metabolic syndrome can be associated with persistent storage
advertisement

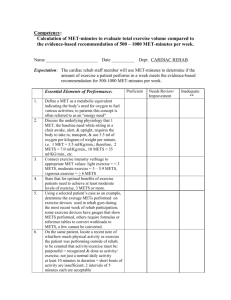
METABOLIC SYNDROME CAN BE ASSOCIATED WITH PERSISTENT STORAGE SYMPTOMS AFTER TREATMENT OF LUTS DUE TO BPH Matteo Salvi1 , Arcangelo Sebastianelli1 , Andrea Cocci1, Andrea Tubaro 2 ,Cosimo De Nunzio2, Linda Vignozzi3 , Mario Maggi3, Marco Carini1,Sergio Serni1, Mauro Gacci1. 1. Department of Urology, University of Florence, Careggi Hospital, Florence, Italy; 2. Department of Urology, Sant’Andrea Hospital, University ‘‘La Sapienza,’’ Rome, Italy 3. Department of Clinical Physiopathology, University of Florence, Florence, Italy INTRODUCTION Several preclinical and clinical evidences suggested the association between Metabolic Syndrome (MetS) and lower urinary tract symptoms (LUTS) due to benign prostatic enlargement (BPE). The aim of our study is to evaluate the impact of MetS components on urinary outcomes after surgical treatment for BPE. METHODS We evaluated a non-selected consecutive population of 378 men (mean age 68) surgically treated with simple open prostatectomy (OP) or transurethral resection of the prostate (TURP) for severe LUTS due to large BPE in two tertiary referral centers. Age, prostate volume (PV) and all MetS parameters (waist circumference [WC], Triglycerides, HDL cholesterol, blood pressure and fasting glucose), defined according to NCEP-ATPIII criteria, were recorded at recovery. LUTS were scored by total (tot-IPSS), voiding (voi-IPSS) and storage (sto-IPSS) IPSS: for all men data were recorded 3 months after surgery. Spearman’s correlation coefficient was used for univariate analyses, whereas multiple linear or logistic analysis were used for multivariate analyses, as appropriate. RESULTS Overall, 140 men (37.0%) satisfied MetS criteria. The improvement of Total and sto-IPSS postoperatively was related with surgical procedure, PSA and Waist circumference (WC). The number of MetS parameters were correlated with postoperative storage IPSS scores (adjusted r=0.162, p=0.008). Moreover, significant differences in delta tot-IPSS score and delta sto-IPSS score between men with or without MetS have been detected (63.2 vs. 81.7, p=0.015 and 19.6 vs. 63.6, p=0.013, respectively, see Figure 1). TURP and WC>102 cm were associated with an higher risk of an incomplete recovery of tot-IPSS (OR: 0.273, p=0.006; OR: 0.288, p=0.010) and Storage IPSS (OR: 0.206, p=0.002; OR: 0.149, p=0.001) as compared to OP and WC<102cm. TURP have the half of chance to achieve a complete recovery of voi-IPSS as compared with OP (OR: 0.55, p=0.000). DISCUSSION Men with MetS comorbid to LUTS, and, in particular those with WC≥ 102cm, showed worse urinary function recovery after any treatment for BPH. The storage symptoms were less decreased after TURP or OP in men with MetS and in particular in those with WC≥102. CONCLUSIONS The presence of MetS should be considered before surgery for LUTS/BPH, to improve MetS patient counseling.