Reviewer`s #1 report Title:In-Office Diagnostic Arthroscopy for Knee
advertisement

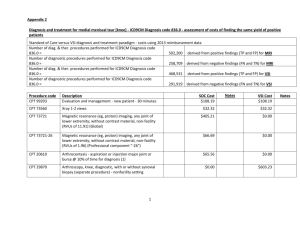
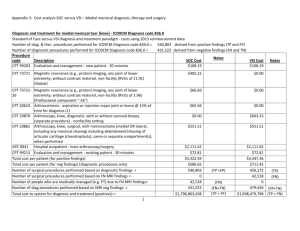
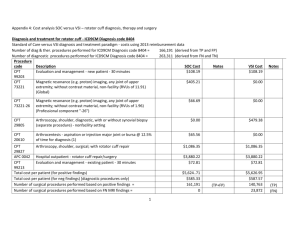
Reviewer's #1 report Title:In-Office Diagnostic Arthroscopy for Knee and Shoulder Intra-articular Injuries -Its Potential Impact on Cost Savings in the United States Version:1Date:9 November 2013 Reviewer:GEORGE PAPACHRISTOU Reviewer's report: According to the present authors, 3 new elements are issued with the present innovating approach: a. Costs reduction, b. Immediate answer to the question of trauma diagnosis, c. excludes FP and FN MRI findings. The proposed procedure is an optic diagnostic investigation of the inside of the examined joint without the use of a palpable instrument, like the probe. This method does not reassure the examiner that his approach is accurate as far as the elimination of FN or FP findings. Furthermore there are not included statistical elements concerning the accuracy of vision diagnostic procedure in comparison with standard arthroscopy. I am questioning also the safety of this diagnostic optic procedure as well as the visibility in cases of traumatic lesions with haemarthrosis as it is the present case, since only one portal is used without irrigation. The safety of the present procedure is identified in references 17-27 as noted in the manuscript. A summary of a recent study which has been submitted for publication on the accuracy of the VSI versus standard arthroscopy and MRI is attached. This information is confidential in nature and is not part of this manuscript. Lastly, based on the exclusion criteria from this study, patients with acute traumatic hemarthosis were not evaluated in this study. We have thus included language in the limitations section to reflect the fact that patients with acute hemarthrosis have not been evaluated with VSI (i.e. its safety and diagnostic capability with these patients) as of yet. Level of interest: An article of importance in its field Quality of written English: Acceptable Statistical review: No, the manuscript does not need to be seen by a statistician. Declaration of competing interests: I declare that I have no competing interests' Reviewer's report #2 Title:In-Office Diagnostic Arthroscopy for Knee and Shoulder Intra-articular Injuries -Its Potential Impact on Cost Savings in the United States Version:1Date:8 January 2014 Reviewer:Yanping Huang Reviewer's report: Major compulsory revisions: General comments: In this paper, the authors compare the use of MRI and VSI in reducing the cost for diagnosis and treatment of knee and shoulder pathologies. The conclusion is the use of VSI technique in replacing MRI could potentially save cost (about 5%) for the US health system. While this may be true from the analysis, the authors seemed to have neglected the discussion of another two important points when making the decision. The first one was that the analysis was based on 100% sensitivity and 100% specificity for the diagnosis using small bore arthroscopy (VSI). Although arthroscopy can be treated as the de fact golden standard in the diagnosis of joint pathology, they are certainly not perfect when used for joint disease diagnosis, such as internal tissue rather than surface damage or damage originating from the bone. Furthermore, the small view obtained from such small bore arthroscopy may limit its accuracy in diagnosis in a large joint. The second point is about the non-invasiveness of MRI compared to the minimally invasive VSI technique. For those patients with true pathology, the use of arthroscopy and surgery would be inevitable. However, for those negative patients (still a large proportion in the total number), I think most of them would prefer to use a non-invasive technique for screening purpose first. Cost is not the only factor that they need to consider. Patient would hesitate to do even a small surgery on their knee because of no true pathology. Therefore, these limitations should be discussed in the revision. 1) Abstract, Method: What is CY 2012? Calendar Year 2012? Give full name; CY 2012 has been changed in the abstract to Calendar Year 2012. VSI has been identified in the abstract as the VisionScope Imaging System. 2) Methods: the full names of “CPT”, “APC” and “DRG” should be given for first appearance; Current Procedural Terminology (CPT); Ambulatory Payment Classification (APC); Diagnostic Related Group (DRG) have been identified accordingly in the methods section. 3) Methods: No XRay diagnosis cost was seen in Appendix 3, please add and revise the table correspondingly with some mistakes in it; We have included Xray diagnostic cost (CPT 73650) @ $32.32 and as well, the cost of general anesthesia for a 45 minute hospital procedure (CPT 01440 @ $131.55) to both VSI and MRI diagnostic/therapeutic pathways for the knee. We have further included the cost of anesthesia for a shoulder arthroscopic procedure (@ $243.32). The anesthesia cost has also been included in Table 1 cost inputs. Based on these additions, Table 5 and 6 values have changed as well. Lastly, Appendix 3 and 4 values were also changed based on these additions. 4) Methods, “direct cost calculation”: “they represent a large portion of all arthroscopic knee (30%) and shoulder (35%) procedures”, give references/resources for these two percentage numbers; References #30 and #31included in reference section. Please also note that based on a review of the actual data, the percentages were changed to 32% for knee and 26% for shoulder. 5) Sup 2, Appendix 3: the difference of cost for diagnosis and treatment of MRI FP and NP patients was not analyzed, i.e., no chondroplasty procedure was included (CPT 29877), please revise properly. I think the authors need to double check the exact accuracy of Appendix 3 and Appendix 4 because currently there are quite a lot of mistakes seen; Thank you for the comments. We have doubled checked Appendix 3 and made adjustments per your suggestions. These changes are reflected in the manuscript and as well in Appendix 3. As well, Appendix 4 has also been fixed. 6) Sup 3, Appendix 4: at the end of the first part, add an additional line “Cost per patient diagnosis & treatment” as in Appendix 3; Added 7) With total cost of 2801 million for 0.972 million patients with knee pathology, the average cost per patient with MRI diagnosis was calculated as 5060? See direct cost was 2839. Also for other overall cost per patient. Seems much larger than the direct cost. Why? This reviewer was not quite understanding on how it was calculated for the overall cost per patient in addition to the direct cost. Please explain; Please note that the overall costs (direct treatment costs + direct treatment costs for complications) have been adjusted downward. The new numbers should make more sense. 8) Results: please give the original numbers of patients found in NSAS for ICD9CM code 836.0 and 840.4. How the patient number was obtained from the original data? An explanation on how these numbers were derived has been included in the results section. 9) Results: a percentage value in addition to absolute value better be given for the saving; We would prefer that percent overall savings not be included. 10) Discussion, 3rd paragraph: “not knowing exactly the patient’s condition based on MRI findings”, what do you mean by not knowing? Actually MRI diagnosis can be used for surgical preparation. Please rephrase this sentence; We have rephrased this sentence to read: The use of in-office arthroscopy may assist the physician in their preparation (based on better and more accurate information) for surgical intervention (when needed). 11) No need to use three tables (Table 5-7) for showing the data of total cost and saving. Compress space by combining these three tables into one; We have combined tables 5 & 6 into table 5 and renumbered table 7 to be table 6. We have also renumbered the tables within the manuscript. 12) For the References, consistently use full or abbreviated format for journals names (Journal of Bone and Joint Surgery or J Bone Joint Surg) and page numbers (115-7 or 115-117), but not mixed; This has been fixed throughout the reference section. Minor essential revisions: 1) Abstract, Results: delete “)” after “836.0”; Fixed 2) Abstract, Results: full name should be given for “VSI” when it appeared for the first time; Fixed 3) Abstract, Conclusions: “better prepare”; Fixed 4) Introduction, last third paragraph: it should be “arthrocentesis”; Fixed 5) Methods, “Direct cost calculation”, next: add a “)” after “rotator cuff”; Fixed 6) Methods, “for the shoulder”, next two paragraphs: moving “existing patient” to “CPT 99213 -E&M”; Please note that there are two CPT codes for evaluation and management – CPT 99203 which is an E&M for a new patient and CPT 99213 which is an E&M for an existing patient. We have however removed “existing patient” from the CPT 99213 description. 7) Results: subtitles, use either “arthroscopy” or “arthroscopies” consistently; Fixed 8) Table 2, title: “cost applied to knee arthroscopy”; Fixed 9) Sup 1, Appendix 2: title, delete “with,” in “followed up with”; Fixed 10) Sup 1, Appendix 2: “arthroscopy procedure”; Fixed 11) Sup 1, Appendix 2: is it “2012” or 2006 for the knee data? It is 2012 and has been fixed 12) Sup 2, “Number of people who are medically managed (e.g. PT) due to FN MRI findings=”: “43,518” rather than “42,518” based on Sup 1; Number should be 42,518 13) Sup 2, CPT 20610: “10% of time”; Fixed 14) Sup 2, Cost per patient for medical management [PT](10.3 sessions over 6 wks); Fixed 15) Sup 2, Costs for patients under physical therapy post surgery for TP, FP, and FN CO results; Fixed 16) Sup 2: thromboembolism; Fixed 17) Sup 3: Number of surgical procedures performed based on positive findings =, 166,191; Fixed 18) Sup 3: Number of patients who crossed over CO) to surgery in FN group =, not copyright “c”; Fixed 19) Please make sure all the codes are consistent. Done Level of interest: An article of limited interest Quality of written English: Needs some language corrections before being published Statistical review: No, the manuscript does not need to be seen by a statistician. Declaration of competing interests: I declare that I have no competing interests