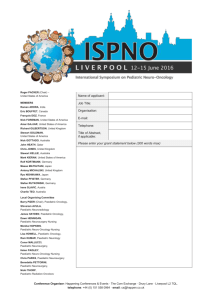
guidelines for writing a winning abstract
advertisement

P291 Autosomal dominant polycystic kidney disease in childhood, what are we doing? Richardson ARW1, Polubothu S1, Sinha MD2, Kerecuk L3, Winyard PJD1 1 Nephro-Urology Unit, UCL Institute of Child Health, 30 Guilford Street, London, UK. 2 Department of Paediatric Nephrology, Evelina Children's Hospital, Westminster Bridge Road, London, SE1 7EH, UK 3 Department of Nephrology, Birmingham Children's Hospital, Birmingham, UK Problem: Autosomal Dominant Polycystic Kidney Disease (ADPKD) can be identified in childhood either opportunistically, due to screening if there is a family history, or because of symptoms prompting investigation. Rare cases lead to CKD V during childhood, and up to a quarter develop hypertension, but most do not have overt issues. There are no national guidelines on follow up, which raises a dilemma over optimal clinical management for children with ADPKD: should we be investigating them aggressively or not medicalise them until they develop signs and symptoms? Purpose: To ascertain current practice amongst UK paediatric nephrologists on the management of ADPKD in childhood. Design: Questionnaire study using a case based approach, consisting of 4 clinical vignettes two of which were for a young child and two for a young adult. This was refined using the Delphi approach in two local meetings. For each age there was a child who had cysts confirmed on ultrasound, and a child with a positive family history with a negative ultrasound. This was emailed to all paediatric nephrologists within the UK and paediatric nephrology trainees, responses were anonymised to person but not clinical centre. Data has been analysed by the team who initially designed and trialled both this questionnaire and the original paper pilot. Findings: There were 45 responses for the child scenario and 19 for the young adult, with at least one reply from each paediatric nephrology centre in the UK. DNA analysis was rarely performed: only 11% would organise it in a child with unknown diagnosis, although 33% felt it warranted in the young adults with clinical uncertainty. Children were more likely to be followed up in tertiary care, 69% with confirmed cysts 40% without, compared to young adults (58% and 28% respectively). Clinical assessments were remarkably similar across all four scenarios (i.e. irrespective of age or whether cysts were proven): the commonest review frequency (43% of respondents) was yearly with ‘one-off’ BP and urinalysis. Some centres only reviewed 5 yearly, though. Ambulatory BP is performed regularly by 24% of clinicians, and no one routinely performs an echocardiogram. There was more diversity in lipid screening: only 6% regularly undertake this in children, compared with 36% in young adults. Conclusion: Most UK children with uncomplicated ADPKD are being followed in specialist centres at yearly intervals. Assessments centre on blood pressure and urinalysis; no paediatric nephrologists are performing screening echocardiograms, and few instigate ambulatory BP or lipid screening. We would like to encourage debate on whether current approaches are sufficient, bearing in mind the high risk of cardiovascular morbidity and mortality in ADPKD and its likely origins in childhood. Is it time for national guidelines to standardise management? Relevance: ADPKD is often considered an adult condition but it is increasingly diagnosed in children, where national guidelines on management are lacking. We have assessed current practice in management of paediatric ADPKD in the UK, and question whether we should establish standard protocols to identify modifiable cardiovascular risk factors.