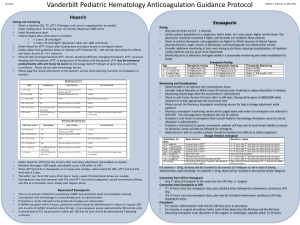
Table 3. Anti-Factor Xa and Enoxaparin Dosing Results

From
The Annals of Pharmacotherapy
Implementation of an Enoxaparin Protocol For Venous
Thromboembolism Prophylaxis in Obese Surgical Intensive
Care Unit Patients
Kyle P Ludwig PharmD BCPS; Heidi J Simons PharmD BCPS; Mary Mone RN BSE; Richard G Barton MD;
Edward J Kimball MD
Posted: 11/09/2011; The Annals of Pharmacotherapy. 2011;45(11):1356-
1362. © 2011 Harvey Whitney
Books Company
Abstract and Introduction
Abstract
BACKGROUND: Venous thromboembolism (VTE) is a serious health care issue that affects a large number of people. Few standards exist for delineating the optimal dosing strategy for VTE prevention in obese patients, especially in the setting of major surgery or trauma.
OBJECTIVE: To document the efficacy of a surgical intensive care unit (SICU)- specific, weight-based dosing protocol of enoxaparin 0.5 mg/kg given subcutaneously every 12 hours for VTE prophylaxis in morbidly obese (defined as body mass index [BMI] ≥35 kg/m
2 or weight ≥150 kg) SICU patients, using peak antifactor Xa levels to determine therapeutic endpoints.
METHODS: Data were collected retrospectively in an academic, university-based SICU on 23 morbidly obese patients who received weight-based enoxaparin for VTE prophylaxis from December 1, 2008, through June 30, 2010.
RESULTS: A weight-based dosage range of enoxaparin 50 –120 mg twice daily (median 60) was given to 23 patients. The mean BMI was 46.4 kg/m 2 . The initial mean anti-factor Xa level (measured after the third dose) was 0.34 IU/mL (range 0.20
–0.59). Patients received an average of 18 doses. Two cases required an increase or decrease in dosage based on anti-factor Xa levels. Morbidity related to this dosing included a single event of minor endotracheal bleeding and a single deep vein thrombosis that was likely present prior to treatment.
CONCLUSIONS: Weight-based dosing with enoxaparin in morbidly obese SICU patients was effective in achieving anti-factor Xa levels within the appropriate prophylactic range. This regimen reduced the rate of VTE below expected levels and no additional adverse effects were reported.
Introduction
Venous thromboembolism (VTE) is a serious health care issue that affects 10
–60% of hospitalized patients.
[1] Current evidence-based literature indicates that VTE is also one of the most preventable complications related to hospitalization.
[1] Practice guidelines for prevention of VTE have been available since 1986, along with a large body of data providing evidence that prevention saves lives. Considered the second most prevalent hospital complication, VTE contributes to increased length of stay and costs, as well as increased rates of morbidity and mortality.
[1]
The 2008 American College of Chest Physicians (ACCP) guidelines for prevention of VTE note that
"almost all hospitalized patients have at least one risk factor for VTE, and approximately 40% have three or more risk factors." [2,3] High-risk conditions include cancer, trauma, history of VTE, and major orthopedic procedures. Standards for preventive treatment can include medications as well as strategies that range from noninvasive venous compression equipment to percutaneously placed inferior vena cava filters.
Obesity has become an epidemic, and this medical condition has complicated virtually every aspect of health care.
[4
–8] Significant financial and medical resources are directed toward obesity prevention as well as the treatment of related complications. Approximately 69,000 patients received bariatric surgery in the
US in 2002; in this population, the incidence of VTE was 3.4 per 1000 discharges.
[9] Surprisingly, this incidence is lower than the rate of VTE after all surgical discharges, which is 9.6 per 1000 discharges. In another study, pulmonary embolism (PE) was found within 30 days of surgery in only 1 of 2000 consecutive outpatient gastric bypass procedures for obesity.
[10]
Few standards exist for delineating the optimal dosing strategy for VTE prevention in obese patients, especially in the setting of major surgery or trauma. Nearly all of the studies that have evaluated VTE prophylaxis with primary respect to the risk posed by obesity are focused in the bariatric surgery population.
[11
–13] The 2008 ACCP guidelines note that the "optimal regimen, dosage, timing, and duration of thromboprophylaxis in bariatric surgery patients is unknown." [1] These guidelines further suggest that normal doses may not be adequate in this population and that higher than standard doses should be used (Grade 2C recommendation).
[1] Based on this ACCP practice guideline, our surgical intensive care unit (SICU) made weight-based dosing of low-molecularweight heparin (LMWH) in the morbidly obese patient, defined as a body mass index (BMI) of greater than or equal to 35 kg/m 2 or weight greater than or equal to 150 kg, the unit standard of care in 2008 for those without contraindications to use.
We retrospectively collected data on this patient population in our SICU to document the results of weight-based dosing for VTE prophylaxis using anti-factor Xa levels as markers for our primary outcome.
Methods
On admission to our SICU, 28 critically ill adults (age ≥18 years) with a BMI greater than or equal to 35 kg/m 2 or weight greater than or equal to 150 kg were screened. Of those, 23 patients received weightbased VTE prophylaxis. Each patient was given enoxaparin 0.5 mg/kg subcutaneously twice daily based on actual body weight from December 2008 until June 2010. This was modeled on the data derived by
Borkgren-Okonek and colleagues.
[13] The enoxaparin dosages used in that study were approximately 0.5 mg/kg twice daily. In support of this standard dosing, several studies have demonstrated that twice-daily dosing of enoxaparin, rather than single daily administration, achieves a more consistent anti-factor Xa level over a 24- hour period in the hyperdynamic trauma population.
[14,15] These authors suggest an appropriate prophylactic reference range for enoxaparin of 0.2
–0.5 IU/mL. If levels were out of range, the dose of enoxaparin was adjusted by 10 mg, based on the Borkgren-Okonek and colleagues study, as well as for ease of administration.
[13]
Exclusion criteria for VTE prophylaxis included coagulopathy, bleeding disorder, spinal epidural hematoma, hepatic failure, platelets less than or equal to 100×10
3 /
μL, estimated creatinine clearance less than or equal to 30 mL/min (based on Cockcroft-Gault equations using adjusted body weight), serum creatinine greater than or equal to 1.6 mg/dL, pregnancy, and/or HIV/AIDS. Additional thromboprophylaxis interventions included routine sequential compression devices, physical therapy, and ambulation as soon as medically cleared. Placement of inferior vena cava filters was permitted as requested by the primary physician. This data collection study was approved by the Institutional Review
Board at the University of Utah Hospital.
The primary objective was to document the results of a unit-specific, weight-based dosing protocol using anti-factor Xa levels as therapeutic endpoints (goal anti-factor Xa levels 0.2
–0.5 IU/mL).
[13,16,17] Secondary endpoints included the rate of deep vein thrombosis (DVT) and PE during the admission, safety as
assessed by rates of minor and major bleeds (definition of a major bleed is overt bleeding, bleeding with anemia associated with a ≥2-mg/dL decrease in hemoglobin from baseline, or bleeding requiring operation or transfusion), and the incidence of heparin-induced thrombocytopenia (HIT) in this same population during hospitalization and at 30 days after discharge.
[9]
Baseline clinical and demographic data were obtained for treated patients. These data included basic metabolic panel, complete blood cell count, age, sex, BMI, VTE risk factors, hospital length of stay, ICU and hospital mortality, and total blood transfusions. The dosage of enoxaparin had been calculated based on SICU admission weight values and dosage was rounded to the nearest 10-mg value, with one exception in which the dosage was rounded to the nearest 5 mg. Doses were administered out of commercially available enoxaparin product syringes. Peak anti-factor Xa levels were obtained through a venipuncture sample approximately 4
–6 hours after the third or fourth dose, based on nursing and/or patient convenience, and evaluated at our national reference laboratory (Associated Regional and
University Pathologists, www.arup.com
).
[17] Blood samples were transported to the laboratory, where they were centrifuged and then assayed according to standard protocols using chromogenic inhibition of factor Xa. The Rotachrom assay using the STA-Compact instrument (Diagnostic Stago, Parsippany, NJ) was used for quantitative activity for enoxaparin. Our laboratory at the University of Utah Hospital reports only levels greater than 0.2 IU/mL, as the precision of the assay below 0.2 IU/mL has not been established. The unit protocol directed that if the initial anti-factor Xa level was in the acceptable prophylactic range (0.2
–0.5 IU/mL), the calculated drug dosage was continued until SICU discharge.
Follow-up levels were not measured unless the patient experienced a change in renal function or health status, or by physician request. If the initial level was not within the defined range, the dose was adjusted by 10 mg, and a follow-up level was checked within 4 hours after the third or fourth dose of the new dosage regimen (Figure 1).
[13] When patients were transferred from the SICU, dosage was transitioned to a fixed dosage of either 30 or 40 mg subcutaneously twice daily because of resolving hyperdynamic drug clearance and reduced VTE risk factors.
[18,19]
Figure 1. Flow chart of unit protocol algorithm. BMI = body mass index; SICU = surgical intensive care unit.
Adverse events were recorded, and included symptomatic VTE during SICU and hospital admission, major and/or minor bleeding events, and incidence of HIT. Readmission to the same institution for any bleeding or clotting event within 30 days of discharge was also recorded. Daily monitoring included standard laboratory values (eg, hemoglobin, hematocrit, platelet count, serum creatinine) as required based on individual patients' needs.
All descriptive statistics were used as appropriate for nominal and ordinal data. These included mean, standard deviation, range, percentage, and count. Statistics were calculated using Microsoft Excel
(Microsoft Office 2003, Microsoft Corp., Redmond, WA).
Results
Between December 1, 2008, and June 30, 2010, 23 patients met the eligibility criteria for use of the standard unit protocol for dosage calculations for morbidly obese patients. Of the 23 patients, 13 (57%) were female, the mean age was 45.6 years, the mean BMI was 46.4 kg/m 2 (range 36
–77), and mean weight was 137 kg (range 97 –267). Fourteen of the 23 (61%) patients were admitted for injuries associated with trauma, and the remaining 9 were admitted for either general or vascular surgery (Table
1). All VTE risk factors were recorded and are presented in Table 2. The majority of the patients had at least 3 risk factors documented for VTE. The median calculated twicedaily dose of enoxaparin was 60 mg (range 50 –120).
Table 1. Patient Characteristics and Admission Outcome Data
Characteristic
Age (y), mean (SD)
Sex, n (%) female male
Weight (kg), mean (SD)
Body mass index (kg/m 2 ), mean (SD)
35
–45 (n = 16)
46 –55 (n = 3)
>55 (n = 4)
ICU length of stay (days), mean (SD)
Ventilator time (hours), mean (SD)
Hospital length of stay (days), mean (SD)
45.6 (15.65) (range 18 –71)
13 (57)
Data
10 (43)
136.7 (37.10) (range 97
–267)
46.4 (11.69) (range 36 –77)
9.1 (8.80) (range 0.8
–33)
176.5 (216.59) (range 0
–803)
15.8 (9.40) (range 4
–39)
Admission surgery service, n (%) trauma 14 (61) general 8 (35) vascular 1 (4)
Transfusion ≥6 units during total hospital stay, n (%) 2 (9)
Table 2. Venous Thromboembolism Risk Factors in Study Population
Risk Factor n (%)
Major surgery of abdomen, pelvis, or lower extremity 22 (96)
Major trauma of pelvis, hip, or lower extremity 15 (65)
Age >40 years 16 (70)
Prolonged immobility, lower extremity paresis
Cardiac or pulmonary failure
Cancer diagnosis/treatment
Inflammatory bowel disease
Recent smoking history
4 (17)
2 (8.7)
2 (8.7)
2 (8.7)
1 (4.3)
The primary outcome (anti-factor Xa level between 0.2 and 0.5 IU/mL) was achieved in 91% of patients
(21 of 23) at the initial time tested. The mean anti-factor Xa level was 0.34 IU/mL (range 0.20
–0.59) at the initial measurement (Figure 2). The overall number of anti-factor Xa levels measured from the study participants is outlined in Table 3. Two patients received 3 additional follow-up anti-factor Xa level measurements during SICU admission; both admissions were longer than 28 days. During this time, both patients had status changes and surgical procedures requiring confirmation of the anti-factor Xa level.
Table 3. Anti-Factor Xa and Enoxaparin Dosing Results
Enoxaparin per dose (mg), mean (SD) 66 (15.89) (range 50 –120)
Initial anti-factor Xa levels (IU/mL), a mean (SD) 0.34 (0.12) (range 0.20
–0.59)
Total patient doses (n), mean (SD) 18 (3) (range 4
–57) a Obtained after 3rd or 4th protocol calculated dose.
Figure 2. Initial anti-factor Xa levels after first dosage cycle (bold lines are suggested range for appropriate prophylaxis).
Of the 2 patients who required dosing adjustments, both adjustments were decreases. The first case was a female with a unit admission weight of 113 kg and a BMI of 47 kg/m 2 who had an anti-factor Xa level of
0.59 IU/mL after the third protocol calculated enoxaparin dose of 50 mg. The dosage was decreased to
40 mg subcutaneously twice daily and a follow-up anti-factor Xa measurement was ordered for after the third dosage. The patient was discharged to a long-term care facility before the level was measured. The second patient was a female with an admission weight of 180 kg and a BMI of 72 kg/m 2 who had an antifactor Xa level of 0.55 IU/mL after the fourth dose of enoxaparin 90 mg. The dosage was decreased to
80 mg subcutaneously twice daily and the follow-up anti-factor Xa level was 0.5 IU/mL. This dosing regimen was continued for another 6 days until the patient transferred to a step-down unit.
One male patient was diagnosed as having a lower extremity DVT. This patient had an initial anti-factor
Xa level of 0.38 IU/mL while on 70 mg of enoxaparin. On review of this case, this patient may have had a preexisting DVT, but the choice was made to treat him until a definitive diagnosis of DVT could be made.
The patient was transferred from an outside facility and had a swollen extremity on admission. A venous duplex ultrasound was ordered but not performed until the following day, at which time confirmation of a
DVT was made and treatment was adjusted. The patient experienced no consequence as a result of the
protocol treatment. One patient had an episode of minor bleeding that occurred during endotracheal suctioning, for which no treatment was required, but enoxaparin was withheld for 2 doses and restarted.
There were no episodes of major bleeding or HIT (Table 4).
Table 4. Primary and Secondary Outcomes
Outcome n (%)
Primary
Therapeutic anti-factor Xa with initial level a 21 (91)
Secondary
VTE during admission
Bleeding event
1 (4.3) major 0 minor 1 (4.3)
HIT
ICU mortality
Hospital mortality
0
0
0
HIT = heparin-induced thrombocytopenia; ICU = intensive care unit;
VTE = venous thromboembolism. a Obtained after 3rd or 4th protocol calculated dose.
With regard to readmission within 30 days of discharge, 5 patients were readmitted but none were for reasons related to bleeding, clotting, or thrombosis. Although 2 patients required transfusions greater than 6 units during their hospital stays, the treating physicians did not think this was related to enoxaparin use.
Discussion
To date, the optimal dosing strategy for VTE prophylaxis in critically ill, morbidly obese patients has not been determined.
[20] These patients have generally been excluded from participation in traditional dosing trials, despite having an intrinsically higher risk for VTE. Unfortunately, clinicians are left to extrapolate data from the bariatric surgery literature due to the limited amount of data on critically ill patients.
Borkgren-Okonek and colleagues examined enoxaparin dosage for VTE prophylaxis in bariatric surgical patients undergoing either laparoscopic or open Roux-en-Y gastric bypass surgery using a BMI-stratified dosing regimen to analyze safety and efficacy.
[13] In this study, patients with a BMI less than or equal to
50 kg/m 2 (n = 124) were given subcutaneous enoxaparin 40 mg every 12 hours and patients with a BMI greater than 50 kg/m 2 (n = 99) were given 60 mg every 12 hours. Anti-factor Xa activity was measured in all patients 4 hours after the third dose of enoxaparin, and the target antifactor Xa range was 0.18
–0.44
IU/mL. Dose adjustments of 10-mg increments were made for levels outside this range. The mean steady-state anti-factor Xa level was 0.26 IU/mL in the 40-mg dose group and 0.32 IU/mL in the 60-mg dose group, with 79% and 69% of patient groups achieving the target levels, respectively. On discharge, patients were given a 10-day, single dose treatment plan that ranged from 30 to 80 mg (based on BMI), although nearly 90% of patients received the 40- to 60-mg dose. One patient in the 40-mg group experienced a DVT and PE during the follow-up period (postoperative day 37). This patient had achieved
the target anti-factor level during the early treatment phase, but subsequent testing revealed the diagnosis of hyperhomocysteinemia. Significant bleeding occurred in 2.2% (5/223) of patients, 4 of which required treatment with transfusion. The authors concluded that their BMI-stratified regimen provided efficacious therapy for prevention of VTE, achieved target range anti-factor Xa levels, and incurred minimal bleeding risks.
[13]
Simone and colleagues compared 2 different LMWH dosing regimens in 40 patients undergoing laparoscopic bariatric surgery.
[21] The dosages, determined prospectively based on surgeon preference, were either 40 or 60 mg subcutaneously twice daily. Anti-factor Xa levels were checked after the first and third dose, but the majority of patients did not receive a verification of the anti-factor Xa level after the third dose. The 60-mg group had better achievement of the target antifactor Xa concentrations at 0.26 ±
0.09 IU/mL, versus 0.17 ± 0.08 IU/mL in the 40-mg group (p < 0.005).
Rondina and colleagues conducted a study in 28 hospitalized medical patients with a BMI greater than or equal to 35 kg/m 2 ; patients received enoxaparin 0.5 mg/kg once daily for 2 consecutive days.
[22] Antifactor Xa levels were measured 4- 6 hours after the first or second dose. After patients received these 2 doses, the treating physician changed or continued therapy as deemed appropriate. Most enoxaparin regimens were decreased to a fixed dose of 40 mg subcutaneously once daily. The average peak antifactor Xa level was 0.25 IU/mL (range 0.08
–0.59). Adverse effects during this shortterm treatment were absent, with no VTE events, bleeding events, or significant thrombocytopenia documented. The authors concluded that a weight-based dosage of enoxaparin resulted in peak anti-factor Xa levels within or near the recommended range for thromboprophylaxis.
Limitations to our study include small sample size, lack of comparator group, and single-center experience. Although the use of anti-Xa levels as a surrogate marker for efficacy is widely used clinically, its overall utility is still being elucidated. However, no other laboratory standard is readily available with better clinical correlation. All doses were dispensed from commercially available product syringes, potentially leading to inaccuracy with administration. Our patient population was followed for only 30 days after discharge, which may have misrepresented VTE prevention in a longer-term setting. While the results of this study add to our understanding of anticoagulant dosing in obese, critically ill patients, they may not be generalizable to the entire obese population. ICU patients tend to be physiologically more hyperdynamic, have erratic subcutaneous absorption, and have massive shifts of fluid, which can make responses to dosing unpredictable.
[19,23,24]
Morbidly obese patients carry a high risk for VTE complications, especially those who have been critically injured or have undergone major surgery. Presently, there does not appear to be consensus on a weightbased dosing protocol for thromboprophylaxis in these patients, but it is clear that the standard dose regimen with an LMWH provides suboptimal anti-factor Xa levels, and, likely, suboptimal prophylaxis.
Current ACCP guidelines document that higher than standard doses or weight-based doses should be considered and this therapy should be monitored using anti-factor Xa levels.
Based on the results of our data collection, we found that weight-based dosing with enoxaparin 0.5 mg/kg in morbidly obese, critically ill patients was effective in achieving anti-factor Xa levels in the prophylactic range. In our patient population, this regimen had limited adverse events and the rate of
VTE was lower than that reported in the literature. Randomized, controlled trials in a specific subset of patients would verify the potential risks and benefits for weight-based dosing treatment.
References
1. Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American
College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest
2008;133:381S-453S. DOI 10.1378/chest.08
–0656
2. Edmonds MJ, Crichton TJ, Runciman WB, Pradhan M. Evidence-based risk factors for postoperative deep vein thrombosis. ANZ J Surg 2004; 74:1082
–97. DOI 10.1111/j.1445–
1433.2004.03258.x
3. Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation
2003;107:I9
–16
4. Caterson ID. Medical management of obesity and its complications. Ann Acad Med Singapore
2009;38:22 –7.
5. Diehl AM. Hepatic complications of obesity. Gastroenterol Clin North Am 2010;39:57
–68. DOI
10.1016/j.gtc.2009.12.001
6. Doyle SL, Lysaght J, Reynolds JV. Obesity and post-operative complications in patients undergoing non-bariatric surgery. Obes Rev 2010;11:875
–86. DOI 10.1111/j.1467–
789x.2009.00700.x
7. Leinum CJ, Dopp JM, Morgan BJ. Sleep-disordered breathing and obesity: pathophysiology, complications, and treatment. Nutr Clin Pract 2009;24:675 –87. DOI
10.1177/0884533609351532
8. James WP. WHO recognition of the global obesity epidemic. Int J Obes (Lond) 2008;32(suppl
7):S120
–6. DOI 10.1038/ijo.2008.247
9. Poulose BK, Griffin MR, Zhu Y, et al. National analysis of adverse patient safety for events in bariatric surgery. Am Surg 2005;71:406
–13.
10. McCarty TM, Arnold DT, Lamont JP, Fisher TL, Kuhn JA. Optimizing outcomes in bariatric surgery: outpatient laparoscopic gastric bypass. Ann Surg 2005;242:494
–8; discussion 498–
501.
11. Scholten DJ, Hoedema RM, Scholten SE. A comparison of two different prophylactic dose regimens of low molecular weight heparin in bariatric surgery. Obes Surg 2002;12:19
–24. DOI
10.1381/096089203231144522
12. Hamad GG, Choban PS. Enoxaparin for thromboprophylaxis in morbidly obese patients undergoing bariatric surgery: findings of the prophylaxis against VTE outcomes in bariatric surgery patients receiving enoxaparin (PROBE) study. Obes Surg 2005;15:1368
–74. DOI
10.1381/096089205774859245
13. Borkgren-Okonek MJ, Hart RW, Pantano JE, et al. Enoxaparin thromboprophylaxis in gastric bypass patients: extended duration, dose stratification, and antifactor Xa activity. Surg Obes
Relat Dis 2008;4:625
–31. DOI 10.1016/j.soard.2007.11.010
14. Haas CE, Nelsen JL, Raghavendran K, et al. Pharmacokinetics and pharmacodynamics of enoxaparin in multiple trauma patients. J Trauma 2005;59:1336- 43; discussion 1343- 4. DOI
10.1097/01.ta.0000197354.69796.bd
15. Rutherford EJ, Schooler WG, Sredzienski E, Abrams JE, Skeete DA. Optimal dose of enoxaparin in critically ill trauma and surgical patients. J Trauma 2005;58:1167
–70. DOI
10.1097/01.ta.0000172292.68687.44
16. Duplaga BA, Rivers CW, Nutescu E. Dosing and monitoring of lowmolecular- weight heparins in special populations. Pharmacotherapy 2001;21:218
–34. DOI 10.1592/phco.21.2.218.34112
17. Nutescu EA, Spinler SA, Wittkowsky A, Dager WE. Low-molecularweight heparins in renal impairment and obesity: available evidence and clinical practice recommendations across medical and surgical settings. Ann Pharmacother 2009;43:1064
–83. DOI 10.1345/aph/1L194
18. Frezza EE, Chiriva-Internati M. Venous thromboembolism in morbid obesity and trauma. A review of literature. Minerva Chir 2005;60:391
–9.
19. Rowan BO, Kuhl DA, Lee MD, Tichansky DS, Madan AK. Anti-Xa levels in bariatric surgery patients receiving prophylactic enoxaparin. Obes Surg 2008;18:162 –6. DOI 10.1007/s11695–
007
–9381–4
20. Hirsh J, Bauer KA, Donati MB, Gould M, Samama MM, Weitz JI. Parenteral anticoagulants:
American College of Chest Physicians evidencebased clinical practice guidelines (8th edition).
Chest 2008;133:141S-59S. DOI 10.1378/chest.08
–0689
21. Simone EP, Madan AK, Tichansky DS, Kuhl DA, Lee MD. Comparison of two low-molecularweight heparin dosing regimens for patients undergoing laparoscopic bariatric surgery. Surg
Endosc 2008;22:2392
–5. DOI 10.1007/s00464–008–9997–6
22. Rondina MT, Wheeler M, Rodgers GM, Draper L, Pendleton RC. Weight-based dosing of enoxaparin for VTE prophylaxis in morbidly obese, medically-ill patients. Thromb Res
2010;125:220
–3. DOI 10.1016/j.thromres.2009.02.003
23. Cheymol G. Effects of obesity on pharmacokinetics implications for drug therapy. Clin
Pharmacokinet 2000;39:215
–31. DOI 10.2165/00003088–200039030–00004
24. Lin H, Faraklas I, Cochran A, Saffle J. Enoxaparin and antifactor Xa levels in acute burn patients. J Burn Care Res 2011;32:1
–5.
Conflict of interest
Authors reported none We thank Cathyyen Dang PharmD BCPS and Nick Lonardo PharmD for identification and screening of potential protocol patients.
The Annals of Pharmacotherapy. 2011;45(11):1356-
1362. © 2011 Harvey Whitney Books Company