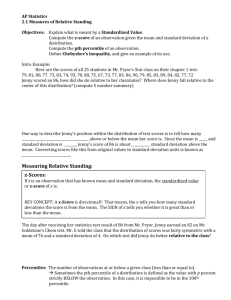
PATIENT CHART Chart for Jenny Brown Simulation #1 STUDENT
advertisement

PATIENT CHART Chart for Jenny Brown Simulation #1 STUDENT NAME:_______________________________ PATIENT INITALS: ___J.B._______________________ CLINICAL DATE(S): _____________________________ INSTRUCTOR: _______________ Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 1 Patient Name: Jenny Brown Room: DOB: Age: 23 MRN: 234-56-7891 Doctor Name: Dr. Marianne Hough Date Admitted: Diagnosis: Generalized anxiety disorder with panic attack, possible PTSD Patient Report (Report from nurse ending shift) Current time: 0700, 2 days after admission to short stay acute psychiatric unit Situation: Jenny Brown is 23 years old, admitted two days ago for acute agitation and anxiety. She is 18 weeks pregnant with her first baby. She was voluntarily admitted from the Emergency Department where she was taken following an episode of acute agitation after ultrasound in the hospital’s Imaging Services Department. She received several doses of IV haloperidol in the ED before being transferred to our unit. Background: While she was in Imaging for a routine ultrasound, Jenny had to be restrained. Apparently she became extremely agitated when the perinatologist told her that the fetus, a girl, has a cleft lip and palate. She was transferred to the Emergency Department and given three 2 mg doses of IV haloperidol over approximately 4 hours. Her suicide assessment was negative but she doubted her ability to safely care for herself at home and she agreed to admission for evaluation. On the first day of admission, she received 2 mg. oral haloperidol regularly, every 4 hours. Yesterday she only had two doses and seemed much more stable. She still had difficulty sleeping and woke screaming from nightmares the first night. Last night she refused the haloperidol and slept on and off but there were no nightmares. Assessment: Vital signs: T: 98.6, Pulse: 76, regular; Respirations: 16, BP: 112/74. Admitting diagnosis was panic attack with underlying generalized anxiety disorder and possible PTSD. She has no psychotic behaviors and is well oriented X3. Her prenatal admission assessment was done per protocol and everything looks good. Fetal heart rate is in the 130s. She’s also had the full psychiatric intake exam. Last night she slept poorly. She cries from time to time and is worried about her baby. Her vital signs have been stable. She has suicide checks ordered every 12 hours but so far those are all negative. She says she won’t harm herself because of the baby. She has showered and is well groomed with a normal train of thought and full vocabulary. She maintains eye contact when speaking. She has rapid, pressured speech at times. She is sometimes fidgety when seated and paces to calm herself. She’s been talking on the phone with her boyfriend from time to time all night – this seems to help calm her. Recommendation: She is due for a mental status check with depression, suicide, and PTSD evaluations – the forms are on the chart. There will be a care conference later today to plan for discharge and follow-up, so the team will need the results of your assessment. Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 2 Provider’s Orders Allergies: NKA Date/Time: Acute Mental Status Change Admission Orders Tuesday Admit to Acute Short Stay Psychiatric Unit 2000 Service: Psychiatry Condition of patient: Good 1. DIET: Regular diet as tolerated 2. VITAL SIGNS: q4h with fetal heart rate check; notify MD for Temp above 101.5, HR>120, decline in neuro status, absence of FHT 3. ACTIVITY: as tolerated 4. SAFETY CHECKS: Q2h for first 24 hours, then q4h 5. LABS: H&H 6. MEDICATIONS: a. Haloperidol 2 mg PO q4h prn agitation, anxiety; may repeat in 2 hrs prn severe anxiety- notify physician b. Haloperidol 5 mg IV for severe agitation – notify physician c. Prenatal vitamin X 1 po daily in am d. Acetaminophen (Tylenol) 650 mg q6h prn headache 7. IV ORDER: If need to start IV to administer medication, leave saline lock in place 8. MISCELLANEOUS: When patient is stable, complete assessment forms for anxiety and depression, PTSD, TBI, military sexual trauma, and suicide in preparation for team conference Thursday afternoon. Marianne Hough, MD Stat Order Form Date/Time: STAT PHYSICIAN ORDER Tuesday Haloperidol 2 mg IV stat. Repeat every 2-4 hours prn for up to 4 doses. 1500 Katherine Shannon, MD Lab Data Date/Time: Sunday 1600 Chemistries Test: Sodium Result: 137 mEq/L Reference range: 135-145 mEq/L Potassium 4.0 mEq/L 3.5-5.2 mEq/L Calcium 8.5 mg/dl 8.5 – 10.2 mg/dl Carbon dioxide 26 mEq/L 20-29 mEq/L Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 3 Hematology Urinalysis Chloride 103 mEq/L 96-106 mEq/L Glucose 99 mg/dl 74 -106 mg/dl Bun Creatinine 15 mg/dl 1.0 mg/dl 7-20 mg/dl 0.8 – 1.4 mg/dl Hematocrit 42% 38 – 43% Hemoglobin 14 g/dl 12 – 16 mg/dl Specific gravity 1.005 1.002 – 1.030 pH 5 5–7 Leukocytes Neg Neg Nitrite Neg Neg Protein (mg/dL) Neg Neg - Trace Glucose (mg/dL) Neg Neg Ketones Neg Neg Urobilinogen (mg/dL) Neg Neg Bilirubin Neg 0.2 – 1.0 Ehr U/dl Micro Neg RBCs: 0-2/HPF WBC: 0-2/HPF RBC Casts: 0/HPF Medication Administration Record Allergies: NKA Scheduled & Routine Drugs Date of Order: Medication: Dosage: Route: Frequency: Prenatal vitamin Hours to be Given: 0900 Dates/Times Given/Initials: - Wednesday/ 0900 AC Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 4 STAT Medications Date of Order: Medication: Dosage: Route: Frequency: Haloperidol 2 mg IV stat Repeat every 2-4 hours prn for up to 4 doses Hours to be Given: Dates/Times Given/Initials: - Tuesday/ 1600 RR - Tuesday/ 1800 RR - Tuesday/ 2000 RR PRN Medications Date of Order: Medication: Dosage: Route: Frequency: Hours to be Given: Dates/Times Given/Initials: Haloperidol 2 mg po q4 hrs prn agitation, anxiety - Tuesday/ 2200 TJF - Wednesday/ 0200 TJF - Wednesday/ 0600 TJF Haloperidol 5 mg IV for severe agitation. Notify provider - Tylenol (acetaminophen) 650 mg q6h prn headache - Nurse Signatures Date/Time Initial TJF RR AC Nurse Signature Teresa Franklin, RN Richard Reid, RN Angela Corbo, RN Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 5 Medical Reconciliation Form Source of medication list (check all that apply) patient medication list, patient/family recall, pharmacy, PCP list, previous discharge paperwork, MAR for facility Allergies: NKA Medication Name Dose Route Frequency Last Dose Continue/DC Prenatal vitamins 1 tab PO Daily Tuesday AM C DC Tylenol 650 mg PO PRN Headache N/A C DC Provider Signatures Date/Time Tuesday 1700 Initial MH Provider Signature Marianne Hough, MD Initial RR Nurse Signature Richard Reid, RN Nurse Signatures Date/Time Tuesday 1700 Reviewed on Transfer by: Teresa Franklin, RN Reviewed on Discharge by: Scan to Pharmacy Time: Date: Tuesday 2100 Date: Date: Patient Name: Jenny Brown Physician: Marianne Hough, MD Diagnosis: Generalized anxiety disorder with panic attack, possible PTSD Age: 23 Gender: Female Height: 5’6” Weight: 130 lbs Major Support: Boyfriend/partner Eric Phone: 555-555-5555 Eric (boyfriend) 555-555-5566 Type of Operation: None History: IUP – 18 weeks, fetus with known cleft lip & palate Advanced Directives: No Allergies: None known Fall Precautions: High Isolation Precautions: Standard Restraints: No Diet: Regular Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 6 Monitoring Vital signs – Q4h FHR checks – Q4h Mental status checks – Q4h Medication Oral medications IV medication Respiratory Social History - Lives in own home with boyfriend, Eric - College student - Parents live in another state Consults - Comprehensive care team: Alicia Green, RN-C; Patricia Gooding, LCSW; Diane Moos, MD/R-1; Todd Grainger, MD/R-3 Treatments Activities of Daily Living As tolerated, self-directed Discharge Planning - Consult neonatology, pediatric surgeon to visit patient before discharge - Home care follow-up Race/religion: Christian Medication brought from home: None Diagnostic Studies Lab – H&H on admission Anxiety and Depression Scale and Scoring (Adapted for Interview) Possible nursing prompts: “When you answer, please use the terms: ‘definitely,’ ‘sometimes,’ ‘not much,’ or ‘not at all.’ If you forget to use one of those words, I will remind you.” “Would you say, ‘definitely,’ ‘sometimes,’ ‘not much,’ or ‘not at all’?” Jenny’s Responses for Scenario: Question: 1. Do you have trouble sleeping at night? 2. Do you feel anxious or stressed for apparently no reason at all? 3. Do you feel miserable or sad? 4. Does leaving your house make you feel anxious? Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 7 5. Have you lost interest in things that you used to enjoy? 6. Do you feel like your heart is racing? 7. Do you have a good appetite? 8. Do you sometimes feel scared or frightened when there is no reason to do so? 9. Do you ever feel like the world would be better without you in it? 10. Do you feel restless or fidgety? 11. Are you more irritable than usual? 12. Do you feel as if it’s hard to get things done? 13. Do you seem to worry all the time? Score: Scoring: Questions 1-6, 8-13 Question 7 Scoring Interpretation: Definitely 3 0 0-7 Minimal concern Sometimes 2 1 8-10 Borderline concern Not often 1 2 11+ Concerning – may need further intervention Not at all 0 3 Anxiety Questions: # 2, 4, 6, 8, 10, 11, 13 Depression Questions: # 1, 3, 5, 7, 9, 12 Source: Snaith R.P. The Hospital Anxiety and Depression Scale. Health and Quality of Life Outcomes 2003;1:29 http://www.hqlo.com/content/1/1/29; http://www.abiebr.com/node/410 Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 8 Suicide Risk Assessment Screening Questions Question: Possible Nursing Prompts: Jenny’s Responses for Scenario: 1. Are you feeling hopeless about the present/future? 2. Have you had thoughts of taking your life? 3. When did you have these thoughts? 4. Do you have a plan to take your life? 5. Have you ever had a suicide If yes, tell me what you’ve been thinking (or about your plan). If yes, can you tell me about that time? attempt? Although the nursing role does not involve establishing a diagnosis of suicide risk, the nurse should notify a licensed independent provider of the findings of any positive screen and take precautions to protect the safety of the patient. Source: VA Suicide Risk Assessment Guide available at: http://www.mentalhealth.va.gov/docs/VA029AssessmentGuide.pdf Primary Care Post Traumatic Stress Disorder Screen (PC-PTSD) Possible nursing prompt: “Would you say ‘yes’ or ‘no’?” Base Question: In your life, have you ever had any experience that was so frightening, horrible, or upsetting that, in the past month, you: Jenny’s Responses for Scenario: 1. have had nightmares about it or thought about it when you did not want to? 2. tried hard not to think about it or went out of your way to avoid situations that reminded you of it? 3. were constantly on guard, watchful, or easily startled? Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 9 4. felt numb or detached from others, activities, or your surroundings? Although the nursing role does not involve establishing a diagnosis of PTSD, current research suggests that the results of the PC-PTSD should be considered "positive" if a patient answers "yes" to any three items. The nurse should notify a licensed independent provider of the findings of any positive screen. Sources: United States Department of Veterans Affairs National Center for PTSD; Professional Section http://www.ptsd.va.gov/professional/provider-type/doctors/screening-and-referral.asp http://www.ptsd.va.gov/PTSD/professional/pages/assessments/assessment-pdf/pc-ptsd-screen.pdf 3-Question TBI Screening Tool Question: Possible Nursing Prompts: 1. Did you have any injury or injuries during your deployment from any of the following: bomb fragment? bullet? any type of vehicle including airplanes? fall/injury? blast (improvised explosive device, RPG, land mine, grenade, etc.? something else? If yes, ask about the type of injury. 2. Did any injury received while you were deployed result in your: being dazed, confused, or “seeing stars”? not remembering the injury? losing consciousness (being “knocked out”) for any length of time? having symptoms afterward like headache, dizziness, irritability, etc.? head injury (closed or open) that required medical treatment? [No verbal response necessary; make note of each positive answer.] Jenny’s Responses for Scenario: Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 10 3. Are you currently experiencing any of the following problems that you think might be related to a possible head injury or concussion: headaches? dizziness? memory problems? balance problems? ringing in the ears? irritability? sleep problems? other? (please be specific): [No verbal response necessary; make note of each positive answer.] Although the nursing role does not involve establishing a diagnosis of PTSD, current research suggests that the results of the PC-PTSD should be considered "positive" if a patient answers "yes" to any three items. The nurse should notify an appropriate licensed provider of the findings of any positive screen. Patient endorsement of items in #2 meets criteria for positive TBI screen. Confirm symptoms of concussive symptoms or head injury through clinical interview. Source: Schwab, K. A., Baker, G., Ivins, B., Sluss-Tiller, M., Lux, W., & Warden, D. (2006). The Brief Traumatic Brain Injury Screen (BTBIS): Investigating the validity of a self-report instrument for detecting traumatic brain injury (TBI) in troops returning from deployment in Afghanistan and Iraq. Neurology, 66(5)(Supp. 2), A235. This is a work of the U.S. government and is not subject to copyright protection in the United States. It may be reproduced and distributed in its entirety without further permission from GAO (http://www.gao.gov/assets/280/271994.html). Chart Materials Jenny Brown – Simulation #1 © National League for Nursing, 2015 11