PCMOD3 - PC617StudyGuides
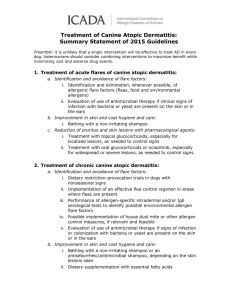
advertisement

Examination of the Skin 1. List the changes in skin related to aging. Structural changes o Decrease in Langerhans’ cells o Variation in size, shape and staining of keratinocytes o Decrease in thickness of the dermis o Loss of elastic tissue o Decrease in number of sweat glands, hair follicles, and specialized nerve ending o Decreased vascularity and an increase fragility of existing capillaries Functional changes o Decreased inflammatory response o Increase wound healing time o Thinning of the skin (increase fragility and risk of injury) o Decrease sweat capacity o Increase dryness secondary to decrease sebum production 2. Describe the health history, physical examination required when the patient presents with a skin problem. Alopecia LA, a 30 year old G3 P3 who is 6 months postpartum, comes to clinic complaining of scalp hair loss. 1. Describe the history, physical examination and laboratory tests that would be needed to diagnose nonscaring alopecia or telogen effluvium. 2. Describe the education about hair growth, changes in hair growth postpartum, and what she should do about the problem. Telogen effluvium-hair prematurely enters the telogen phase where mature hair is shed. Normally a person sheds 50-150 hairs a day. Caused by hormones and will spontaneously recover in about 6 months. 3. If after examining LA, the diagnosis is alopecia areata, what are the autoimmune endocrinopathies that have been associated with this complaint? Vitiligo Atopy (eczema, asthma, hay fever) Thyroid disease Pigmentation Changes SD, a 25 year old African American woman, has developed vitiligo on her face, neck and arms. 1. Explain to SD what vitiligo is and about her risk for other autoimmune diseases. Consider the psychological and emotional impact that this skin manifestation may cause for SD. 2. What are some cosmetic options for SD? 3. Pruritis MF, a 30 year old male, comes to the clinic complaining of itching. The symptoms indicate a systemic cause (probably jaundice). 1. What are the components of the history needed to diagnose the cause of the itching? Total skin exam to identify or exclude other dermatologic disorders. History:diurnal rhythms, character, severity, distribution, exacerbating and alleviating factors, previous treatment. Medication, alcohol use, past medical hx, exposures to environmental contacts and complete review of systems. 2. How would the history differ if the pruritis was due to an external cause? No 3. What are the suggested treatments for external causes of pruritis? Avoid irritants (including stopping medications) Cooling the skin-wear light clothing, air conditioning, cool compresses, calamine lotion or aqueous creams, tepid bath before bed, if inflammation a hydrocortisone cream or Capsaicin. 4. What are the suggested treatments for systemic causes of pruritis? Oral antihistamine like diphenhydramine, Non sedating antihistamines have not been effective. Rashes (Rhus dermatitis) Jonathon has a rash that developed 2 days after he returned from a hiking/camping trip. The rash is pruritic, in a linear distribution on both legs, and vescicular. He has tried hydrocortisone creme - but it is not helping. 1. What further history would be helpful? 2. What is the probable cause of the rash? 3. List the best treatment for this localized rash. Urticaria DF is a 20 year old G1P0 at 36 weeks in her pregnancy who is complaining about pruritic urticaria that has appeared on her abdomen and thighs. 1. Describe the history and physical examination needed. Past medical history History of urticaria in the past family history food exposures (ingestion, inhalation, contact) drug exposures (such as herbals, medications, supplements) infection exposures (such as viral hepatitis or infectious mononucleosis) potential physical triggers (such as cold, heat, exercise, sweating, pressure, sun/light exposure) history of insect bites or stings history of hormonal dysfunction occupational exposure to allergens or irritants review of systems (Dynamed) 2. Describe the treatment for this common complaint that is safe and effective for DF and her fetus. Zyrtec or Claritine both are Cat. B (Dynamed) Parasitic Infestation JK, a 20 year old male, complains of severe itching that has developed since spending the week end at a commune (4 days ago). He reports that several people there were complaining of itching. He has never had these symptoms before. 1. What are some focused history questions that will help determine whether or not JK has a scabies infestation? 2. Why would the itching become noticeably worse 3-4 days after exposure to the scabies mite? Describe the focused physical examination of JK who may have a scabies infestation. Describe the management, patient education, and follow-up if JK has scabies. 3. How would the management, patient education and follow-up differ if JK has pediculosis? Fungal skin infection (Intertrigo) BT, a 40 year old obese female with Type II diabetes mellitus, is seen in clinic complaining of a burning, pruritic rash under both breasts and in the groin area. She tells the provider that the rash is red and moist and the corn starch she has been using is not helping. 1. What is the diagnosis? Intertrigo caused by candida albicans 2. What pharmacologic therapy is indicated? Topical antifungal cream combined with low strength hydrocortisone cream (for inflammation and pruritis) applied 2-3 times/day for 7-14 days. 3. Describe the education necessary for BT to understand the cause, how to use the medication, and how to prevent recurrence of this problem. Stop using cornstarch (or talc) powder which can encourage growth. Keep area clean and dry. Wear cotton underwear and unrestrictive clothing. Tinea Pedis MK is a 19 year old star basketball player who complains of blisters between his toes and red weeping patches on both feet for the last 2 weeks. He has had similar toe lesions in the past, but his usual remedy of Tinactin powder is not helping. He says the problem is interfering with his shoe contract with a famous maker of athletic shoes. 1. During the physical examination, where else on his body should be inspected for lesions? Why? 2. What are the possible diagnoses? Give rationale for each choice. 3. Outline the management for MK to include any diagnostics that are appropriate, treatment, education, consultation/referral and follow-up. Education should include ways to prevent spread of the fungus to other parts of his body (if this is the correct diagnosis). Tinea unguium RJ is a 20 year old marathon runner for a college track team. He comes to clinic complaining of the nail on his great toe turning yellow and seeming to “come loose”. 1. What further history would be appropriate? Renal, liver dysfunction, drug history (P450 enzyme) 2. Describe the physical examination needed. Visual-nail will appear yellow and thickened. 3. What laboratory tests are indicated to help diagnose the problem? Potassium hydrochloride (KOH) microscopy prep. Scrape active lesion with #15 blade onto a glass slide, add 10% -20% KOH and apply cover slip. Gently heat sample and place under microscope. 4. Describe the most efficacious treatment regimen for RJ’s tinea unguium. Systemic antifungal. Terbinafine 250mg/day for 12 weeks. 5. What laboratory tests are indicated before initiating and during systemic therapy? CBC before therapy and every 6 weeks to neutropenia and liver function test initially and every 6 weeks. 6. Describe the best plan for patient education and follow-up. Reduce environmental factors avoiding moisture and constriction, wearing sandals in warm weather. Use talc powder, avoid cornstarch based powders because they encourage fungal growth. 7. What is the outcome criteria for evaluating the treatment of RJ’s tinea unguium? Responding to treatment. Usually returns despite treatment. Bacterial Infection (Cellulitis) Sam J., a 50 year old sawmill worker, presents to clinic complaining of a large area of red, raised painful skin on his right thigh. He first noticed it yesterday and had to take off from work to be seen today. His temperature is 100 F. 1. What further subjective (history) data would you ask of Sam J.? (Be sure to ask about any allergies to medication.) 2. Physical examination of Sam would include 3. List the differential diagnoses. 4. Describe the best management plan for Sam J. including treatment, education and follow-up. 5. Under what conditions should the provider refer Sam J. to an M.D.? 6. What is the outcome criteria for evaluating the treatment and education you have given Sam? Primary Herpes Labialis BA, a 17 year old recent high school graduate on her way to college, comes to clinic complaining of blisters that have erupted on her upper lip. “My mother says it’s a cold sore, but I haven’t had a cold.” 1. Where on the body can herpes simplex erupt? Where are the lesions most likely to erupt? HSV1- mainly cause oral lesions HSV2-mainly cause genital lesions Either type can erupt EITHER location Grouped vesicles on an erythematous base appear on the lips, facial area, throat or genital area. 2. What is the best treatment for this primary outbreak of herpes labialis? Acyclovir 200mg PO 5 times daily for 7-10 days 3. How would the treatment differ for recurrent outbreaks? Only severe cases should be treated. Acyclovir 400mg PO bid for 5 days 4. What patient education is appropriate for BA? Lifelong disease Ability to transmit HSV even with no lesions Use lip balm with sunscreen Atopic dermatitis Jessica is a 16 year old who suffers from atopic dermatitis. 1. 1. Explain the primary cause of atopic dermatitis to Jessica. 2. 2. Describe the usual treatment for atopic dermatitis to Jessica. Herpes Zoster Mae H. is an 80 year old African American grandmother who has senile dementia. She lives with her youngest daughter, son-in-law, and 3 teen aged children. The oldest of the children has a new baby boy (6 weeks old). Her daughter brings her to clinic today because Mae has developed blisters then crusted lesions of her right forehead and cheek. Mae picks at the lesions and has long fingernails. 1. What is the most important consideration or potential very serious consequence of herpes zoster in this area? There may be involvement of the trigeminal nerve that innervates the cornea and can cause permanent damage. 2. What cranial nerve is involved? trigeminal nerve 3. Would it be appropriate for the NP to give her treatment or should the NP consult/refer? Why? Refer to an ophthalmologist do to ocular complications. 4. What is the usual treatment for herpes zoster within the first 48 hours of the initial eruption? Antiviral treatment like Acyclovir 5. What are the education points that should be shared with Mae’s family? Transmission of virus to susceptible individuals (granddaughter and great grand baby) Pain control-Mae may not be able to verbalize Vaccinate after rash disappears (CDC) Picking at lesions may cause secondary infection 6. What are the potential complications of herpes zoster? Postherpetic neuralgia (nerve pain), facial palsy and motor paralysis. In immunodeficiency patients dissemination, pneumonia, hepatitis, meningoencephalitis and purpura fulminans. 7. Mae does not care for the baby and lives in a separate room. What should the NP tell her granddaughter about the transmission of herpes zoster to her baby? They cannot get Herpes zoster but if they got the virus it would present as chickenpox. You have to come in contact with the lesions for transmission. Teenage Acne Billy B. is a 15 year old who comes to clinic for treatment of acne. His mother has told him to scrub his face, stop eating chocolate, and to stop picking at the pimples. 1. Explain to Billy what acne is. 2. Explain to Billy how he can decrease scarring from acne. 3. What diet changes should Billy make? Why? 4. What history (subjective) data do you need in order to treat Billy’s acne properly? 5. What are the goals of treatment for Billy? 6. What topical treatment is most appropriate for Billy? How does this topical treatment of acne work to decrease acne lesions? How long will it take for improvement after the topical treatment is started? 7. Describe the patient education and follow-up plan most appropriate for Billy. 8. Under what conditions should Billy be referred to a dermatologist for care? 9. What is the outcome criteria that you will use to evaluate Billy’s care? Acne Inversa (Hidradenitis Suppurativa) Lauren is a 19 yr old who presents with multiple swollen areas accompanied by black comedones in her right axillary region. She is frightened by the dramatic nature of the lesions and is having a lot of pain. Lauren is planning a week vacation on the beach later this month. 1. What can you tell Lauren about her condition that will help reduce her fear? This condition is caused by abscesses of the blocked hair follicles. Cause is unknown but there is a genetic influence. The average time for healing is about a week. 2. What will Lauren need to know to prepare her for the potential future with this condition? May reoccur in axillae, groin, perianal region, buttocks, chest, back and inframammary areas. Many cases disappear after age 35. 3. How will you examine Lauren to help determine the appropriate treatment and if she needs a referral? Unresponsive to oral therapy. 4. List the most common treatments for this condition. Topical, Oral and surgical therapy conservative management(2) o loose clothing o avoidance of heat, humidity, shaving, depilitation, deodorants o warm compresses o antibacterial soaps (dynamed) 5. Which treatments above can you prescribe in the primary care setting and which ones will you need to refer to a dermatologist? Surgical and laser therapy and recurrent lesion should be referred to dermatologist. 6. What will Lauren need to know about her potential treatment even if it is with the dermatologist and her planned vacation. Some treatment cause sun sensitivity. Seborrheic Dermatitis Robert, age 48, presents to clinic today with an exacerbation of seborrheic dermatitis. 1. What is seborrheic dermatitis and what is the cause? 2. What history and physical examination will need to be done in order to arrive at the diagnosis of seborrheic dermatitis? 3. How will you treat Robert's skin problem? 4. Health teaching for Robert would include prevention of outbreaks. What can be done to prevent exacerbations? Dry skin Sally, age 40, suffers from dry skin. Describe how you will manage her skin care, including patient education. Advise to keep room temp as close to 68° as possible to keep skin from drying. Use of humidifiers, bath water should be warm but not hot, apply moisturizer immediately after drying and use mild soap or cleansers sparingly. Air travel can remove moisture from skin. Pt will need to keep hydrated and use moisturizer. Eat a well balanced diet, add nutritional supplement if needed, exercise, get adequate rest. Avoid scratching and use cortisone cream ( for no more than one week) for itching. Acne Rosacea Judith is a 45 year old woman with a reddened face and scattered telangiectasia. She flushes easily and has developed some pustules around her nose. Her systems worsened after a cruise to Cozemel. 1. 2. 3. 4. What is the cause of acne rosacea? Who are the people most likely to be affected? What are the subjective and objective data needed to make a diagnoses of acne rosacea? How is acne rosacea treated? Include education to help prevent exaccerbations. When should these patients be referred? Warts David, age 20, has a wart on his thumb and small finger. 1. What is the causative agent of the wart? HPV 1 or HPV 4 2. How will you treat the warts? Include patient education in your discussion. Education: Most warts are benign, viral lesions that spread from person to person particularly in showers, locker rooms and other public places. May resolve spontaneously although it may take years. Educate on self treatment and side effects to all meds as well as instructions on soaking and paring the wart before application of medications, and proper use of OTC treatments. Make take multiple treatments to resolve. In office treatment should be down if The patient desires therapy The presence of pain, bleeding, itching and burning Lesions that are disabling or disfiguring Large numbers or size of lesions Prevention of spreading to unblemished skin An immuno-compromised state. In office options Chemical distruction Cryotherapy Electrodesiccation Laser ablation Contact Dermatitis LS is a 21 year old, African-American female who works as a cashier at McDonald’s. She complains of a rash on her hands for two weeks that her supervisor finds offensive. The rash itches and occasionally burns. She started using a new soap to clean counters at work about 3 weeks ago. Past history is significant for dry skin that she has treated with moisturizers and cortisone cream. The rash is on the palmar surface of her hands and on all her fingers, irregularly distributed in scaly, maculopapular erythematous patches. The nails are spared. 1. What history and examination are needed? 2. Outline the appropriate management. (She has no insurance and no prescription card. How will this affect your prescribing?) 3. What education should be provided? Would her cultural/socioeconomic background influence this education? How? 4. Her boss is refusing to let her work because he thinks she is infectious. LS asks for a work excuse. What do you do? 5. What is the plan for follow-up for LS? The Heartbreak of Psoriasis Beth is a 25 year old graduate student who just finished her oral comprehensive examination. She comes to clinic because of an exacerbation of her psoriasis. She was diagnosed when she was 21 years old. “Mother has it, too.” Beth has characteristic lesions on her elbows, knees, scalp and intergluteal cleft. 1. What are the usual nail dystrophies associated with psoriasis? Onycholysis (spooning) and hyperkeratosis (thickening) 2. What are the best medications for Beth today for her skin and her scalp? A solution to remove scale containing salicylic acid (3%) to be massaged into the scalp and left on for several hours or at night. And then an appropriate shampoo for dial use. Topical corticosteroids applied 2-3 times a day for 2-3 weeks. 3. Describe the education needed about the use and potential side effects of this treatment. What are the potential consequences of prolonged use of high potency steroids on Beth’s skin lesions? Skin atrophy with glucocorticosteroid use with an occlusive wrap can hasten the therapy of large or thick plaques. 4. Why should Beth avoid sunburn during her trip to Hawaii to celebrate graduation? Wear protective clothing and sunscreen d/t photosensitivity caused by treatment. Malignant skin lesions Lem G. is a 66 year old fair skinned farmer who frequently works outside without a hat. He is concerned about two spots on his face that have been there about three months and seem to be enlarging. One lesion is a ½ x 1 cm, discrete brown plaque that appears to be stuck on. The second is a round ½ cm lesion on the side of his nose with a raised center, pearly border, and distinct margin. It has a couple of small, non-blanching blood vessels in it. 1. Review chapter 47 Screening for skin cancer. 2. What are possible diagnoses for Lem? Rationale? 3. Outline your management plan (diagnostics, therapeutic/treatment, education, consultation/referral, follow-up). 4. What is actinic keratosis? Is it considered malignant? 5. What are the ABCDEs of assessing skin cancer?