Final Review Med Surg
advertisement

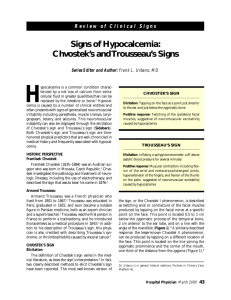
Med-Surg Final Review- Part 1 Increased Intracranial Pressure S/S: First sign- Decreasing LOC, headache, vomiting without nausea, papilledema, changes in VS, Cushing’s triad (late sign), Cheyne-Stokes respirations, posturing. Cushing’s Triad: hypertension, bradycardia, widening pulse pressure (systolic ↑, diastolic stays the same) Dx: Intracranial pressure monitoring device, skull radiography, CT, MRI, lumbar puncture, cerebral angiography. Tx: Goal is to maintain cerebral tissue perfusion and blood pressure. Keep oxygen saturation at 95%, HOB elevated 30 degrees, control temperature, administer anticonvulsants, Versed, antiemetics, etc to reduce the chances of anything happening that could increase ICP. IV: NS, LR, or 3% hypertonic saline. (Hypotonic or solutions with glucose can raise ICP.) Autonomic Dysreflexia Def: an exaggerated sympathetic nervous system response among those with a spinal cord injury above T6. S/S: Severe HTN decreased HR, pounding headache, nausea, blurred vision, sweating, and anxiety. Can lead to seizures, stroke, and death. Causes: Full bladder, abdominal distention, constipation, skin pressure, skin breakdown, exposure to hot or cold Prevent: administer antihypertensives, raise HOB, Foley catheter, and prevent triggers Immobilization of Spinal Injuries The head and back are immobilized mechanically with a cervical collar and back support. o Stabilizes the spinal column to help prevent movements which may lead to paralysis. After pt is stabilized, the injured portion of the spine is further immobilized using a cast, brace, or surgery. Traction is applied with weights and pulleys to decompress the spine. A turning frame is used to change the pt’s position without altering the alignment of the spine. Thyroid Gland- Hormones Thyroxine, T4; Triiodothyronine, aka T3 o Regulates (increases) body’s metabolic rate Calcitonin, aka thyrocalcitonin o Regulates serum calcium levels, o Secreted when serum calcium levels are high, inhibits shift of calcium from bones Tetany (see hypocalcemia also) The main symptom of sudden and acute hypoparathyroidism Develops when the parathyroid glands are accidentally removed during a thyroidectomy. S/S: twitches, tingling, dysrhythmias, seizures, spasms, laryngospasm. Signs: tap facial nerve mouth or jaw twitch or tighten = positive Chvostek’s sign Inflate BP cuff fingers spasm = positive Trousseau’s sign. Tx: Calcium salts IV or PO Antibiotic Therapy Take ALL antibiotics prescribed. Mastectomy Simple: removal of entire breast Radical: removal of all breast tissue, overlying skin, axillary lymph nodes, and underlying pectoral muscles Modified Radical: same as radical but with the muscles left intact. Post Op: Tamoxifen if ER+; elevate arm; no BPs, IV’s or sticks on affected side; no deodorant or shaving of affected side; progressively exercise affected side. Reconstruction: can be done immediately, or up to 1 year later. Diabetes Insipidus Pathology: Deficient or ineffective ADH S/S: massive diuresis—up to 30L/day, dehydration, polyuria, polydipsia, polyphagia Nsg: risk for fluid volume deficit--- strict I&O, daily weight Tx: IV fluids, vasopressin, Lypressin nasal spray, DDAVP Laryngeal Nerve Damage Severe, persistent hoarseness or inability to speak. May be due to trauma during thyroidectomy. Renal Scan Intravenous Pyelogram Radiographic dye is injected IV to see how the dye is concentrated by the kidneys and then excreted. Pictures are taken at 5-15 minute intervals Observe for stones and abnormalities. Prep: enemas, laxatives, fluids only or NPO for 8-10 hours before surgery, check for allergy to iodine or shellfish, tell pt they will experience a warm, flush, feeling. Teach: encourage fluids to flush out the dye, recognize s/s of allergic response. Hypocalcemia S/S: Tingling in the extremities and the area around the mouth (circumoral paresthesia), muscle and abdominal cramps, carpopedal spasms referred to as Trousseau's sign, mental changes, positive Chvostek's sign (spasms of the facial muscles when the facial nerve is tapped, laryngeal spasms with airway obstruction, tetany (muscle twitching), seizures, bleeding, and cardiac dysrhythmias. The client has hypocalcemia if the total serum calcium level is below 8.8 mg/dL (normal range, 9 to 11 mg/dL) or the ionized calcium level is below 4.4 mg/dL (normal range, 4.4 to 5.4 mg/dL). Keep emergency tracheostomy tray, mechanical ventilation equipment, artificial airway, and endotracheal intubation equipment at the client’s bedside if hypocalcemia is severe. IV line for the emergency administration of calcium. The nurse observes frequently for respiratory distress and notifies the physician immediately if this problem occurs. Until hypocalcemia is corrected, the nurse must assist the client with activities of daily living (ADLs). Movement, noise, and other environmental disturbances can trigger muscle contractions or convulsions. Thus, minimizing all forms of stress is essential until serum calcium levels approach normal and symptoms are relieved. Dietitian consult Cushing’s Syndrome Def: Hypersecretion of the adrenal cortex resulting in excess cortisol and other adrenal cortex hormones. Causes: Endogenous: Pituitary tumor, adrenal gland neoplasm, carcinoma of lung or other tissue. Exogenous: Prolonged high doses of corticosteroids. S/S: muscle weakness, truncal obesity, hirsutism, deep voice, irregular periods, HTN, hypokalemia, hyperglycemia, hypernatremia, increased cortisol levels. Tx: Depends on cause; slow tapering off of steroids, radiation, surgery (partial removal of pituitary gland to decrease ACTH secretion Meds: Aldactone for bilateral benign adrenal tumor. Chemo or other drugs that interfere with ACTH. Nsg: high risk of infection Subtotal Thyroidectomy (see Thyroidectomy for more info) Pt. will only need thyroid replacement meds for a few months. Exfoliative Dermatitis HIV Transmitted by: blood, semen, vaginal secretions, and breast milk Risk Factors: unprotected sex, contact with infectious fluids, sharing needles, receiving multiple blood transfusions, use of non-sterile tattooing equipment, AIDS: HIV converts to AIDS when the T4 cell count level goes from the normal 800 to 1200 Burn Injury Rule of Nines: Head and neck = 9% Right arm = 9% Left arm = 9% Posterior trunk = 18% Anterior trunk = 18% Right leg = 18% Left leg = 18% Perineum = 1% Superficial burn: pink to red and painful, sunburn, 1st degree Superficial Partial thickness burn: painful, blistered, weepy, 2nd degree Deep Partial thickness burn: painful, thick blisters or weepy edema, sensitive to cold, 3 rd degree. Full thickness burn: affects skin, fat, muscle, and bone. May be red, white, or black (eschar), often painless. 4th degree Fluid Resuscitation: Baxter Formula (3-4cc) x (kg of wt) x (% of body burned)= total CCs to be given in 24 hours ½ to be given in the first 8 hours ¼ to be given in the 2nd 8 hours ¼ to be given in the 3rd 8 hours Nsg interventions: reverse isolation, foley catheter, I&O is measured hourly, medicate with Morphine 30 minutes before dressing change, monitor for infection, high protein/high calorie diet. Diabetes Mellitus Type 1: no insulin production; requires injections for life Type 2: insulin resistance and or inadequate secretion S/S: polyphagia, polydipsia, polyuria, elevated BSL Dx: FSBS > 200 Fasting serum glucose > 110 (must fast for 8 hours) Urine sugar and acetone Glucose Tolerance Test Hgb A1C > 7% shows that the pt is not controlling hyperglycemia 7%=avg. BSL of 150 Emergency Complications: Acute Hypoglycemia (BSL < 70) s/s: diaphoresis, nervousness, shakiness Check blood sugar immediately Diabetic Ketoacidosis (DKA) s/s: Kussmaul’s respirations, fruity breath, 3 p’s, BSL > 300 Primarily a problem with type 1 Hyperglycemic hyperosmolar nonketonic syndrome (HHNKS) s/s: BSL > 600, but not ketone formation, comatose Pt is still producing some insulin: Type 2 Ketones: products of fatty acid metabolism Indicates breakdown of fats for energy, a sign that diabetes is out of control. Can lead to DKA. Instruct pt to test again in a few hours DO NOT exercise; call MD if moderate or large amounts found in urine. External Bleeding Arterial lacerations are evident when the blood is squirting with a lot of force in a rhythmic fashion. 3 treatments: 1. Direct pressure 2. Elevation 3. Pressure points (pulse site between the heart and laceration) Carotid, axillary, brachial, radial, femoral, popliteal, pedal Tourniquet is used as a last resort because it can cause tissue death and can lead to amputation. Uncontrolled bleeding can lead to shock. Blood Transfusion Saline is the only fluid that can be given with blood. Transfusion Reactions Complication Signs and Symptoms Cause(s) Action Incompatibility reaction Hypotension, rapid pulse rate, difficulty breathing, back pain, flushing Mismatch between donor and recipient blood groups Stop the infusion of blood. Infuse the saline at a rapid rate. Call for assistance. Administer oxygen. Raise the feet higher than the head. Be prepared to administer emergency drugs. Send first urine specimen to laboratory. Save the blood and tubing. Febrile reaction Fever, shaking chills, headache, rapid pulse, muscle aches Allergy to foreign proteins in the donated blood Stop the blood infusion. Start the saline. Check vital signs. Report findings. Septic reaction Fever, chills, hypotension Infusion of blood that contains microorganisms Stop the infusion of blood. Start the saline. Report findings. Save the blood and tubing. Allergic reaction Rash, itching, flushing, stable vital signs Minor sensitivity to substances in the donor blood Slow the rate of infusion. Assess the client. Report findings. Be prepared to give an antihistamine. Circulatory overload Hypertension, difficulty breathing, moist breath sounds, bounding pulse Large volume or rapid rate of infusion; inadequate cardiac or kidney function Reduce the rate of infusion. Elevate the head. Give oxygen. Report findings. Be prepared to give a diuretic. Hypocalcemia Tingling of fingers, hypotension, muscle cramps, convulsions Multiple blood transfusions containing anticalcium agents Stop the blood infusion. Start saline. Report findings. Be prepared to give CaCl DIC- disseminated intravascular coagulation Can happen as a complication of shock. Normally, when you are injured, certain proteins in the blood become activated and travel to the injury site to help stop bleeding. However, in persons with DIC, these proteins become abnormally active. Small blood clots form within the blood vessels. Some of these clots can clog up the vessels and cut off blood supply to various organs such as the liver or kidney. These organs will then stop functioning. Over time, the clotting proteins become “used up.” When this happens, the person is then at risk for serious bleeding from even a minor injury. This disorder can result in clots or, more often, in bleeding. The bleeding can be severe. Risk factors for DIC include: Blood transfusion reaction Cancer, including leukemia Infection in the blood by bacteria or fungus Pregnancy complications (such as retained placenta after delivery) Recent surgery or anesthesia Sepsis (an overwhelming infection) Severe liver disease Severe tissue injury (as in burns and head injury) Dx: PTT – high Platelets – low PT – high Tx: The goal is to determine and treat the underlying cause of DIC. Blood clotting factors will be replaced with plasma transfusions. Heparin is sometimes used. Thyroidectomy Pre-op: admin antithyroid meds for several weeks, teach to avoid neck strain, Post-op: HOB elevated 30° or more, ice bag to neck, trach set at bedside, suction equipment, VS q1-4 hrs, check dressing and back of neck for bleeding, Monitor for: Airway obstruction (restlessness, tachycardia, dyspnea), laryngeal nerve damage (severe hoarsness or inability to speak), hemorrhage (check dressing and back of neck), tetany, thyroid crisis Total thyroidectomy will require lifelong replacement of thyroid hormones; Take meds exactly as prescribed Components of Immune System ABG’s Normal: 80-100 mmHg Shock: below 60 mmHg If SpO2 (oxygen saturation) is above 90%, the PaO2 is most likely 60 mmHg or above. Gastric Surgery Post-Op: No ASA or NSAIDS, will need lifetime injections of B12 Side effect can be dumping syndrome o Occurs due to decreased size of stomach or loss of vagus nerve prevents normal pacing of chyme movement o Fluid is drawn out of the blood within 15-30 min of eating to moisten food o S/S: BP falls, becomes dizzy, diaphoretic and weak, cramps, hyperactive bowel sounds, urge to defecate o Teach: Usually resolves within a few months; lay down after meals until dumping syndrome resolved; 6 meals/day: low carb, mod. fat, high protein; drink fluids between meals, not with them; may have chronic diarrhea-do good skin care Hemoglobin and Nutrition Foods rich in iron enhance hemoglobin production. Fractures Immobilize joints on both sides of possible fracture. Splint in the position found 4 interventions: check pulses immobilize ice elevate 5 P’s when assessing and charting a fracture: Pain Pallor Pulses Paresthesia- nerve damage, numbness, tingling Paralysis Wound Healing Primary intention: wound layers are sutured together and well approximated. Heals relatively fast with minimal scarring Secondary intention: granulating tissue fills the wound. Edges are not approximated. Healing is slow, and happens from the bottom up. Needs moisture. Complication of wet dressing left on too long: maceration If dressing is stuck: moisten with sterile saline and pull gently. Cold Injury IV access can be difficult to obtain because the cold causes vasoconstriction. Places other than arms, hands, and legs for IV access: subclavian, jugular, and femoral Areas most affected by cold injury: hands, feet, nose, cheeks S/S: 1. Pain, 2. Tingling, 3. Numbness How to re-warm: warm blankets, warm oral fluids, and warm IV fluids Highest risk: elderly- more susceptible because of loss of sub-q fat, diminished circulation, and reduced neural control of circulation Treatment goal: Temp > 95°, good circulation and warmth to tissues without tissue cellular damage Chemotherapeutic Agents Tissue Plasminogen Activator (t-PA) Used for treatment of ischemic stroke. “Clot buster”- will dissolve the clot in the brain Must start within 3 hours of the onset of symptoms. Will dissolve all clots… so make sure there are no wounds. Erythropoietin Secreted by the kidneys to stimulate RBC production Decreased O2 in blood triggers this response Pts with renal failure are deficient in erythropoietin Morphine Up to 50mg/hr PCA for burn pts. Tattoos Pigments are not FDA approved Interfere with MRI- poor picture quality Infection: Hep. B, C, HIV, tinea corporis (tx with antifungals), Staph (tx with topical ATB x10 days) Skin Care: avoid soaking, do not touch area, cover with ATB cream, good hand hygiene, wash area TID with antibacterial soap and pat dry, apply lotion x2 weeks, avoid direct sunlight to area x4 weeks. Removal: painful, never looks like it did pre-tattoo. Piercings Healing Time: Ear lobe: 6-8 wks Ear cartilage: 4mo-1yr Eyebrow: 6-8 wks Nostril: 2-4 mo Tongue: 4 wks Lip: 2-3 mo Navel: 4mo-1yr