Acute periapical abscess
advertisement

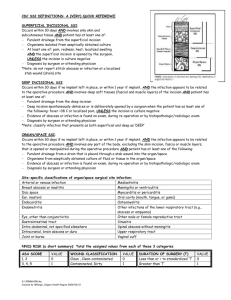
MINISTRY of PUBLIC HEALTH of UKRAINE VINNITSYA NATIONAL PIROGOV MEMORIAL MEDICAL UNIVERSITY It is "confirmed" on a methodical meeting of department of pediatric dentistry head-chair doc.Filimonov Yu.V. ____" _____________________ " Methodical recommendation for 4d year students of dental faculty Educational discipline Module ¹ Rich in content module ¹ Topic Course Faculty Autor Pediatric surgery 1 1 1 1 O Odontogenic and nonodontogenic periostitis 4 IV Stomatological Isakova N.M. Vinnitsya 2012 Actuality of theme: 1. Concrete aims: Periostitis is a disease which is characterized by distribution of inflammatory process on a periosteum to the sprout and body of jaw from a odontodenic or nonodontogenic cell. Patients with odon periostitis of jaws fold 3,3% from all children which call to surgeon-stomatology. Surgeon-stomatology must in good time diagnose this disease of MFA and conduct necessary treatment depending on the type of periostitis for children for prevention of complications. 3.Educator aims: To develop sense of professional responsibility for the timeliness of diagnostics of periostitis jaws in children and rightness of determination of medical tactics of doctor-stomatology. 3 Base knowledges, abilities, habits which are necessary for study the topic. Names of previous disciplines Skills are got 1. General anatomy The structure of the maxillofacial region, the blood and nerve supply 2. Gistology Histological structure of the oral mucous cavity. The mechanism of development and phase of inflammation 3. Therapy, pediatrics Know the features of a child's body. Know the basic diseases of importance in conducting the diagnosis of major dental diseases 4.Task for independent work during preparation to employment. 4.1. List of basic terms, parameters, descriptions which a student must master at preparation to employment : Term Determination 1. Acute periostitis Is acute purulent inflammation of the periosteum of the alveolar processes and bodyof the jaw 2 Chronic periostitis Excessive formation of periosteal stack layering, which are to be removed surgically due to indications 3. Granulomatous periodontitis Formed on the area of the root apex granulomais detected only radiographically. 4.2. Theoretical questions to employment: 1. Able to diagnose sharp serous and purulent periostitis of jaws for children and define medical tactics them. 2. Able to conduct differential diagnostics of sharp periostitis jaws for children with tumours and inflammatory diseases of jaws on the stage of intensifying. 3. Able to conduct differential diagnostics of chronic periostitis jaws for children with tumours and inflammatory diseases of jaws. 4.3 Practical works (tasks) To conduct the different types of the local anaesthetizing on phantoms. 5. A plan and organizational structure of lesson in discipline. № Stages of Distribution employment of time Preparatory stage 15 min he organizational questions. 1.2 Forming of motivation. 1.3 Control of initial level of preparation. 2.stag Basic 55 min 3. inal stage 3.1. 3.2. 20 min Control of eventual level of preparation. General estimation of studing activity of student. Types of control practical tasks, situatioonal tasks, verbal crossexamination at standart list of questions. test tasks Facilities of studies Text-books, methodical recommendations. 3.3 Informing of students about the theme of next employment. Maintenance of theme Infections of orofacial and neck region, particularly those of odontogenic origin, have been one of the most common diseases in human beings. Despite great advances in health care, these infections remain a major problem; quite often faced by oral and maxillofacial surgeons. These infections range from periapical abscess to superficial and deep neck infections. The infections generally spread by following the path of least resistance through connective tissue and along fascial planes. The infections spread to such an extent, distant from the site of origin, causing considerable morbidity and occasional death. Early recognition of orofacial infection and prompt, appropriate therapy is absolutely essential. A thorough knowledge of anatomy of the face and neck is necessary to predict pathways of spread of these infections and to drain these spaces adequately. This chapter deals with various types of orofacial and neck infections, with necessary description of numerous fascial spaces; with special reference to their involvement, surgical anatomy, clinical features, principles of their management with the surgical techniques used for drainage or decompression of the infections by intraoral or extraoral routes, and finally modes of their spread and the complications that would be encountered if these cases are left untreated, are also discussed. ETIOLOGY Infections in the orofacial and neck region usually originate from following sources: A. General classification It is based on the origin of the infection. 1. Odontogenic The majority of infections in orofacial and neck region belong to this group. Odontogenic infections arise within jaw bones, and can be classified as those arising from: (i) Pulp disease, (ii) Periodontal disease, (iii) Secondarily infected cysts or odontomes, (iv) Remaining root fragment, (v) Residual infection, and (vi) Pericoronal infection. These manifest in the following forms: (i) Periapical abscess, (ii) Periodontal abscess, (iii) Infected cyst, (iv) Residual abscess, and (v) Pericoronal abscess. 2. Traumatic Occasionally, trauma from penetrating wounds of soft and hard tissues of the face can lead to orofacial infection. 3. Implant surgery 4. Reconstructive surgery. 5. Infections arising from contaminated needle punctures. 6. Others This group includes instances of orofacial infections arising from other factors such as infected antrum, salivary gland afflictions etc. 7. Secondary to oral malignancies B. On the basis of causative organisms Orofacial infections can be classified as:— 1. Bacterial infections (a) The odontogenic infections encountered in orofacial region are mostly bacterial infections, (b) Non-odontogenic infections: (i) Tonsillar, and (ii) Nasal infections which are more common in children, and (iii) Furuncle of overlying skin. 2. Fungal infections These infections have slow rate of spread. These are difficult to diagnose in early stages. 3. Viral infections The literature does not show sufficient reports about these conditions of odontogenic origin. Irrespective of the original source of infection, once it has been established within the soft tissues, its further spread tends to occur in uniform fashion. PATHWAYS OF ODONTOGENIC INFECTION Serious dental infection, spreading beyond the tooth socket, is more common due to thepulpal infection than the periodontal infection. Invasion of the dental pulp by bacteria after decay of a tooth Inflammation, edema and lack of collateral blood supply Venous congestion or avascular necrosis (pulpal tissue death) Reservoir for bacterial growth (anaerobic) і Periodic egress of bacteria into surrounding alveolar bone I The periapical infection progress can vary according to the following: i. The number and virulence of the organism. ii. Host resistance. iii. Anatomy of the involved area. Odontogenic Infections Types of infection: A. Acute, and B. Chronic Acute Stage In the acute stage, the infection spreading in the soft tissues can take the following forms in the clinical situations: (i) Abscess, (ii) cellulitis, and (iii) fulminating infections. 1. Abscess is a circumscribed collection of pus in a pathological tissue space. A true abscess is a thick-walled cavity containing pus. The suppurative infections are characteristic of staphylococci, often with anaerobes, such as Bacteroides, and are usually associated with large accumulation of pus, which require immediate drainage. These microorganisms produce coagulase, an enzyme, that may cause fibrin deposition in citrated or oxalated blood. 2. Cellulitis is spreading infection of loose connective tissues. It is a diffuse, erythematous, mucosal or cutaneous infection. It is characteristically the result of streptococci infection; and does not normally result in large accumulation of pus. Streptococci produce enzymes such as streptokinase (fibrinolysin), hyaluronidase, and streptodornase. These enzymes breakdown fibrin and connective tissue ground substance and lyse cellular debris, thus facilitate rapid spread of bacteria along the tissue planes. Antibiotics may arrest the spread of infection; and may bring about complete resolution of the condition. However, in cases refractory to antibiotic coverage, pus pockets should be suspected; and in such cases, exploration and drainage should be done. 3. Fulminating infections of the various spaces in the orofacial region: Here, the infection involves the secondary spaces involving vital structures, along the pathway of least resistance. Acute Infection The odontogenic abscesses present in the following forms: a. Acute periapical abscess An odontogenic abscess usually arises and remains in the confines of alveolar bone. This is referred to as acute periapical abscess. b. Acute dentoalveolar abscess Once the infection has crossed the confines of alveolar bone and comes to lie in the neighbouring soft tissues, and if it gets localized, it is referred to as acute dentoalveolar abscess. c. Acute periodontal abscess d. Acute pericoronal abscess The infection follows the path of least resistance. The important and the deciding factor, in the involvement of the fascial spaces, is the relationship of root apices of molars with the mylohyoid line. The abscess related to mandibular second and third molars, usually, perforates the lingual cortex and spreads to the submandibular space; as the root apices of these teeth lie below the mylohyoid line. The abscess related to premolars and first molars, involves the sublingual space, as the root apices of these teeth are situated above the mylohyoid line. Acute Periapical Abscess Etiology The main cause is infective necrosis of pulp. Causes of infective necrosis of pulp include: (i) carious involvement, (ii) contamination of traumatic exposure of pulp, (iii) sterile necrosis, where apical vessels are torn by blow on the teeth, or (iv) following inadvertent chemical or thermal damage to pulp. Micro-organisms from infected pulp invade periapical tissues. The entry to periapical tissues is gained usually through (i) apical foramina; and in such circumstances, the infection is truly periapical, Occasionally, the entry is through (ii) accessory canals, (iii) an endodontic perforation, (iv) an opening in the floor of the pulp chamber of a primary molar, (v) from an area of surface resorption, or (vi) root fracture. In these circumstances, the abscess develops on the lateral aspect of root or at the root furcation or in the vicinity of root fracture, as the case may be. Clinical features Severe throbbing pain in the affected tooth. The offending tooth may show carious involvement, and may be sensitive to percussion. Mobility may or may not be present. Radiographic presentation The involved tooth shows carious lesion with periapical pathology, root fracture, erosion or absorption as the case may be. It also shows periapical radiolucency, areas of resorption; and the different types of radiolucencies involving the root fractures. Treatment The treatment modalities comprise of the following: (i) antibiotics, (ii) analgesics, (iii) drainage through the pulp chamber, (iv) extraction of the offending tooth, or (v) endodontic treatment. Acute Dentoalveolar Abscess Etiology This disease entity is a continuation of periapical abscess. Clinical features 1. Pain The severity of pain depends upon the stage of the disease process. 2. Submucosal swelling in the sulcus, usually on the outer aspect of alveolar process. Fluctuation may be elicited after few days. If left untreated, the swelling bursts and produces sinus tract discharging pus. Radiographic presentation There is no appreciable difference in the presentation of the two entities radiographically, except that the area of radiolucency may be more marked in dentoalveolar abscess. Treatment The same treatment modalities hold true for dentoalveolar abscess. In addition, intra- or extraoral incision and drainage may be required. Acute Periodontal Abscess Etiology It arises in periodontal membrane adjacent to a periodontal pocket. Clinical features Dull pain, rarely severe, and variable in intensity. Pus discharges via gingival pocket. It may produce a sinus on either inner or outer aspect of alveolar process; and rarely tracks through the skin. Periodontal abscesses are uncommon in children and an acute swelling close to gingival margin of a primary molar is usually a periapical abscess. SurgicalTherapy SurgicalTechnique for Incision and Drainage of an Abscess Incision and drainage helps the following: i. to get rid of toxic purulent material ii. to decompress the edematous tissues iii. to allow better perfusion antibiotic and defensive elements iv. to increase oxygenation of the infected area. of blood, containing Hilton's Method of Incision and Drainage The method of opening an abscess ensures that no blood vessel or nerve in the vicinity is damaged and is called Hilton's method. Steps 1. Topical anaesthesia is achieved with the help of ethyl chloride spray. 2. Stab incision: made over point of maximum fluctuation in the most dependent area along the skin creases, through skin and subcutaneous tissue. 3. If pus is not encountered, further deepening of surgical site is achieved with sinus forceps (to avoid damage to vital structures). 4. Closed forceps—are pushed through the tough deep fascia and advanced towards the pus collection. 5. Abscess cavity is entered and forceps opened in a direction parallel to vital structures. 6. Pus flows along sides of the beaks. 7. Explore the entire cavity for additional loculi. 8. Placement of drain—a soft yeat's or corrugated rubber drain is inserted into the depth of the abscess cavity; and external part is secured to the wound margin with the help of suture 9. Drain left for at least 24 hours. 10. Dressing—is applied over the site of incision taken extraorally without pressure. Purpose of keeping the drain The purpose of drain is to allow the discharge of tissue fluids and pus from the wound by keeping it patent. The drain allows for debridement of the abscess cavity by irrigation. Tissue fluids flow along the external surface of a latex drain. Hence, it is not always necessary to make perforations in the drain, which could weaken and perhaps cause fragmentation within the tissues. Removal of drains Drains should be removed when the drainage has nearly completely ceased. Drains have shown to allow ingress of skin flora along their surfaces. Some forms of drain, such as latex drains in particular, are irritating to the surrounding tissues and may stimulate some exudates formation on their own. Thus, drains are usually left in infected wounds for 2-7 days (Flynn 2000). Literature. Basic: 1.Lectures which are read on the department of pediatric dentistry. 2. Pinkham J.R. Pediatric dentistry. – 2nded.- W.B. Sounders Company. – 1994.- 647 p. 3. Pediatric dentistry /Ed. R.R.Welbury.- Oxford, 1997 – 584p. Additional: 1. Шаргородский А.Г. Клиника, диагностика, лечение и профилактика воспалительных процессов челюстно-лицевой области. - Свердловск, 1987. - 305 с. 2. Хирургическая стоматология.: Учебник /Т.Г.Робустовой. - М.: Medicine, 1990, 327. 3. Стоматология детского возраста: Учебник / А.А.Колесова. - М.: Medicine, 1991. 4. Танфильев Д.Е. Удаление зубов. - Л.: Medicine. 1976. - 160 с. 5. Соловьев М. М., Игнатов Ю.Д., Конобевцев О. Ф. Обезболивание at лечении зубов in детей. - М.: Medicine, 1985. - 184 с. 6. Рузин Г.П., Бурых М. М. Основы технологии операций в хирургической стоматологии и челюстно-лицевой хирургии. - Харьков, 2000. - 291 с.