I-site - case report
advertisement
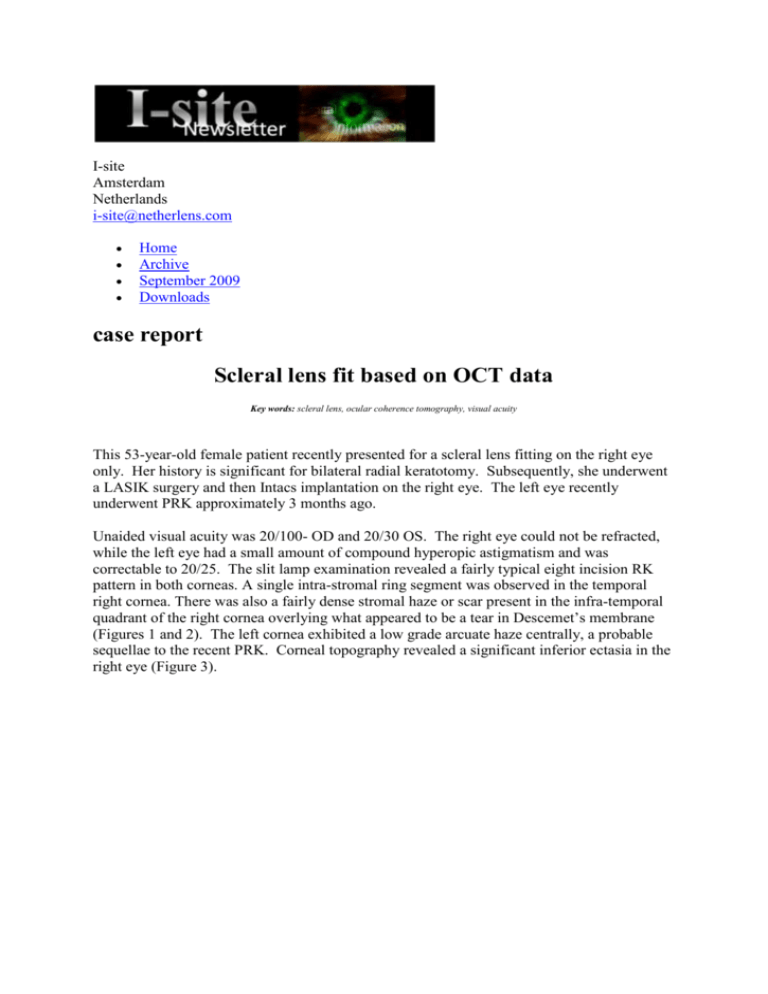
I-site Amsterdam Netherlands i-site@netherlens.com Home Archive September 2009 Downloads case report Scleral lens fit based on OCT data Key words: scleral lens, ocular coherence tomography, visual acuity This 53-year-old female patient recently presented for a scleral lens fitting on the right eye only. Her history is significant for bilateral radial keratotomy. Subsequently, she underwent a LASIK surgery and then Intacs implantation on the right eye. The left eye recently underwent PRK approximately 3 months ago. Unaided visual acuity was 20/100- OD and 20/30 OS. The right eye could not be refracted, while the left eye had a small amount of compound hyperopic astigmatism and was correctable to 20/25. The slit lamp examination revealed a fairly typical eight incision RK pattern in both corneas. A single intra-stromal ring segment was observed in the temporal right cornea. There was also a fairly dense stromal haze or scar present in the infra-temporal quadrant of the right cornea overlying what appeared to be a tear in Descemet’s membrane (Figures 1 and 2). The left cornea exhibited a low grade arcuate haze centrally, a probable sequellae to the recent PRK. Corneal topography revealed a significant inferior ectasia in the right eye (Figure 3). Figure 1: OD at 90 degree Figure2: OD at 180 degree The plan was to fit the right eye with an 18mm diameter scleral lens to improve the visual acuity as well as reduce the symptoms of dryness. To that end, several anterior segment scans were taken of the right eye using the Visante Optical Coherence Tomographer, or OCT, (Carl Zeiss) to better fit the scleral lens, as described in a recent article on the novel technique of fitting scleral lenses using OCT images in the March 2008 issue of Eye & Contact Lens: Science and Clinical Practice by this author. Figure 3: Corneal Topography summary map Because the maximum width of the Visante OCT scan is 16mm, several images were taken and assembled into a composite using Adobe Photoshop CS-3 software. Image analysis tools were then used to construct the proposed design over the composite image. Figure 4 shows the outline of the proposed design (red line). Instead of using simulated “K” readings, the power was calculated by performing a refraction over a corneal-scleral lens from a trial set. Figuur 4: OD composite design The lens specifications were then sent to Truform Optics (Euless, Texas) where the lens was manufactured in Boston XO material and plasma treated. The very next day the scleral lens was dispensed, resulting in visual acuity of 20/25, the same as the left eye. No modifications were necessary, as the lens demonstrated good centration, clearance, and no scleral compression. In view of the compromised endothelium, the patient was instructed to go slow in increasing the wearing time. After one week, the patient had built up to eight hours of continuous wear without symptoms. The lens was removed only to satisfy the wearing schedule. She stated that the comfort was excellent, with minimal or no awareness. Visual acuity was still 20/25, and the eye looked exactly as it did on the day the lens was dispensed. An OCT scan was taken with the lens in place (Figure 5). The inside surface of the lens is outlined in yellow, and is as predicted from the original design in Figure 4. Figure 5: OD composite actual This case study reflects the efficacy of fitting scleral lenses using OCT or other digital images of the anterior eye. The author has been using this technique for more than 18 months with great success. With few exceptions, the author no longer uses trial lenses for GP lens design. The author has also designed corneal lenses using this technique with equally efficacious results. While the technique is very flexible and open with respect to design variables, one still has to work within the limitations of the manufacturing equipment and to design within those constraints. Greg Gemoules ODDallas TX USA Greg Gemoules is a 1983 graduate of the Illinois College of Optometry and holds a B.A. degree in Chemistry from Millikin University, both in the USA. He has been in private practice in the Dallas area (Texas, USA) area since 1984. He specializes in the custom design and fitting of specialty contact lenses for complex corneas, including dry eye, keratoconus, and post-refractive surgery. Greg has authored several research papers on contact lenses in the peer reviewed literature. He has been an invited speaker at the Contact Lens and Eyecare Symposium, the Contact Lens Association of Ophthalmologists annual meeting, the CLAO Education and Research Symposium, the Global Specialty Lens Symposium, and the Sjogren’s Syndrome Foundation Dry Eye Conference. I-site Amsterdam Netherlands i-site@netherlens.com