Pediatric History Form - Integrative Pediatrics Of Olney
advertisement

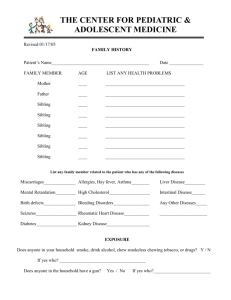
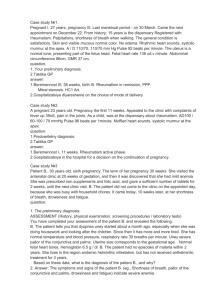
Integrative Pediatrics of Olney HISTORY Birth History Name: _______________________________Birth Date: ____________Time:___________________ Birth Wt.: ______________Length:_______________Head circumference: _____________________ Number of week’s (of Pregnancy):______________Type of Delivery: _________________________ Any problems during labor or delivery: __________________________________________________ Any issues during Nursery the stay: ____________________________________________________ Jaundice (Y / N) -If YES; Rx: ___________________Discharge weight (on date):________________ Vaccines given (Date):________Hearing screen (Date): ________Newborn screening (Date) _______ Breast/ Formula: _____________Feeding Problems: ___________________Colic:_______________ Mother's Pregnancy History Age: _________Name of Obstetrician: _________________________ Mom's Blood Type__________ Anemia: ________________Antibiotic use: ______________________________________________ BP: _____________Gestational diabetes: ______________Emergencies:______________________ Preterm labor (# of weeks of Gestation, Treatment given, How long):__________________________ Surgery: ________________Smoking:__________________Hep B Status (neg/pos):_____________ Alcohol: ______________Drugs:_________________Second Hand Smoke: ___________________ Vaccinations: _______________________HPV / HERPES (Y/N) - if Yes, Rx: ____________________ Any other problems during Pregnancy OR Labor: _________________________________________ Prenatal Vitamins: ____________________Other supplements taken: _________________________ Child's Milestones (Approximate Age in months) Motor Head steady:_________________Rolled over:__________________Sat up:___________________ Sat up without support:_____________Crawled:_____________Stood with support:_____________ Walked:______________________________Pointing:_____________________________________ Verbalization Cooing:_________Blabbering:_________Single word/s:________2-3 word Phrases:_____________ Toilet Trained:_____________________________________________________________________ Does your child have problems with? Sleep:________________Nightmares:____________________Bed Wetting:___________________ Nail Biting:_________________ Anger:____________________Anxiety:______________________ Patient Name: Medical History ALLERGIES: Environmental:______________________Food /s:____________________________ Age at Diagnosis:_____________Medications:_________________ER visits: __________________ ASTHMA:______________Age at Diagnosis:_________Medications:_________________________ Admission to Hospital:__________________ER visit/s( with Dates):__________________________ Pulmonologist (Name & Hospital):_____________________________________________________ ADD/ ADHD:________Age at Diagnosis:________Medication/s:_____________________________ Why medicine stopped or changed:____________________________________________________ SPEECH Problems: __________ Age at Diagnosis:__________Speech therapy:________________ HEARING Problems: __________________Treatment:____________________________________ VISION Problems: ___________________Treatment:______________________________________ INJURIES/FRACTURES:__________Which Part:________Age:______Treatment/ surgery:________ DIET:____________________________________________________________________________ Vitamins/ Supplements taken regularly: _________________________________________________ _________________________________________________________________________________ SURGERIES (Date/ Age) ____________________________________________________________: IMMUNIZATIONS (Up TO Date/ NOT):_________Which one/s Missing or Pending:______________ Exposure to SECOND HANDSMOKE:_________________________________________________ PETS at home:____________________________________________________________________ DAYCARE/ BABYSITTER:__________________First Started:____________Hours/week:________ DENTIST: ________________________________________________________________________ Last Visit:___________Any Problems:__________________________________________________ SCHOOL:________________________________________________Grade:__________________ EXERCISE/ SPORT:_______________________________________________________________ ALLERGY TO MEDICATIONS: ________________________________________________________ REACTION/MANIFESTATION: ________________________________________________________ SIBLINGS: # 1 2 3 Name Age/ DOB Medical History Intervention 4 Patient Name: Family History Condition Asthma Allergies ADD/ ADHD Heart Disease Behavioral Problems/ Depression High Cholesterol/ Heart Attack High Blood Pressure Cancer (which organ) Diabetes Kidney Disease Language Deficits Rheumatoid Arthritis or Lupus Surgery Thyroid Problems Vision Deficit Smoking Alcohol Drugs STD's/ HIV Hep B/ Hep C Hearing/ Speech Deficits Age Mother MGM MGF Father PGM PGF Patient Name: Mother's Siblings Significant History Age at Diagnosis Intervention 1 2 3 4 Father's Siblings Significant History Age at Diagnosis Intervention 1 2 3 4 Developmental Delay in any (Extended) Family member: Diagnosis:________________Age at Diagnosis:_________Current Treatment:_________________ DECLARATION I, ___________________________________(Mother/Father), certify that the information that I have supplied is correct and accurate to the best of my knowledge. SIGNATURE: _____________________________________________________________________ DATE: ___________________________________________________________________________