Sl No. Description of Field Details 1 Names of Author/ Authors ( as
advertisement

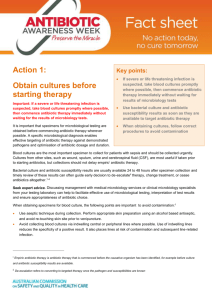
Sl No. 1 Description of Field Details Names of Author/ Authors ( as you want them to appear in the journal) in the same order as in copyright form 1.Dr. Rajlaxmi Upadhyay 2.Dr. Manas Ranjan Upadhyay 3. 4. 5. 6. 7. 8. 2 Designation and affiliation of each of the authors 1.MBBS, M.D. (Pharmacology) 2.MBBS, M.D.(Pediatrics),DM. (Neonatology) 3. 4. 5. 6. 7. 8. 3 Institution to which the research is associated with 4 Corresponding author’s name and address 5 Corresponding author’s email id 6 7 Contact number ( preferably mobile number) of the corresponding author Running title of the article 8 Keywords 9 MeSH terms ( optional but highly recommended)to obtain MeSH terms go to the following URL http://www.nlm.nih.gov/mesh/MBrowser.html Total number of Tables and Figures 10 Newborn and Pediatric Health Centre, Cuttack, Odisha Dr. Rajlaxmi Upadhyay,c/o Dr. Manas Ranjan Upadhyay, newborn and pediatric health centre, plot No D/54, sector 7, CDA, Cuttack, Odisha. 753014 drrajlaxmi@yahoo.co.in 09437017044 Prevalence of Recent Microbial Isolates and Current Trends in Antimicrobial Resistance in a Referral Paediatric Hospital (Cuttack) Antimicrobial Resistance, Recent microbial isolates 11 12 Type of articleE.g.- original article/case report/review article/letter to the editor etc Original article Department Pharmacology Abstract Prevalence of recent microbial isolates and current trends in Antimicrobial resistance in tertiary care hospital and referral Neonatal unit of Cuttack in state of Odisha 5. Introduction: Odisha has a very (IMR) of 71per 1000 live births as compared to the national figure of 55. Sepsis is the commonest cause.Importance of the study is to emphasize the need of rationalizing antibiotic therapy, formulate appropriate empirical antibiotic therapy, unit specific and determined by the prevalent spectrum of etiological agents and their antibiotic sensitivity pattern and often guided by the source of infection, need of universal blood culture before antibiotic therapy- to help in modification of therapy according to the sensitivity reports. Methods: Study conducted at a level 3,eleven Bedded, tertiary care private NICU at Cuttack, Odisha. Clinically suspected cases of bacteremia were included in the study. After clearance of ethics committee, data wascollected in a predesigned proforma .Blood culture were collected under strict asepsis.The isolates, identified by BACTEC culture systems by a standard lab. All the data collected will be entered into data sheets and then electronically into spread sheets for analysis. Results Staphylococcus aureus was the most frequently isolated pathogen followed by Acenetobacter and enterococcus in equal percentages .15% of culture positives were late onset cases.100% of LOS had H/O previous hospital admission and antibiotic therapy. The organisms isolated in EOS - (Staphylococcus- 66%, Acenetobactor- 17%, Enterococcus 17%.). in LOS- Staphylococus (CONS) in all cases. Resistance pattern of Staph. Isolate : Vancomycin- moderately sensitive,partly sensitive, Teicoplanin- 50% resistance, Methicillin - 25% resistance, Cotrimoxazole, amoxyclav, cefopodoxime, Ciprofloxacin- all resistant, Linezolid and amikacin – 100% sensitivity seen. Resistance pattern of Acenetobacter. Isolate as noted in the study isCefipime , ceftriaxone, cefoperazone, aztreonam resistance- 100% resistant,Ciprofloxacin, imipenem, piperacillintazobactam, meropenem, Livofloxacin, netilmycin sensitivity- 100% Resistance pattern of Enterococcus. Isolate: No Significant resistance noted is Vancomycin, clindamycin, teicoplanin, linezolid, amikacin, ciprofloxacillin, cefoperazone Sensitivity- 100% Conclusion More such studies are essential in all set up to study the pattern of isolates, prevalence and resistance pattern to help choosing the correct antibiotic. Most important step to avoid growing antibiotic resistance is to avoid unnecessary antibiotic use( prophylactic),strong emphasis on asepsis, early breastfeeding , skincare, strong unit policy for antibiotic use. Prevalence of Recent Microbial Isolates and Current Trends in Antimicrobial Resistance in a Referral Paediatric Hospital at Cuttack, Odisha R. Upadhyay1, M.R.Upadhyay2 1. MO, Itamati PHC (N),Nayagarh,Odisha 2. Director Newborn and Pediatric Health centre Corresponding Author: drrajlaxmi@yahoo.co.in Introduction Sepsis is the commonest cause of neonatal mortality amounting to 30- 50% of total neonatal mortality rate in developing countries. 20% of all neonates develop sepsis and 1% die of sepsis related causes. Prematurity and low birth weight babies are at higher risk of sepsis and sepsis related death. Sepsis related deaths are largely preventable with strict aseptic practice, skin care, early initiation of breast milk, rational antimicrobial therapy and aggressive supportive care. Early Onset Sepsis (EOS) occurs within first 72 hours of life, may be symptomatic at birth with respiratory distress and pneumonia or asymptomatic, risk factors of EOS are low birth weight (<2500 grams) or prematurity, febrile illness in the mother with evidence of bacterial infection within 2 weeks prior to delivery, foul smelling and/or meconium stained liquor, Rupture of membranes >24 hours, single unclean or > 3 sterile vaginal examination(s) during labor, prolonged labor (sum of 1st and 2nd stage of labor > 24 hrs), perinatal asphyxia (Apgar score <4 at 1 minute),presence of foul smelling liquor or three of the above mentioned risk factors warrant initiation of antibiotic treatment. Infants with two risk factors should be investigated and then treated accordingly. Late onset sepsis (LOS) presents after 72 hours of age.where source of infection is Nosocomial or Community-acquired. Clinical presentation ranges from septicemia, pneumonia or meningitis. Risk Factors of LOS-low birth weight, prematurity, admission in intensive care unit, mechanical ventilation, invasive procedures, administration of parenteral fluids, and use of stock solutions. Risk Factors of Community-acquired LOS - poor hygiene, poor cord care, bottle-feeding, and prelacteal feeds. In contrast, breastfeeding helps in prevention of infections. Thus the study objective is to describe the pattern of bacterial isolates from the blood cultures in the NICU , find their current resistance pattern, help in deciding appropriate choice of antibiotics in empirical treatment .Importance of the study lies in the fact to emphasize the need of Rationalize antibiotic therapy. When the baby is asymptomatic and without any risk factor- avoid antibiotics, when there is two or less risk factor – do septic screen and start antibiotics if the test is positive, emperic antibiotic therapy only when the baby is diagnosed clinical sepsis or there is foul smelling liquor, formulate appropriate empirical antibiotic therapy, Unit-specific and determined by the prevalent spectrum of etiological agents and their antibiotic sensitivity pattern and often guided by the source of infection, need of universal blood culture before antibiotic therapy- to help in modification of therapy according to the sensitivity reports. Methods This is a prospective observational study over a period of 4 months (June to sept.2011) in a Level 3,eleven beded, tertiary care private Neonatal ICU of Newborn and Pediatric Health Centre , Cuttack. Clinically suspected cases of bacteremia were included in the study ( all clinical sepsis or asymptomatic with risk factors following positive sepsis screen ).Data was collected in a predesigned proforma that included-Standard demographic information, weight, gestation, clinical presentation,the risk factors of sepsis, H/O previous hospital admission, H/O of previous antibiotic administration, organism isolated, antibiotic sensitivity pattern. Blood cultures were collected under strict aseptic precaution - proper hand washing, use of sterile gloves, skin sterilization with spirit- Betadine( 1min)- Spirit, Fresh veinepuncture, 1-2ml blood collected from the hub and transferred to the culture bottle The isolates were identified by BACTEC culture systems by a standard lab.Bacterial growth detected within 12 to 24 hrs and sensitivity reported within 3-4 days. Antibiotic Policy of the ICU noted as Emperic antibiotic therapy started when symptomatic baby with strong clinical possibility of infection, cases where sepsis screen is positive, case where there is high risk of neonatal sepsis ( FSL or 3 or more risk factor) and antibiotic therapy is modified after getting sensitivity reports in culture positive cases, also early stoppage of antibiotics when the culture is negative and clinical course is not like sepsis. The antibiotics choice practised in the ICU in case of EOS is Cefotaxime/cefepime with amikacin, Vancomycin with amikacin when the baby is term and presented with pneumonia. In LOS is Cefotaxime/ cefepime with amikacin in community aquired sepsis, piperacillin + tazobactam/ Meropenem with amikacin- hospital acquired and Vancomycin with amikacin- when there is pneumonia Results Out of 100 blood samples positive cultures were obtained in 14% cases. Staphylococcus aureus was the most frequently isolated pathogen (57%), followed by Acenetobacter and enterococcus in equal percentages (21.4%).EOS –Suspected in 64 cases ,85% of culture positives were EOS, all cases of EOS were directly admitted to the hospital, LOS-Suspected were 36 cases, 15% of culture positives were late onset cases.100% of LOS had H/O previous hospital admission and antibiotic therapy. The organisms isolated were 64 cases of EOS of which- 19% were culture positive (Staphylococcus66%, Acenetobactor- 17%, Enterococcus -17%.) 36 numbers were LOS out of which 5.5% culture positive where the organism was Staphylococus (CONS) in all cases 100%. Resistance pattern of Staph. Isolate as found out from the study is : Vancomycin is75%(6 out of 8) moderately sensitive, 25% sensitive, Teicoplanin- 50% resistance, Methicillin - 25% resistance, Cotrimoxazole, amoxyclav, cefopodoxime, Ciprofloxacin- all resistant, Linezolid and amikacin – 100% sensitivity seen. Resistance pattern of Acenetobacter. Isolate as noted in the study-Cefipime , ceftriaxone, cefoperazone, aztreonam resistance- 100% resistant,Ciprofloxacin, imipenem, piperacillin- tazobactam, meropenem, Livofloxacin, netilmycin sensitivity- 100% Resistance pattern of Enterococcus. Isolate: No Significant resistance noted is Vancomycin, clindamycin, teicoplanin, linezolid, amikacin, ciprofloxacillin, cefoperazone Sensitivity- 100% Discussion Very low percentage of overall culture positivity rate as compared to the available NNPD data ( 14% vs 32%) .May be due to higher incidence of prehospital antibiotic use which is more apparent in case of late onset sepsis. In our case the most common isolate is gram positive coci (57%) where as in NNPD only 13.6% in EOS and 15% in LOS are gram positive cocci. In NNPD the most common isolate in both form of sepsis is klebsiella ( EOS- 32.5%, LOS- 27%). In case of staphylococus 25% isolate are only sensitive to vancomycin vs 73.5% in NNPD(2002-3) data which could indicate time trend of growing vancomycin resistance. Acenetobactor was the most common gram negative isolate where as klebsiella was most common in NNPD data, this was almost resistant to cephalosporin but showing good sensitivity to ciprofloxacin piperacillin tazobactam, imipenem, meropenem and netilmycin. In our observation by and large the eneterococus is sensitive to the common antibiotics.From the finding it was very obvious that resistance is a growing problem. In case of staph the vancomycin and teicoplanin resistance is a emmerging problem, however with still good sensitivity towards amikacin and linezolid the emperic gram positive therapy should gradually change to linezolid and amikacin.The gram negative isolate have developed good resistance to common third generation antibiotics.Sensitivity towards Piperacillin tazobactam, imipenem, meropenem, ciprofloxacin and netilmycin is well mentained. So gradually with emmerging resistance the third generation cephalosporin is becoming useless forcing the clinician to go more and more for reserve drugs as mentioned above Conclusion For the fierce antimicrobial resistance the cry of the hour is no action today, no cure tomorrow. Many more such studies are essential in all set up to study the pattern of isolates, prevalence and resistance pattern to help choosing the correct antibiotic. Most important step to avoid growing antibiotic resistance is to avoid unnecessary antibiotic use( prophylactic),strong emphasis on asepsis, early breastfeeding , skincare,strong unit policy for antibiotic use. It is very essential to rule out sepsis by tests so as to avoid unnecessary use of antibiotics,universal blood culture before antibiotics - help pin point the antibiotic therapy, ? Early stoppage of antibiotic if culture is negative and clinical course and other investigation safely rules out sepsis. References 1 .(Bang AT, Bang RA, Bactule SB, Reddy HM, Deshmukh MD. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet 1999;354:1955-61 2. Stoll BJ. The global impact of neonatal infection. Clin Perinatol 1997;24:1-21