER COMPLETELY) Living/deceased Living/deceased How many How many Father Mother Brothers? Sisters? How many Children? Does any of your family have any of the following illnesses? (Check) Hay fever Asthma Eczema Hives Sinus trouble Any other illnesses? Is any family member deceased? ____________________ Cause? _________________________________________ _________________________________________________________________________________________________ Do any illnesses seem to run on your father’s or mother’s side of the family? _________________________________________________________________________________________________ Diabetes, hypertension, heart disease, stroke, other? _____________________________________________________ ________________________________________________________________________________________________ -5- Continue on back through pages 1-7 16. PAST HISTORY: (EVERYONE MUST ANSWER COMPLETELY) (1) Have you ever had any of the following illnesses? ____ tuberculosis ____ pneumonia ____ kidney disease ____ ulcer disease ____ rheumatic heart disease ____ diabetes ____ heartburn ____ thyroid disease ____ hypertension ____ cancer ____ radiation therapy ____ blood transfusion ____ kidney stones ____ liver disease ____ high risk for AIDS ____ sleep apnea (2) What surgery have you had? (tonsillectomy, nasal surgery, etc.). Approximate dates: __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ (3) Have you had any serious illness or injuries which led to hospitalization? Yes ____ No ____ List type and year: ___________________________________________________________ __________________________________________________________________________________________ (4) Have you received the Pneumovax vaccine? Yes ____ No ____ Do you know? ____ (5) Do you receive the yearly flu vaccine? Yes ____ No ____ Do you know? ____ Please list all medications you take and the dose, including over-the-counter medications: (1) _________________________ (6) _________________________ (2) _________________________ (7) _________________________ (3) _________________________ (8) _________________________ (4) _________________________ (9) _________________________ (5) _________________________ (10) ________________________ REVIEW OF SYSTEMS: (EVERYONE MUST ANSWER COMPLETELY) Do you have any of the following at this time? (Check) General Cardiovascular ____ weight loss ____ chest pain ____ chills ____ chest pain with exercise ____ loss of appetite ____ calf pain with exercise ____ fatigue ____ ankle swelling ____ poor memory ____ fall asleep during the day Endocrine ____ snoring is a problem ____ cold intolerance ____ heat intolerance Musculoskeletal ____ morning joint stiffness and aching ____ painful, swollen joints ____ muscle tenderness or pain ____ muscle weakness Kidney ____ trouble starting urine ____ bed wetting ____ burning with urination ____ loss of urine with cough or sneeze ____ frequent urination during the night Gynecological ____ excess bleeding ____ change in menstrual cycle Blood ____ bleed or bruise easily ____ swollen lymph nodes Gastrointestinal ____ nausea ____ vomiting ____ diarrhea ____ change in bowel habits ____ trouble swallowing (food gets stuck) ____ heartburn ____ black bowel movements ____ blood in bowel movement Neurological ____ weakness/clumsiness ____ tingling, burning, or numbness of extremities Other ____ lumps or bumps under arms ____ lumps or bumps in breasts Psychological ____ fearful, anxious ____ excessive worry ____ crying spells ____ trouble sleeping ____ behavior problems ____ depression -6- Continue on back through pages 1-7 ADULT SLEEP SCALE (AGE 18 AND OLDER) Are you sleepy during the day? If so, complete the following using the appropriate numbers, 0 through 3: 0 = not sleepy during the day; 1 = slight chance of dozing; 2 = moderate chance of dozing; 3 = high chance of dozing Chance of dozing ________ ________ ________ ________ ________ ________ ________ ________ Situation of dozing/falling asleep Sitting and reading Watching television Sitting inactively in a public place (theater or meeting) As a passenger in a car for an hour without a break Lying down to rest in the afternoon Sitting and talking to someone Sitting quietly after lunch without alcohol In a car, while stopped for a few minutes in traffic PEDIATRIC SLEEP SCALE (AGE 2 TO 17) FILL OUT IF THIS APPLIES TO YOU Complete using 0 = No or don’t know; 1 = Yes While sleeping, your child ________ Snores more than half the time ________ Always snores ________ Snores loudly ________ Has heavy or loud breathing ________ Has trouble breathing, struggles to breathe ________ Have you seen your child stop breathing during the night? If so, describe ___________________ Does your child ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ ________ Tend to breathe through the mouth during the day? Have a dry mouth on waking up in the morning? Occasionally wet the bed? Wake up feeling unrefreshed in the morning? Have a problem with sleepiness during the day? Has a teacher or other supervisor commented that your child appears sleepy during the day? Is it hard to wake your child up in the morning? Did your child stop growing at a normal rate at any time since birth? Is your child overweight? (if so, at what age did this first develop? ________) Have difficulty organizing tasks and activities? Is easily distracted by extraneous stimuli? Fidgets with hand or feet or squirms in seat? Is “on the go” or often acts as if “driven by a motor”? Interrupts or intrudes on others (for example, butts into conversations or games) ? Please list anything you wish to add which the questionnaire did not address. _________________________________________________________________________________________________ _________________________________________________________________________________________________ _________________________________________________________________________________________________ _________________________________________________________________________________________________ To the best of my knowledge, I have answered the complete questionnaire. ________________________________ Signature Reviewed form with the patient in its entirety. ______________________________ Joseph J. Callanan, M.D. ________________________________ Neetu Talreja, M.D. -7-