Obstetrics PGY1 - Department of Family & Preventive Medicine
advertisement

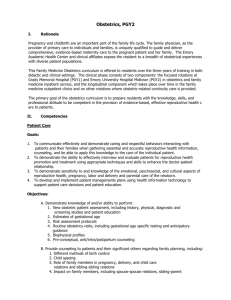
Obstetrics I. Rationale Pregnancy and childbirth are an important part of the family life cycle. The family physician, as the provider of primary care to individuals and families, is uniquely qualified to guide and deliver comprehensive, evidence-based maternity care to the pregnant patient and her family. The Emory Academic Health Center and clinical affiliates expose the resident to a breadth of obstetrical experiences with diverse patient populations. This Family Medicine Obstetrics curriculum is offered to residents over the three years of training in both didactic and clinical settings. The clinical phase consists of two components: the focused rotations at Grady Memorial Hospital (PGY1) and Emory University Hospital Midtown (PGY2) in obstetrics and family medicine inpatient service, and the longitudinal component which takes place over time in the family medicine outpatient clinics and on other rotations where obstetric-related continuity care is provided. The primary goal of the obstetrics curriculum is to prepare residents with the knowledge, skills, and professional attitude to be competent in the provision of evidence-based, effective reproductive health care to patients. II. Competencies Patient Care Goals: A. To communicate effectively and demonstrate caring and respectful behaviors interacting with patients and their families when gathering essential and accurate reproductive health information, counseling, and be able to apply this knowledge to the care of the individual patient. B. To demonstrate the ability to effectively interview and evaluate patients for reproductive health promotion and treatment using appropriate techniques and skills to enhance the doctor-patient relationship. C. To demonstrate sensitivity to and knowledge of the emotional, psychosocial, and cultural aspects of reproductive health, pregnancy, labor and delivery and parental care of the newborn. D. To develop and implement patient managements plans using health information technology to support patient care decisions and patient education. Objectives: A. Demonstrate knowledge of and/or ability to perform: 1. New obstetric patient assessment, including history, physical, diagnostic and screening studies and patient education 2. Estimates of gestational age 3. Risk assessment protocols 4. Routine obstetrics visits, including gestational age specific testing and anticipatory guidance 5. Biophysical profiles 6. Pre-conceptual, anti/intra/postpartum counseling B. Provide counseling to patients and their significant others regarding family planning, including: Last updated March 7, 2013 1. 2. 3. 4. Different methods of birth control Child spacing Role of family members in pregnancy, delivery, and child care Impact on family members, including spouse-spouse relations, sibling-parent relations and sibling-sibling relations C. Provide counseling in a non-judgmental manner to patients and their significant others regarding various options for managing an unwanted pregnancy, recognizing that there are multiple religious, ethical, and moral considerations in this counseling, and if unable to provide comprehensive counseling, be able to refer to a provider who can. D. Communicate with a family, the news of fetal loss or congenital anomaly, recognizing the stages of grief, and appropriately scheduling the family back for follow-up. E. Provide clear explanatory information and obtain consent on all patients undergoing diagnostic or therapeutic procedures in a manner understandable to the patient. F. Discuss the pregnancy, treatment plan, anticipatory guidance, and lactation issues with the patient and her family in a manner understandable to all of them. G. Review questions with patients and their families and elicit any concerns they may have. Learning Activities: (check all that apply) Attending Rounds Research Conference X Multidisciplinary Rounds Grand Rounds Subspecialty Conference Morning Report X Other (specify) X Ethics/Comm Conference Specialty Conference Noon Conference Faculty Supervision Other (specify) PALS and Neonatal Resuscitation Course exams Last updated March 7, 2013 X X X Self-study OB Monographs Evaluation Methods: (check all that apply) X Attending Evaluation X Directly Supervised Procedures Program Director X In-Training Exam X Review x Oral Report 360° Evaluation X Outpatient Clinics Case presentation Direct Patient Care Resident Seminar Journal Club Critical Appraised Topics Faculty facilitated selfcritique of videotaped patient encounter X X Morning Report: Senior Resident/Faculty Supervision and Feedback Record Review Medical Record document review Medical Knowledge Goals: A. To provide comprehensive antepartum care, utilizing assessment tools and screening methods for pregnant patients. B. To identify common antepartum complications and know how to manage these complications. C. To deliver appropriate intrapartum care for pregnant patients. D. To identify common intrapartum complications and know how to manage these complications. E. To provide appropriate postpartum care for pregnant patients. F. To identify postpartum complications and appropriately manage these complications. G. To provide effective care of the normal newborn. H. To perform neonatal resuscitation. I. To recognize ectopic pregnancies and manage them effectively. Objectives: A. Demonstrate knowledge of and assist in the performance of: 1. New obstetric patient assessment, including history, physical, diagnostic and screening studies and patient education 2. Estimates of gestational age 3. Risk assessment protocols 4. Routine obstetrics visits, including gestational age specific testing and anticipatory guidance 5. Biophysical profiles 6. Pre-conceptual, anti/intra/postpartum counseling B. Demonstrate knowledge of the following ante partum complications and their managements, assisting in the management of those that present in the clinical setting: 1. First trimester bleeding 2. Third trimester bleeding 3. Gestational diabetes 4. Pregnancy-induced hypertension, pre-eclampsia, eclampsia 5. IUGR / macrosomia 6. Premature rupture of membranes 7. Pre-term labor 8. Abdominal trauma 9. Advanced maternal age 10. Abnormal AFP 11. Anemia 12. Abdominal pain 13. Sexually transmitted infections 14. UTI/ pyelonephritis 15. Positive group B strep 16. Oligohydramnios 17. Polyhydramnios 18. Abnormal lie 19. Hyperemesis gravidarum 20. Post-date pregnancy 21. Size-date discrepancy Last updated March 7, 2013 C. Demonstrate knowledge of and/or ability to perform under faculty supervision: 1. Pudendal/local block anesthesia 2. Normal vaginal delivery 3. Placement of Fetal scalp electrode 4. Placement of intrauterine pressure catheter 5. Vacuum/forceps delivery 6. Episiotomy and repair 7. External fetal monitoring 8. Analgesia during pregnancy 9. Determination of rupture of membranes 10. Leopold maneuvers 11. Determination of cervical dilatation, effacement, presentation, station 12. Use of Ultrasound to determine presentation 13. Stages of labor, and normal labor curve 14. First person assist in Cesarean Section D. Demonstrate knowledge of the following intrapartum complications and their managements, managing or assisting in the management of those that present in a clinical setting under faculty supervision: 1. Prolonged rupture of membranes 2. Abnormal presentation, position 3. Fever 4. Active herpes 5. Labor disorders 6. Meconium 7. Vaginal/cervical lacerations and repair 8. Vacuum delivery 9. Breech delivery 10. Retained placenta 11. Shoulder dystocia 12. Abnormal fetal tracking E. Demonstrate knowledge and display skills under faculty supervision to perform: 1. Manual extraction of placenta 2. First assist of tubal ligation and hysterectomy F. Demonstrate knowledge and displays skills in the management of post-epidural complications under faculty supervision for: 1. postpartum hemorrhage 2. postpartum infection 3. postpartum PIH 4. amniotic fluid embolism G. Demonstrate knowledge of care of the normal newborn including: 1. Estimating gestational age by Dubowitz criteria 2. Initial physical examination 3. Initial prophylactic medications 4. Initial feeding of the infant in the delivery room 5. Ability to perform circumcisions under faculty supervision H. Demonstrate knowledge of and skills in neonatal resuscitation by passing the course and performing correctly in the clinical setting. Last updated March 7, 2013 I. Describe typical signs and symptoms, the work-up, and management of an ectopic pregnancy. Learning Activities: (check all that apply) x Attending Rounds Research Conference x x Multidisciplinary Rounds Grand Rounds Subspecialty Conference Morning Report Other (specify) Self study Ob modules x x Ethics/Comm Conference Specialty Conference Noon Conference Faculty Supervision Ambulatory Care Clinic Evaluation Methods: (check all that apply) X Attending Evaluation X Directly Supervised Procedures Program Director X In-Training Exam X Review x Oral Report 360° Evaluation X Other (specify) PALS and Neonatal Resuscitation Course exams X Outpatient Clinics x x x X X Direct Patient Care Resident Seminar Journal Club Critical Appraised Topics Neonatal Resuscitation and PALS courses Morning Report: Senior Resident/Faculty Supervision and Feedback Record Review Medical Record document review Case presentation Practice-Based Learning and Improvement Goals: A. To understand the need for and engage in continuing self-education about updates in obstetrics using information technology and other modes for learning evidence-based care. B. To identify gaps in obstetrics knowledge and skills and set learning and self improvement goals. C. To develop a vision for whether obstetrics may be part of future practice. Objectives: A. Discuss the value of including Obstetrics in the practice of Family Medicine. B. Accept and respond positively to constructive feedback for self- improvement. C. Construct an educational experience that allows for additional training in obstetrics as indicated, based on self-identified personal knowledge and skills gaps to be prepared for on anticipated future practice including obstetrics. If obstetrics are not to be part of a future practice, describe how the family physician may interact with the pregnant patient and her family to help ensure the most gain from the experience. D. Participate in a quality improvement/practice management project to assess the degree of compliance with an evidence-based or best practice clinical guideline related to Obstetrics, and report the findings and plans for improvement. E. Identify sources to which residents may turn for more information or continuing education on family-centered obstetrics. Last updated March 7, 2013 Learning Activities: (check all that apply) Attending Rounds Research Conference Multidisciplinary Rounds Grand Rounds Subspecialty Conference Morning Report Other (specify) X Outpatient Clinics Ethics/Comm Conference Specialty Conference Noon Conference Faculty Supervision Portfolio development Evaluation Methods: (check all that apply) X Directly Supervised Attending Evaluation Procedures Program Director In-Training Exam Review Direct Patient Care Resident Seminar Journal Club Critical Appraised Topics QI Project Morning Report X Faculty Supervision and Feedback Quality Improvement Project presentation Other (specify) Interpersonal and Communication Skills Goals: A. To learn to communicate efficiently and effectively with obstetric patients and their families, the health care team and obstetric consultants. B. To communicate and document clearly and completely using written and verbal methods. C. To demonstrate sensitivity to patient and family cultural, lifestyle, race, gender, age, disability issues. D. To develop effective interpersonal and teaching skills for participation in the healthcare team and for support of maternity patients and their families including use of language translators. Objectives: A. Prepare a consultant referral form which contains a complete and succinct summary of the patient’s diagnosis, accurate description of the problem, the question for the consultant, and other information pertinent to the referral. B. Utilize, and facilitate the communication of accurate information effectively with other members of the health care team, patients and their families in a timely manner. C. Present patient cases accurately and effectively. D. Effectively, accurately, efficiently document obstetric patient encounters in the medical record. E. Communicate effectively with obstetric patients and their families. F. Communicate effectively verbally and in writing with community healthcare partners. Learning Activities: (check all that apply) x Attending Rounds Research Conference Multidisciplinary Rounds Last updated March 7, 2013 Ethics/Comm Conference Outpatient Clinics x Direct Patient Care Grand Rounds Subspecialty Conference Morning Report Other (specify) Videotape patient encounter and self-critique x Specialty Conference Noon Conference Faculty Supervision Ambulatory Care Clinic x Evaluation Methods: (check all that apply) x Attending Evaluation x Directly Supervised Procedures Program Director Review x In-Training Exam 360° Evaluation x Other (specify) x Checklist evaluation of Patient interaction videotaped performance Patient surveys Other (specify) x Resident Seminar Journal Club Critical Appraised Topics Focused observation of faculty professional role models Morning Report: x Supervision and Feedback Senior Resident/Faculty Videotape review of patient encounter Professionalism Goals: A. To develop a commitment to carrying out professional responsibilities B. To adhere to ethical principles C. To develop sensitivity to a diverse patient populations Objectives: A. Displays behavior that is patient-centered, team-oriented, compassionate, ethical and sensitive to patient culture and beliefs. B. Demonstrate personal responsibility for compliance with residency program policies and procedures, for responsible management of patient records, follow-up on diagnostic study results, patient phone requests for information, clarification, and medication. C. Displays behavior that reflects initiative, punctuality, dependability and responsibility. D. Completes charting in a timely manner, and maintains up-to-date duty hour, delivery volume and obstetric procedure documentation. E. Demonstrate attention to detail and appearance that reflects respect for self, the profession, patients and families. Learning Activities: (check all that apply) Attending Rounds Research Conference Multidisciplinary Rounds Grand Rounds Morning Report Other (specify) Prepare an EBM Case Last updated March 7, 2013 Ethics/Comm Conference x Outpatient Clinics x Direct Patient Care Specialty Conference Noon Conference Resident Seminar Journal Club Faculty Supervision Critical Appraised Topics Review Self critique patient interaction videotape x Observe behavior of faculty role models Evaluation Methods: (check all that apply) X Attending Evaluation X Directly Supervised Procedures Program Director Review X X Other(specify) 360° Evaluation In-Training Exam Morning Report X Faculty Supervision and Feedback Portfolio Other(specify) Videotape review and facilitated critique Systems-Based Practice Goals: A. To understand the value of obstetrical care in the practice of family medicine and the positive impact on patients and families. B. To identify and utilize community and system resources to support effective and efficient maternity care. C. To learn to bill appropriately for services and procedures. D. To utilize a team approach to patient care and quality improvement practices. Objectives: A. Participated effectively in team-based, patient-centered approach to comprehensive health care for female patients and their families B. Meet patient needs or arrange for the comprehensive reproductive health promotion and management services C. Fully utilize community and system resources to optimize high quality reproductive health management. D. Demonstrated the interest in teaching less experienced learners how to provide high quality, patient centered obstetrical care within the healthcare system and community. E. Utilize appropriate coding and billing procedures and clinic resources for efficient, effective, patient centered reproductive health services and practice management. F. Demonstrate sensitivity to cost containment, patient safety, best practices guidelines, and comparative effectiveness in clinical decisions. G. Compare and contrast the patient satisfaction, provider satisfaction, practice cost/revenue and obstetric patient health outcomes in Family Physician practices that offer or choose not to offer obstetrical services H. Participate in a practice management project on a healthcare systems topic. Learning Activities: (check all that apply) x Attending Rounds Research Conference Multidisciplinary Last updated March 7, 2013 Ethics/Comm Conference x Outpatient Clinics x Direct Patient Care Rounds Grand Rounds Subspecialty Conference Morning Report x x Specialty Conference Noon Conference x x Resident Seminar Journal Club Faculty Supervision x Critical Appraised Topics Other (specify) Practice Management project Evaluation Methods: (check all that apply) Attending Evaluation Directly Supervised Procedures x Program Director Review In-Training Exam Other(specify) Other(specify) Morning Report x Faculty Supervision and Feedback Portfolio Project presentation III. Instructional Strategies (see above) A. Observation of obstetrics preceptor role models and upper level resident’s assessment of actual patients in labor and delivery B. Management of actual patients in continuity clinic case discussions C. Ambulatory care conference and core obstetric readings D. Associated rotations: family medicine, pediatrics, and newborn nursery IV. Evaluation Strategies (see above) A. Observation of resident by obstetric preceptor (PC, K, PBL, CS, P, SBP) B. Observation of resident clinical performance and medical record documentation by clinic preceptor (PC, K, CS, P) C. Procedure/diagnosis documentation. (PC, K, CS, P) D. End of rotation evaluation (forms: all competencies) E. Performance on the Obstetrics section of the in-training exam and mini-quizzes (K) F. Evaluation of case presentation PC, K, PBL, CS, P, SBP) V. Implementation Methods The PGY1 resident is scheduled for the Obstetric core rotation at Grady Memorial Hospital, where he/she joins the team of an OB intern and an OB PGY3 resident, who assumes responsibility for the team under the supervision of OB/GYN faculty. The team is responsible for the triage area. The Family Medicine resident and the OB intern share responsibility for seeing all patients coming through the triage area, and all patients are signed out to the OB PGY3 resident. The Family Medicine resident primarily sees term patients (=/> 37 weeks gestation), except when the OB intern is unable to handle the volume of pre-term patients and beginning the patient evaluation to rule out the need for emergency measures. The Family Medicine resident is expected to attend morning report, the Grady OB/Gyn didactic sessions, and will participate in the labor, delivery and C-section activities. Each Family Medicine resident should have the goal of doing and documenting at least 30 vaginal deliveries by the end of this rotation. Last updated March 7, 2013 The obstetric curriculum has several components. During all training years, the didactic teaching sessions includes obstetrics-related presentations. In the PGY-1 year the resident rotates through the Ob-Gyn department of Grady Memorial Hospital for four weeks. The resident is responsible for triage of all patients that present to this clinic along with the OB intern. In addition the resident will be called to all deliveries during the shift. The rotation consists of 12 hour shifts (7pm-7am) Monday through Friday. The resident is required to read the following monographs (pregnancy care and medical conditions of pregnancy) and to score >90% on the written exam. It is required that on at least three occasions during this rotation that the supervisor rechecks the examination of the cervix to document competency in cervical examination. In the PGY-2 year the resident rotates through the Emory University Hospital Midtown delivery suite for a six week rotation. The FM resident is responsible for triage and management of labor under the supervision of the Ob-Gyn attending physicians. In addition the resident is first assist on all C-sections that occur during the residents shift. The rotation consists of Monday to Friday shifts of 7:00 AM to 7:00 PM with call in the family medicine service every fourth night. The resident is taught and expected to memorize and use the pneumonic DR C BRAVADO for interpreting rhythm strips. Throughout the residency, residents follow their own obstetric patients in their continuity clinic. These patients are scheduled into the Family Medicine Clinic beginning in their intern year. They are followed solely by each individual resident under the supervision of Family Medicine faculty. These patients deliver at Emory University Hospital Midtown. The resident is expected to perform vaginal deliveries and assist the OB department faculty in C-sections of their continuity patients. Residents are expected to manage and deliver at least 10 continuity OB patients prior to graduation. Contact Information: Jessica Arluck, MD Pic # 10382 Chiefs: Tara Cleary tcleary@emory.edu Martina Badell mbadel@emory.edu Emory University Hospital Midtown 550 Peachtree Street, NE Atlanta, GA 30308 (404) 686 8121 ofc (404) 778 3527 fax VI. Suggested Readings Articles: Labor Analgesia, AFP, March 1, 2012 Steven D. Schrock, MD, and Carolyn Harraway-Smith, MD. Managing Adverse Birth Outcomes: Helping Parents and Families Cope Van Dinter MC, Graves L Am Fam Physician. 2012 May 1; 85(9):900-904. Office Management of Early Pregnancy Prine LW, MD, Macnaughton, H, MD Am Fam Physician. 2011 Jul 1; 84(1):75-82. Umbilical Cord Blood: A Guide for Primary Care Physicians MARTIN P., Kurtzburg J., Hesse B. Am Fam Physician. 2011 Sep 15; 84(6):661-666. Last updated March 7, 2013 Usta J., Antoun,J, Ambuel B, Khawaja M. Involving the Health Care System in Domestic Violence: What Women Want Ann. Fam. Med 2012 10:213-220; doi:10.1370/afm.1336 Moos M , Dunlop AL et al Healthier women, healthier reproductive outcomes: recommendations for the routine care of all women of reproductive age American Journal of Obstetrics & Gynecology Volume 199, Issue 6, Supplement B , Pages S280-S289, December 2008 The clinical content of preconception care: women with chronic medical conditions Anne L. Dunlop, MD, MPH; Brian W. Jack, MD; Joseph N. Bottalico, DO et al ACOG, 2008, Vol 199, # 6 Liver Disease in Pregnancy - February 15, 1999 - American Academy of Family Physicians http://www.aafp.org/afp/990215ap/829.html Medical Options for Early Pregnancy Termination August 1997, AFP http://www.aafp.org/afp/970800ap/abortion.html Urinary Tract Infections During Pregnancy February 1, 2000 American Academy of Family Physicians http://www.aafp.org/afp/20000201/713.html Obstetric Care in Patients with HIV Disease 117. Krist A.., Am Fam Physician 2001 Jan 1; 63(1):107- Neonatal Herpes Simplex Virus Infections Rudnick CM Hoekzema GS Am Fam Mar 15; 65(6):1138-1142. Physician. 2002 Management of Vaginitis Owen M Clenney TL Am Fam Physician. 2004 Dec 1; 70 (11):21252132. Screening and Treatment for Sexually Transmitted Infections in Pregnancy Majeroni BA and Ukkadam S. Am Fam Physician. 2007 Jul 15; 76 (2):265-270. Screening for Bacterial Vaginosis in Pregnancy to Prevent Preterm Delivery Lin KW LoBrano MB Am Fam Physician. 2009 Apr 15; 79 (8):697-698. Screening for Genital Herpes Putting Prevention into Practice Am Fam Physician. 2005 72(01):135-136. Jul 1; Epilepsy in Pregnancy - October 15, 1997 - American Family Physician http://www.aafp.org/afp/971015ap/rochest.html Safety of Radiographic Imaging During Pregnancy April 1, 1999 American Academy of Family Physicians http://www.aafp.org/afp/990401ap/1813.html 04/01/99, NHBPEP Report on High Blood Pressure in Pregnancy: A Summary for Family Physicians - July 15, 2001 - American Family Physician http://www.aafp.org/afp/20010715/263.html 07/18/01 Intrauterine Growth Restriction: Identification and Management - August 1998 - American Academy of Family Physicians http://www.aafp.org/afp/980800ap/peleg.html 11/16/00, Pyelonephritis in Pregnancy: Is Hospitalization Necessary? - March 15, 2000 - American Academy of Family Physicians http://www.aafp.org/afp/20000315/tips/25.html 12/01/00 Last updated March 7, 2013 Diagnosing and Managing Ectopic Pregnancy - February 15, 2001 - American Family Physician http://www.aafp.org/afp/20010215/tips/11.html 02/20/01 Evaluation of Pregnant Women Exposed to Respiratory Viruses - May 15, 2000 - American Academy of Family Physicians http://www.aafp.org/afp/20000515/3065.html 07/10/00 Emergency Postcoital Contraception - November 15, 2000 - American Family Physician http://www.aafp.org/afp/20001115/2287.html 11/21/00 Case Studies in Partner Violence - December 1, 1999 - American Academy of Family Physicians http://www.aafp.org/afp/991201ap/2569.html 12/01/99 Current Trends in Cervical Ripening and Labor Induction - August 1999 - American Academy of Family Physicians http://www.aafp.org/afp/990800ap/477.html 07/31/99 HELLP Syndrome: Recognition and Perinatal Management - September 1, 1999 - American Academy of Family Physicians http://www.aafp.org/afp/990901ap/829.html External Cephalic Version - September 1, 1998 - American Academy of Family Physicians http://www.aafp.org/afp/980901ap/coco.html 08/24/01 Interpretation of the Electronic Fetal Heart Rate During Labor - May 1, 1999 - American Academy of Family Physicians http://www.aafp.org/afp/990501ap/2487.html Common Peripartum Emergencies - November 1, 1998 - American Academy of Family Physicians http://www.aafp.org/afp/981101ap/morrison.html Management of Suspected Fetal Macrosomia - January 15, 2001 - American Family Physician http://www.aafp.org/afp/20010115/302.html Kirkham C, Harris S, Grzybowski S. Evidence-based prenatal care: part I. General prenatal care and counseling issues. Am Fam Physician 2005; 71:1307-16. Review. Kirkham C, Harris S, Grzybowski S. Evidence-based prenatal care: part II. Third-trimester care and prevention of infectious diseases. Am Fam Physician 2005; 71:1555-60. Review ACOG Obstetrics Guidelines #263 August 2011 Policy Statement Maternity Leave in Normal Pregnancy #236 Nov 2009 Clinical Practice Guideline Immunization in pregnancy Replaces #220 (Dec 08) #235 Oct 2009 Clinical Practice Guideline Active management of the third stage of labour: prevention and treatment of postpartum hemorrhage Replaces #88 (April 2000) #214 Sept 2008 to 42+0 weeks Clinical Practice Guideline Guidelines for the management of pregnancy at 41+0 Replaces #15 (Mar 1997) # 206 Mar 2008 Clinical Practice Guideline Diagnosis, evaluation and management of the hypertensive disorders of pregnancy # 203 Feb 2008 Clinical Practice Guideline Rubella in Pregnancy Last updated March 7, 2013 # 197 Sept 2007 Clinical Practice Guideline Fetal Health Surveillance: Antepartum and Intrapartum Consensus Guideline Replaces #130 (July 2003), #90 (June 2000); #112 (March 2002); and # 112 (April 2002) #190 April 2007 Policy Statement Pospartum Maternal and Newborn Discharge Replaces #56 (Oct 1996) # 006538 NGC Feb.2008 Asthma in pregnancy. American College of Obstetricians and gynecologists Vaginal Birth after Previous Cesarean 2010 National Guideline Clearinghouse http://guideline.gov/content.aspx?id=23853 Diabetes in pregnancy. Management of diabetes and its complications from pre-conception to the postnatal period. 2008 Mar. NGC: 007192 National Collaborating Centre for Women’s and Children’s Health - National Government Agency http://guideline.gov/content.aspx?id=14324&search=pregnancy Hypertension in pregnancy. The management of hypertensive disorders during pregnancy. 2010 Aug. NGC: 008073 National Collaborating Centre for Women’s and Children’s Health - National Government Agency http://guideline.gov/content.aspx?id=24122&search=pregnancy Practice parameter update: management issues for women with epilepsy—focus on pregnancy (an evidence-based review): teratogenesis and perinatal outcomes. Report of the Quality Standards Subcommittee and Therapeutics and Technology Subcommittee of the American Academy of Neurology and American Epilepsy Society. 2009 July NGC: 007263 American Academy of Neurology http://guideline.gov/content.aspx?id=14680&search=pregnancy VTE, thrombophilia, antithrombotic therapy, and pregnancy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. 2001 Jan (revised 2012 Feb). NGC: 008939 American College of Chest Physician http://guideline.gov/content.aspx?id=35275&search=pregnancy Thromboembolism in Pregnancy: Clinical Guidelines - February 1, 2001 - American Family Physician http://www.aafp.org/afp/20010201/tips/7.html 02/06/01 Management of Pre-term Birth, Obstetrics and Gynecology Clinics, Vol 39, Issue 1, March 2012 US Preventive Services Task Force Neural Tube defects: Folic Acid for Prevention Recommendations, May, 2009 http://www.uspreventiveservicestaskforce.org/uspstf/uspsnrfol.htm FP Practice Endorsed Guidelines and Policies Trial of Labor After Cesarean (TOLAC), Formerly Trial of Labor Versus Elective Repeat Cesarean Section for the Woman With a Previous Cesarean Section, March 2005 A Review of the Evidence and Recommendations by the American Academy of Family Physicians. Available at: http://www.aafp.org/online/en/home/clinical/clinicalrecs/ob/tolac.html and http://www.aafp.org/online/etc/medialib/aafp_org/documents/clinical/clin_recs/tolacpolicy.Par.0001.F ile.tmp/clinicalrec_tolac.pdf TOLAC Shared Patient Provider decision tool: Last updated March 7, 2013 http://www.aafp.org/online/etc/medialib/aafp_org/documents/clinical/patient_ed/tolaccolor.Par.0001.File.tmp/TOLAC-color.pdf Prevention of Perinatal Group B Streptococcal Disease: Revised Guidelines from CDC, 2010 (endorsed by AAFP with reservations) Available at: http://www.aafp.org/online/etc/medialib/aafp_org/documents/clinical/clin_recs/cdcgbs.Par.0001.File.t mp/MMWRGroupBStreptococcaldisease11192010.pdf Circumcision: Position Paper on Neonatal Circumcision Board Approved: August 2007 Reaffirmed Available at: http://www.aafp.org/online/en/home/clinical/clinicalrecs/guidelines/Circumcison.html Immunizations in Pregnancy from CDC (updated Oct, 2011). Chart and flyer available at: http://www.cdc.gov/vaccines/pubs/downloads/f_preg_chart.pdf and http://www.cdc.gov/vaccines/pubs/downloads/f_preg.pdf AAFP: FP Essentials Monographs and Policies Genetics Update May 2012 (#396) http://www.aafp.org/online/en/home/cme/selfstudy/fpe/fpeissues.html Care of the Pregnant Patient, 2011 (#382) Society for Maternal/Fetal Medicine: Maternal Fetal Medicine Monograph, High Risk Pregnancy Care 2009 https://www.smfm.org/attachedfiles/SMFMMonograph3.1.pdf Finley BJ, Harnisch DR. Women’s Genitourinary Conditions. (# 314) AAFP Home Study. Leawood, Kan: American Academy of Family Physicians, 2005. Soldat LG, Batra CP, Murad E. Medical Conditions in Pregnancy. (#316) AAFP Home Study. Leawood, Kan: American Academy of Family Physicians, 2005. Pauwels J, Olifer L, Huntington J, Church L. Reproductive Health Update. (#340), AAFP Home Study. Leawood, Kan: American Academy of Family Physicians, 2007. Texts: Cunningham F, Williams JW. Williams Obstetrics. 23nd ed. New York, N.Y.: McGraw-Hill Medical, 2010. Available Books at Ovid at Emory HS Library Gibbs R, Kirlan B et al Danforth’s Obstetrics and Gynecology. 10th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins, 2008. Available Books at Ovid at Emory HSC Library American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care. 6th ed, Elk Grove Village, Ill.: American Academy of Pediatrics, 2007. Creasy RK, Resnik R, Iams JD. Maternal-Fetal Medicine: Principles and Practice. 6th ed. Philadelphia, Pa.: Saunders, 2009. (Via MD Consult at Emory Health Sciences Library) Weiner: Drugs for Pregnant and Lactating Women, 2nd ed, 2009. (MD Consult thru Emory HSc Library) Brunt, B Evidence-Based Competency Management for the Obstetrics Unit, 2nd ed, 2008 (R2 Library) Gabbe SG, Niebyl JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 6th ed. Philadelphia, Pa.: Churchill Livingstone/Elsevier, 2012. (Available at MD Consult) Last updated March 7, 2013 Speroff L, Fritz MA. Clinical Gynecologic Endocrinology and Infertility. 8th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins, 2011. (Books at OVID) Websites: The Center for Disease Control and Prevention http//:www.cdc.gov/reproductivehealth/MaternalInfantHealth/ (revised 1/19/12) http//:www.cdc.gov/women/ (modified, 2012) http://www.womenshealth.gov/ http://www.womenshealth.gov/publications/ourpublications/breastfeeding-guide/(Breast feeding) http://www.womenshealth.gov/publications/our-publications/pregnancy-dos-donts.pdf (Pregnancy) http://www.womenshealth.gov/publications/our-publications/pregnancy_food_donts.pdf Nutrition) Association of Maternal and Child Health Programs http://www.amchp.org American College of Obstetricians and Gynecologists http://www.acog.org National Guideline Clearinghouse http:/www.guideline/index.aspx American Pregnancy Association (Tools and Pt Ed) http://www.americanpregnancy.org/ Last updated March 7, 2013