Nephrolithiasis, Acute Renal Colic - Dis Lair

Nephrolithiasis, Acute Renal Colic
Introduction
Acute renal colic is probably the most excruciatingly painful event a person can endure. Striking without warning, the pain is often described as being worse than childbirth, broken bones, gunshot wounds, burns, or surgery. Renal colic affects approximately 1.2 million people each year and accounts for approximately 1% of all hospital admissions. Most active emergency departments (EDs) treat an average of at least one patient with acute renal colic every day depending on the hospital's patient population. The ED physician is often the first to see and evaluate these patients. While proper diagnosis, prompt initial treatment, and appropriate consultations are clearly the primary responsibility of the emergency physician, substantial patient education, including preventive therapy program options, should also be started in the ED.
Background
The overall lifetime rate of kidney stones in the general population is approximately 12% for men and 4% for women.
Having a family member with a history of stones doubles these rates. Approximately 30 million people are at risk in the
United States. Peak incidence occurs in people aged 35-45 years, but the disease can affect anyone at any age. Initial stones in elderly people and in children are relatively uncommon; however, consider kidney stones whenever acute back or flank pain is encountered, regardless of patient age. When stones occur in persons in these uncommon age groups, a metabolic workup consisting of a 24-hour urine collection and appropriate serum laboratory testing is recommended.
The increasing incidence of kidney stone disease in the
United States seems to be related to the socioeconomic status of the patient population. The lower the economic status, the lower the likelihood of renal stones. Other parts of the world with lower standards of living tend to have lower incidences of kidney stones but have higher rates of bladder calculi. Black people have a lower incidence of stones than white people, and people living in the South and
Southwest have higher incidences of stones than people living in other parts of the United States.
Renal failure and stones
While nephrolithiasis is not a common cause of renal failure, certain problems, such as preexisting azotemia and solitary functional kidneys, clearly present a higher risk of additional renal damage. Other high-risk factors include diabetes and struvite staghorn calculi and various hereditary diseases such as primary hyperoxaluria, Dent disease, cystinuria, and polycystic kidney disease. Spinal cord injuries and similar functional or anatomical urological anomalies also predispose patients with kidney stones to an increased risk of renal failure. Recurrent obstruction, especially when associated with infection and tubular epithelial or renal interstitial cell damage from microcrystals, may activate the fibrogenic cascade, which is mainly responsible for the actual loss of functional renal parenchyma.
In emergent settings in which concern exists about possible renal failure, the focus of treatment should be on correcting dehydration, treating urinary infections, preventing scarring, identifying patients with a solitary functional kidney, and reducing risks of acute renal failure from contrast nephrotoxicity, particularly in patients with preexisting azotemia (creatinine >2 mg/dL), diabetes, dehydration, or multiple myeloma. Adequate intravenous hydration is essential to minimize the nephrotoxic effects of intravenous contrast agents. Choosing imaging studies that do not require intravenous contrast (eg, ultrasound, abdominal flat plate radiographs, noncontrast CT scans) is wise, especially in patients at increased risk for developing renal failure.
Clinical Aspects of Acute Renal Colic
Predicting spontaneous stone passage
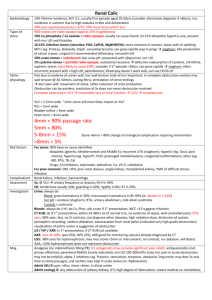
In general, smaller stones are more likely to pass spontaneously, but stone passage also depends on the exact shape and location of the stone and the specific anatomy of the upper urinary tract in the particular individual. For example, the presence of a ureteropelvic junction (UPJ) obstruction or a ureteral stricture could make passing even very small stones difficult or impossible. If the stone is 4 mm or smaller, the stone is eventually passed 90% of the time.
Stones 5-7 mm generally have a 50% chance of passing spontaneously. Calculi larger than 7 mm are unlikely to pass unassisted. However, nothing is more difficult in managing an acute kidney stone attack than predicting what will happen with the stone. Most experienced ED physicians and urologists have observed very large stones passing and some very small stones that do not move.
Diagnosis
The diagnosis is often made based on clinical symptoms alone, although confirmatory tests are usually performed. At this point, the goals and opinions of physicians in different specialties diverge. From the point of view of the ED physician, making the diagnosis of a renal or ureteral stone and excluding appendicitis or abdominal aortic aneurysm is sufficient. A urologist, who must ultimately make the decision about possible surgery, may require additional information. Before such a decision can be made, a urologist must know the exact size, shape, orientation, radiolucency, composition, and location of the stone and must know about overall kidney function, the presence of any infection, and other clinical information.
Clinical findings
The classic presentation for a patient with acute renal colic is the sudden onset of severe pain originating in the flank and radiating inferiorly and anteriorly. The pain is usually, but not always, associated with microscopic hematuria, nausea, and vomiting. The patient usually exhibits considerable costovertebral angle tenderness, but the rest of the examination findings are often unremarkable. Unlike patients
with an acute abdomen, who usually try to lie absolutely still, patients with renal colic tend to move constantly, seeking a more comfortable position. (However, patients with pyonephrosis also tend to remain motionless.)
Approximately 85% of all patients with renal colic demonstrate at least microscopic hematuria, which means that 15% of all patients with kidney stones do not have hematuria. Lack of hematuria alone does not exclude the diagnosis of acute renal colic. Tachycardia and hypertension are relatively common in these cases, even in patients with no prior personal history of abnormal cardiac or blood pressure problems.
The presence of pyuria, fever, leukocytosis, or bacteriuria suggests the possibility of a urinary infection and the potential for an infected obstructed renal unit or pyonephrosis. Such a condition is potentially life
threatening and should be treated as a surgical emergency.
In patients who are floridly septic or hemodynamically unstable, a percutaneous nephrostomy is a faster and safer way to establish drainage of an infected and obstructed kidney. Retrograde approaches to drainage require more sedation and anesthetic and may cause reflux of infected material from the ureter into the kidney and may exacerbate the infection. Retrograde endoscopy in these situations, if used at all, should be reserved for relatively mild cases in which patients are medically stable. Use appropriate urine cultures and antibiotics whenever a urinary infection is suspected in conjunction with hydronephrosis or renal colic.
Renal Colic Pain
The colicky-type pain known as renal colic usually begins in the upper lateral mid back over the costovertebral angle and occasionally subcostally. It radiates inferiorly and anteriorly toward the groin. The pain generated by renal colic is primarily caused by the dilation, stretching, and spasm caused by the acute ureteral obstruction. (When a severe but chronic obstruction develops, as in some types of cancer, it is usually painless.)
Colic is a misnomer because renal colic pain tends to remain constant, whereas intestinal or biliary colic is usually somewhat intermittent and often comes in waves. The pattern of the pain depends on the individual's pain threshold and perception and on the speed and degree of the changes in hydrostatic pressure within the proximal ureter and renal pelvis. Ureteral peristalsis, stone migration, and tilting or twisting of the stone with subsequent intermittent obstructions may cause exacerbation or renewal of the renal colic pain. The severity of the pain depends on the degree and site of the obstruction, not on the size of the stone. A patient can often point to the site of maximum tenderness, which is likely to be the site of the ureteral obstruction.
A stone moving down the ureter and causing only intermittent obstruction actually may be more painful than a stone that is motionless. A constant obstruction, even if high grade, allows for various autoregulatory mechanisms and reflexes, interstitial renal edema, and pyelolymphatic and pyelovenous backflow to help diminish the renal pelvic hydrostatic pressure, which gradually helps reduce the pain.
The interstitial renal edema produced stretches the renal capsule, enlarges the kidney (ie, nephromegaly), and increases renal lymphatic drainage. (Increased capillary permeability facilitates this edema.) It may also reduce the radiographic density of the affected kidney's parenchyma when viewed on a noncontrast CT scan.
Distension of the renal pelvis initially stimulates ureteral hyperperistalsis, but this diminishes after 24 hours, as does renal blood flow. Peak hydrostatic renal pelvis pressure is attained within 2-5 hours after a complete obstruction.
Within the first 90 minutes of a complete ureteral obstruction, afferent preglomerular arteriolar vasodilation occurs, which temporarily increases renal blood flow.
Between 90 minutes and 5 hours after the obstruction, renal blood flow starts to decrease while intraureteral pressure continues to rise. By 5 hours after a complete obstruction, both renal blood flow and intraluminal ureteral pressure decrease on the affected side. Renal blood flow decreases to approximately 50% of normal baseline levels after 72 hours, to 30% after 1 week, to 20% after 2 weeks, and to 12% after
8 weeks. By this point, intraureteral pressures have returned to normal, but the proximal ureteral dilation remains and ureteral peristalsis is minimal.
Interstitial edema of the affected kidney actually enhances fluid reabsorption, which helps to increase the renal lymphatic drainage to establish a new, relatively stable, equilibrium. At the same time, renal blood flow increases in the contralateral kidney as renal function decreases in the obstructed unit.
In summary, by 24 hours after a complete ureteral obstruction, the renal pelvic hydrostatic pressure has dropped because of (1) a reduction in ureteral peristalsis; (2) decreased renal arterial vascular flow, which causes a corresponding drop in urine production on the affected side; and (3) interstitial renal edema, which leads to a marked increase in renal lymphatic drainage. Additionally, as the ureter proximal to the stone distends, some urine can sometimes flow around the obstruction, relieving the proximal hydrostatic pressure and establishing a stable, relatively painless equilibrium. These factors explain why severe renal colic pain typically lasts less than 24 hours in the absence of any infection or stone movement.
Experimental studies in animals have suggested that renal damage may begin within 24 hours of a complete obstruction and permanent kidney deterioration starts within 5-14 days.
While some practitioners wait several months for a stone to pass in an asymptomatic patient, others argue that permanent damage is occurring as long as intervention is delayed. Based on personal experience and anecdotal cases, the author recommends waiting no longer than 4 weeks for a stone to pass spontaneously before considering intervention.
Convincing asymptomatic patients of the need for surgical intervention may be difficult in the absence of a clear consensus in the urological community about the length of time to wait before surgical stone removal, fragmentation, or bypass.
If only a partial obstruction is present, the same changes occur, but to a lesser degree and over a longer period.
Proximal ureteric and renal pelvic hydrostatic pressures tend to remain elevated longer, and ureteral peristalsis does not diminish as quickly. If the increased pressure is sufficient to establish a reasonable flow beyond the obstructing stone, glomerular filtration and renal blood flow approximates reference range baseline levels, although pain may be ongoing.
Phases of the Acute Renal Colic Attack
The actual pain attack tends to occur in somewhat predictable phases, with the pain reaching its peak in most patients within 2 hours of onset. The pain roughly follows the dermatomes of T-10 to S-4. The entire process typically lasts
3-18 hours. Renal colic has been described as having 3 clinical phases.
Acute, or onset, phase
The typical attack starts early in the morning or at night, waking the patient from sleep. When it begins during the day, patients most commonly describe the attack as starting slowly and insidiously. The pain is usually steady, increasingly severe, and continuous; some patients experience intermittent paroxysms of even more excruciating pain. The pain level may increase to maximum intensity in as little as
30 minutes after initial onset or more slowly, taking up to 6 hours or longer to peak. The typical patient reaches maximum pain 1-2 hours after the start of the renal colic attack.
Constant phase
Once the pain reaches maximum intensity, it tends to remain constant until it is either treated or allowed to diminish spontaneously. The period of sustained maximal pain is called the constant phase of the renal colic attack. This phase usually lasts 1-4 hours but can persist longer than 12 hours in some cases. Most patients arrive in the ED during this phase of the attack.
Abatement or relief phase
During this final phase, the pain diminishes fairly quickly, and patients finally feel relief. Relief can occur spontaneously at any time after the initial onset of the colic. Patients may fall asleep, especially if they have been administered strong analgesic medication. Upon awakening, the patient notices that the pain has disappeared. This final phase of the attack most commonly lasts 1.5-3 hours.
Pain in Renal Colic
Renal pain fibers are primarily preganglionic sympathetic nerves that reach spinal cord levels T-11 to L-2 through the dorsal nerve roots. Aortorenal, celiac, and inferior mesenteric ganglia are also involved. Spinal transmission of renal pain signals occurs primarily through the ascending spinothalamic tracts. In the lower ureter, pain signals are also distributed through the genitofemoral and ilioinguinal nerves. The nervi erigentes, which innervates the intramural ureter and bladder, is responsible for some of the bladder symptoms that often accompany an intramural ureteral calculus.
1.
Upper ureter and renal pelvis: Pain from upper ureteral stones tends to radiate to the flank and lumbar areas. On the right side, this can be confused with cholecystitis or cholelithiasis; on the left, the differential diagnoses include acute pancreatitis, peptic ulcer disease, and gastritis.
2.
Middle ureter: Midureteral calculi cause pain that radiates anteriorly and caudally. This midureteral pain in particular can easily mimic appendicitis on the right or acute diverticulitis on the left.
3.
Distal ureter: Distal ureteral stones cause pain that tends to radiate into the groin or testicle in the male or labia majora in the female because the pain is referred from the ilioinguinal or genitofemoral nerves. If a stone is lodged in the intramural ureter, symptoms may appear similar to cystitis or urethritis. These symptoms include suprapubic pain, urinary frequency, urgency, dysuria, stranguria, pain at the tip of the penis, and sometimes various bowel symptoms, such as diarrhea and tenesmus. These symptoms can be confused with pelvic inflammatory disease, ovarian cyst rupture, or torsion and menstrual pain in women.
Most of the pain receptors of the upper urinary tract responsible for the perception of renal colic are located submucosally in the renal pelvis, calices, renal capsule, and upper ureter. Acute distention seems to be more important in the development of the pain of acute renal colic than spasm, local irritation, or ureteral hyperperistalsis.
Stimulation of the peripelvic renal capsule causes flank pain, while stimulation of the renal pelvis and calices causes typical renal colic. Mucosal irritation can be sensed in the renal pelvis to some degree by chemoreceptors, but this irritation is thought to play only a minor role in the perception of renal or ureteral colic.
In the ureter, an increase in proximal peristalsis through activation of intrinsic ureteral pacemakers may contribute to the perception of pain. Muscle spasm, increased proximal peristalsis, local inflammation, irritation, and edema at the site of obstruction may contribute to the development of pain through chemoreceptor activation and stretching of submucosal free nerve endings.
Nausea and vomiting are often associated with acute renal colic and occur in at least 50% of patients. Nausea is caused by the common innervation pathway of the renal pelvis, stomach, and intestines through the celiac axis and vagal nerve afferents. This is often compounded by the effects of narcotic analgesics, which often induce nausea and vomiting through a direct effect on GI motility and through an indirect
effect on the chemoreceptor trigger zone in the medulla oblongata. Nonsteroidal anti-inflammatory drugs (NSAIDs) can often cause gastric irritation and GI upset.
The presence of a renal or ureteral calculus is not a guarantee that the patient does not have some other,
unrelated medical problem causing the GI symptoms.
Acute onset of severe flank pain radiating to the groin, gross or microscopic hematuria, nausea, and vomiting not associated with an acute abdomen are symptoms that most likely indicate renal colic caused by an acute ureteral or renal pelvic obstruction from a calculus. Renal colic pain rarely, if ever, occurs without obstruction.
In some cases, a stone may pass before the definitive imaging procedure has been completed. In these cases, residual inflammation and edema still may cause some transient or diminishing obstruction and pain even without any stone being positively identified.
Nerve Blocks
Nerve blocks have been used successfully in both the diagnosis and treatment of renal colic, although they are more helpful in chronic than in acute cases. Intercostal nerve blocks can be used to differentiate pain from chondritis, neuromas, and radiculitis from true renal pain. This is achieved by injecting an anesthetic agent, such as lidocaine, around the 11th or 12th intercostal nerve proximal to the site of the pain at a time when the patient is experiencing pain. If the injection causes abolition of the pain, a peripheral nerve or musculoskeletal etiology is suggested. Subsequent injections of various agents to produce neurolysis (eg, 10% phenol or 100% absolute alcohol) have been tried but often result in an intolerable denervation-related discomfort.
In the mid 1950s, a study was reported in which 51 patients with documented renal colic were successfully treated for pain using only a unilateral posterior splanchnic nerve block.
Complete relief from pain, nausea, and vomiting was reported in all 51 patients treated.
1
Urinalysis
Microscopic examination of the urine is a critical part of the evaluation of a patient thought to have renal colic. Gross or microscopic hematuria is only present in approximately 85% of cases. The lack of microscopic hematuria does not eliminate renal colic as a potential diagnosis. In addition to a dipstick evaluation, always perform a microscopic urinalysis in these patients.
Pay attention to the presence or absence of leukocytes, crystals, and bacteria and to the urinary pH. In general, if the number of WBCs in the urine is greater than 10 cells per highpower field or greater than the number of RBCs, suspect a urinary tract infection (UTI). Determining urinary pH also helps because, (1) with a pH lower than 6.0, a uric acid stone should be considered, and (2) with a pH greater than 8.0, an infection with a urea-splitting organism such as Proteus,
Pseudomonas, or Klebsiella is likely. Urinary crystals of calcium oxalate, uric acid, or cystine may occasionally be found upon urinalysis. When present, these crystals are very good clues to the underlying type and nature of any obstructing calculus.
While mild leukocytosis often accompanies a renal colic attack, a high index of suspicion for a possible infection should accompany any serum WBC count of 15,000/µL or higher in a patient presenting with an apparent acute kidney stone attack, even if afebrile.
Imaging Studies
Flat Plate Radiograph of the Abdomen or Plain Abdominal
Film
The historical cornerstone of any evaluation of abdominal pain that could be a stone is a flat plate radiograph of the abdomen or kidneys, ureters, and bladder (KUB), which has been used for this purpose since 1896. All urinary calculi may not always be visible on the KUB radiograph because of their small size, stone radiolucency, or overlying gas, stool, or bone. The stones that are observed can be correlated with opacities found on other studies for identification and tracking progress.
Many calcifications observed on the KUB radiograph are phleboliths, vascular calcifications, calcified lymph nodes, appendicoliths, granulomas, various calcified masses, or even bowel contents. All can be confused with urinary tract calculi.
Also, the insoluble radiopaque carrier for osmotically controlled-release oral system (OROS) pharmaceuticals can sometimes be mistaken for urinary calculi on KUB radiographs. (The OROS, developed by Alza Pharmaceuticals, is designed for once-daily dosing of various medications, including methylphenidate [Concerta], oxybutynin [Ditropan
XL], doxazosin [Cardura XL], verapamil [Covera-HS], and prazosin [Minipress].)
The flat plate radiograph uses the same orientation and anatomical presentation that is observed on fluoroscopy images and retrograde pyelograms or during endoscopic ureteral surgery, such as ureteroscopy or intracorporeal lithotripsy. Even if a stone is not visible on a flat plate radiograph, the calculus could be a radiolucent uric acid stone that can be dissolved with alkalinizing medication. Such a stone is more likely if the urine pH indicates very acidic urine.
In practice, any patient with symptoms of acute renal colic who demonstrates a urine pH lower than 6.0 should be considered at risk for a possible uric acid stone and should have a KUB radiograph performed to help determine radiolucency.
The flat plate radiograph is inexpensive, quick, and usually helpful even if no specific stone is observed. It is extremely useful in following the progress of previously documented radiopaque calculi and checking the position of any indwelling double-J stents. The KUB radiograph can suggest the fluoroscopic appearance of a stone, which determines whether it can be targeted with extracorporeal shockwave lithotripsy (ESWL). The KUB radiograph is also quite accurate
for helping determine the exact size and shape of a visible radiopaque stone, which can only be estimated using a CT scan alone because the x-ray beam of the CT scan does not always cross the stone at its widest point.
Differentiation between a phlebolith and an obstructing calcific stone becomes easier when the KUB radiograph demonstrates a lucent center, identifying the calcification as a phlebolith. This central lucency is not observed as often on
CT scans. For these reasons, many urologists recommend the flat plate radiograph in addition to CT scan for any renal colic–type scenario.
A number of studies have suggested that the flat plate has a relatively low sensitivity and specificity for renal and ureteral calculi. Many patients have numerous pelvic calcifications that make pinpointing specific stones difficult. Any calcific density observed on a KUB radiograph that happens to overlie the course of the ureter is not guaranteed to be a stone. A number of emergency physicians argue that the flat plate radiograph adds little to the identification and treatment of a stone in the ED. Furthermore, obtaining a flat plate radiograph may cause delays, may unnecessarily increase the cost of the workup, and causes additional patient radiation exposure. Consequently, the flat plate radiograph is no longer uniformly required in the modern era, now that unenhanced CT scans are the criterion standard for diagnosis of acute renal colic.
A large clinical study from Johns Hopkins University in 2000 by Jackman and associates concluded "plain abdominal x-ray is more sensitive than scout CT for detecting radiopaque nephrolithiasis.
2 Of the stones visible on plain abdominal xray, 51% were not seen on CT. To facilitate outpatient clinic follow-up of patients with calculi, plain abdominal x-rays should be performed." Many urologists, including this author, recommend that in addition to other studies (eg, noncontrast helical or spiral CT scans), a KUB radiograph be obtained in all patients with a clinical presentation of acute flank pain suggestive of renal colic. Knowing the exact size and shape of a stone, its position, fluoroscopic appearance, surgical orientation, and relative radiolucency is an advantage. Also, the progress of the stone can be easily monitored with a follow-up flat plate radiograph. These advantages far outweigh the few disadvantages associated with performing the examination.
A reasonable practical compromise has been suggested that would require the KUB only in cases in which the CT scan indicates ureteral or renal calculi. This would avoid the cost and radiation exposure in patients who do not actually have stones. Additionally, the digital CT scout radiograph can be used as a reasonable substitute for the KUB radiograph if cost factors, excessive delays, or logistical problems make obtaining a formal abdominal flat plate study difficult.
Renal Ultrasound
Ultrasound is fast, easy, safe, and relatively inexpensive to perform. Ultrasound requires no intravenous contrast and can easily detect any significant hydronephrosis, although this must be differentiated from UPJ obstruction and an extrarenal pelvis. Ultrasound cannot be used to find small stones (ie, £5 mm) and does not help in the evaluation of kidney function. A large extrarenal pelvis or UPJ obstruction can easily be misread for hydronephrosis if ultrasound alone is used.
For some stones, ultrasound works quite well; however, in general, the test is less useful for diagnosing ureteral calculi than other modalities. Middleton et al reported perhaps the most successful use of ultrasound for renal colic in 1988 (ie, a stone detection rate of 91%). Most authors report detection rates of approximately 30%. The unusually high reported success rate achieved by Middleton et al can be explained in part by the fact that a radiologist specializing in ultrasound performed the studies, which typically required at least 15-20 minutes to complete. The success of diagnostic ultrasound is very dependent on operator skill and experience, which is probably demonstrated by the unique setting in which their study was performed.
3
Renal ultrasound works best in the setting of relatively large stones within the renal pelvis or kidney and sometimes at the
UPJ. Whether the stones are radiolucent or opaque does not matter because an ultrasound picture is based strictly on density, not on calcium content. Ultrasound is a good way to monitor known stones after medical or surgical therapy if the stones are large enough to be detected by this modality and are in a suitable position. Ultrasound can also be used to check the abdomen for a possible abdominal aortic aneurysm or cholelithiasis, which can sometimes be mistaken for acute renal colic. It is also useful in differentiating filling defects observed on contrast studies because stones are much more echogenic than tumors, clots, or tissue. Ultrasound is the initial imaging modality of choice for patients with acute renal colic who are pregnant because it avoids all potentially hazardous ionizing radiation.
Ultrasound relies on indirect visualization clues to identify stones. Differentiating an extrarenal pelvis from an obstructed one is sometimes difficult when using ultrasound alone. Intermittent obstruction or mild hydronephrosis can be easily missed with ultrasound, and, with the few exceptions mentioned above, it generally does not provide much information about most other disease processes capable of causing acute flank pain.
Sometimes, a KUB abdominal flat plate radiograph is used in addition to the ultrasound to help identify and monitor suspected stones, especially if renal dilation is detected. As with the KUB radiograph alone, any density detected along the expected course of the ureter is not guaranteed to be an actual stone within the collecting system.
Combining a renal ultrasound with an abdominal flat plate radiograph has been proposed as a reasonable initial evaluation protocol when a CT scan cannot be performed or is unavailable. Ultrasound has reasonably good sensitivity for
detection of other sources of abdominal pain, such as cholelithiasis and abdominal aortic aneurysms. When combined with the KUB radiograph, ultrasound can quickly and inexpensively provide substantial information about the urinary tract without the risk of contrast nephrotoxicity or hypersensitivity. Intravenous pyelograms (IVPs) can then be limited to those patients for whom additional information is required for a diagnosis or for whom the etiology of the pain remains unclear.
The intrarenal resistive index, as measured on Doppler studies, has been proposed as one way to diagnose acute renal obstruction using ultrasound. Elevation of the resistive index on the affected side, compared with the opposite healthy kidney, is evidence of obstruction. However, intrarenal resistive index does not identify partial or intermittent obstructions and is less helpful in the early phase of even complete ureteral blockage. It also does not provide any information about the radiolucency, size, shape, or position of any stone and cannot be used to differentiate between intrinsic and extrinsic urinary obstructions.
Pyelosinus extravasation or fornix rupture, which occurs in up to 20% of patients with acute ureteral obstructions, leads to a loss of dilation and may be responsible for false-negative findings from studies. Other nonobstructive renal problems, such as renal failure, diabetic nephropathy, and renal compression, can affect the readings.
Under normal conditions, renal vascular resistance is relatively low and renal blood flow is excellent throughout the cardiac cycle, with a reasonable flow continuing even during diastole. During conditions associated with increased vascular resistance, such as an acute ureteric obstruction, the measured decrease in renal blood flow during diastole is proportionately greater than the decrease during systole.
The resistive index is calculated as peak systolic velocity minus end-diastolic velocity divided by the peak systolic velocity. An elevated resistive index of 0.7 or more is considered indicative of an acute ureteral obstruction. A change in the resistive index between the affected and contralateral (healthy) kidney of 0.04 or more also suggests a ureteral obstruction. (The affected kidney has the higher resistive index value.) This study may be particularly useful in pregnancy (when exposure to ionizing radiation must be minimized), severe contrast media allergy, and azotemia. For best results, measure the intrarenal resistive index during a pain attack but before any NSAIDs or other anti-inflammatory medications are administered.
Considering that up to perhaps 35% of patients with documented acute ureteral obstruction do not demonstrate any significant hydroureteronephrosis, the use of a noninvasive study such as Doppler ultrasound and intrarenal resistive index, which does not depend on visual ureteral or renal pelvic dilation, may eventually prove very useful. For now, additional studies on this technique are needed before intrarenal resistive index can be reliably used for diagnosing acute renal colic and ureteric obstruction.
Nuclear Renal Scans
A nuclear renal scan can be used to objectively measure differential renal function, especially in a dilated system for which the degree of obstruction is in question. This is also a reasonable study in pregnant patients, in whom radiation exposure must be limited.
Technetium Tc 99m (diethylene triamine pentaacetic acid) is the radioisotope used. It is eliminated from the body almost exclusively by glomerular filtration. The rate of clearance from the renal unit provides an excellent estimate of the glomerular filtration rate and the relative rate of drainage or clearing from each kidney. A drainage half-time that is 20 minutes or longer indicates obstruction, while a drainage half-time of 10 minutes or less is considered unobstructed. If the drainage half-time is 10-20 minutes, the result is indeterminate.
Plain Renal Tomography
Observing even a relatively large radiopaque stone located in the kidney or renal pelvis on a standard abdominal flat plate radiograph can be difficult or impossible if the patient has abundant gas or stool overlying the area. This can be overcome using noncontrast or plain renal tomography.
Renal tomography requires moving the radiograph projector and film in such a way that a zone of photographic clarity is positioned at the stationary focus point of the radiograph beam. All other overlying material is eliminated on this type of radiograph. The focal point is adjusted along the anteroposterior axis a distance of 1 cm, and the radiograph procedure is repeated. Usually, a series of 4-6 films is needed to completely image both kidneys. Remember that if such a series of films is needed, it should be obtained before any intravenous contrast is administered; contrast obscures any stones present.
Plain renal tomography is most useful when checking for small stones that might be present in the kidney before starting a preventive therapy plan or when differentiating intrarenal calcifications that are likely to be stones from extrarenal opacities that are clearly not renal calculi.
Intravenous Pyelogram
The IVP, or urogram, was the criterion standard for the detection and diagnosis of renal and ureteral calculi from
1927, when Swick first described it, until it was recently displaced by the unenhanced CT scan. The contrast agents used most since 1952 were iodinated benzoic acid derivatives until less allergenic nonionic agents were introduced in the
1980s. Various reactions have been attributed to intravenous contrast agents, including nausea, vomiting, urticaria, bronchospasm, cardiac arrhythmias, seizures, direct nephrotoxicity (especially in dehydrated or azotemic patients), and anaphylaxis.
The main advantage of the IVP is the clear outline of the entire urinary system that it provides, making visualization of
even mild hydronephrosis relatively easy. This effect is enhanced by the osmotic diuretic effect of the contrast medium. When a patient has multiple pelvic calcifications, identifying the actual stone is simple with the IVP. IVP can also show nonopaque stones as filling defects. Disadvantages include the need for intravenous contrast material, which may provoke an allergic response or renal failure, and the need for multiple delayed films, which can take hours. The delayed films take time because the contrast material passes quite slowly into the blocked renal unit and ureter. Filming continues until the entire distal ureter is visible, which contributes to an increased radiation dose to the patient.
The dose of intravenous contrast is usually approximately 1 mL/kg. The bolus method of intravenous contrast administration is usually recommended for renal colic evaluations because it allows for a nephrogram-effect phase film. This normally occurs within the first minute after bolus contrast injection and cannot be obtained with the slow-drip infusion technique. Acute ureteral obstruction causes an intense persistent finding on nephrograms, caused by an increase in the intrarenal concentration of the contrast media. This may take several hours or more to fully visualize, which necessarily delays completion of the study.
Flat plate radiographs are obtained immediately before contrast administration and at 1, 5, 10, and 15 minutes afterwards or until visible contrast material fills both ureters.
Prone films are sometimes obtained to enhance visualization of the ureters. When the bladder is full of contrast and the distal ureters contain sufficient contrast for visualization, the patient is asked to void; then a postvoid film is taken.
Sometimes, oblique views are needed when bone or bowel contents overlie the area of interest.
Contrast-induced nephropathy is the third leading cause of hospital-acquired acute renal failure. A serum creatinine level of more than 2 mg/dL is a relative contraindication to the use of intravenous contrast agents. Patients with azotemia, multiple myeloma, pregnancy, or diabetes, especially if dehydrated, are particularly susceptible to acute contrast nephropathy which is defined as a 25% or greater increase in serum creatinine levels within 2-3 days of intravenous contrast exposure. Ischemia, direct intracellular high– contrast-concentration toxicity and free-radical injury are thought to be the causative mechanisms of contrast-induced nephropathy.
Low osmolarity or iso-osmolar contrast may help to reduce the risk of contrast-induced nephropathy. A renal vasodilator
(fenoldopam mesylate [Corlopam]) has been used to minimize renal complications in higher-risk patients requiring intravenous contrast studies who would otherwise be at high risk for azotemia. Fenoldopam is a dopamine type 1A agonist that has been shown to increase renal plasma flow and to help prevent contrast nephropathy. Theophylline and Nacetylcysteine have also been used with some success, but the standard prophylactic therapy is intravenous saline at a rate of 1-3 mL/kg/h. Hemodialysis before and after intravenous contrast can also be used to minimize renal toxicity, but such a regimen is costly and too cumbersome for general use except in special high-risk situations.
A randomized study by Merten and colleagues from
Charlotte, NC, published in JAMA in 2004 compared the standard intravenous saline hydration prophylaxis with a
154-mEq/L sodium bicarbonate solution. Identical volumes of each solution were used. They found a substantial benefit in the sodium bicarbonate–treated group compared with the sodium chloride–treated cohort. Patients treated with prophylactic sodium chloride hydration were 8 times more likely to develop nephropathy after contrast exposure than the patients treated with sodium bicarbonate. Such a treatment plan is practical, inexpensive, simple, safe, and effective, and the author now recommend sodium bicarbonate intravenous hydration as the prophylactic treatment of choice for prevention of contrast-induced nephropathy.
4
Serious allergic reactions to intravenous contrast occur in
0.1-0.2% of patients. Pretreatment with steroids, antihistamines, and H1 and H2 blockers can further reduce the likelihood of severe allergic reactions, especially if administered several hours prior to the study. Nonionic contrast media is more expensive but less likely to provoke an allergic response than the older ionic media, especially if the patient has a history of mild or moderate allergic reactions to contrast or injected dye.
A history of asthma or multiple drug allergies should also suggest the use of a nonionic agent. Many institutions currently use only the nonionic agent for all intravenous contrast studies, despite the added cost, because of the increased safety it provides. Glucophage (Metformin) should be discontinued at least 1 day before any intravenous contrast study, particularly in patients with proven or borderline azotemia, because of the risk of worsening renal function and the rare development of potentially lifethreatening lactic acidosis. The medication can be resumed
48 hours after the contrast study if renal function has normalized.
Some urologists prefer the IVP to other imaging studies in the initial evaluation of possible ureteral stones because the size, shape, and position of any calculi are usually very clear and the orientation of the studies is very familiar because it is identical to the types of radiographs performed in endoscopic stone surgeries and shockwave lithotripsy.
Another advantage is that IVPs demonstrate renal function and allow for verification that the opposite kidney is functioning normally. Typically, an IVP finding positive for a ureteral stone shows a delayed nephrogram effect and columnization. The ureter is peristaltic so the entire ureter is not usually visualized on a single film except when an obstruction is present, such as from a stone. Even without observing any specific stone, the presence of a nephrogram
effect in one kidney with normal function of the opposite kidney is highly suggestive, but not diagnostic, of ureteral obstruction.
Extravasation of contrast around the collecting system may be a sign of a ruptured fornix, while pyelolymphatic backflow indicates that contrast has entered into the renal lymphatic drainage system. Both are considered signs of a more severe ureteric obstruction. However, no published study has indicated that the clinical course, treatment outcome, or residual renal damage is altered in any way in these patients.
In fact, this information about the radiological assessment of the relative severity of the obstruction rarely affects clinical treatment decisions, except perhaps in persons with solitary kidneys.
Medullary sponge kidney
Generally, only an IVP provides sufficient detail to diagnose medullary sponge kidney (MSK), also called tubular or ductal ectasia or cystic dilation of the collecting ducts. While Beitzke first described the condition in 1908, the characteristic radiographic features were not recognized until 1939, by
Lenarduzzi. MSK is generally a benign congenital condition that demonstrates dilation of the distal renal collecting tubules on IVP as the tubules fill with contrast. These normally invisible microscopic tubules show a whitish blush in the papilla in persons with MSK. In severe cases, stones, cysts, and diverticula can be present. The condition is bilateral in 70% of patients and is usually not discovered until the second or third decade of life, even though MSK is congenital.
The most accurate way to demonstrate MSK has been described as high-quality excretory urography (ie, IVP) with serial renal tomography starting just before the injection of the contrast media and continuing every 4 minutes for the next 20 minutes.
Most patients with MSK are asymptomatic; unless they have an IVP for an unrelated reason, the condition may never be diagnosed. The overall prevalence in the general population has been estimated at approximately 1 case per 5000-10,000 people, while the prevalence among persons receiving an IVP for any reason is approximately 1 case per 200 patients. No autopsy studies have been conducted to document the exact prevalence of the disease.
Of patients who are symptomatic, renal colic and calcium urinary stones are the most common problems. (UTIs and hematuria are the others.) Women are more likely to have
MSK than men. The number of patients with MSK among all stone formers is not known; it ranges from 2.6-21% in various studies. A nephrolithiasis patient with MSK is estimated to pass 1.23 stones per year, compared with 0.66 stones per year in calcium stone formers without MSK. Hypercalcemia and hypercalciuria are quite common in patients with MSK, occurring in as many as 50% of these patients in some studies. Renal leak hypercalciuria is more common in MSK patients than in other hypercalciuric calcium stone formers.
Hypocitraturia is also more common in MSK stone-forming patients, with a rate roughly double that of calcium stone formers without MSK.
Hypomagnesuria and distal renal tubular acidosis have been found more often in calcium stone–forming patients than in other calcium nephrolithiasis patients. UTIs also seem to be more prevalent in MSK patients, both with and without renal stone formation, compared with other patients (with a higher incidence in women, as expected). Renal failure is rare.
Some patients with MSK may report severe chronic renal pain without any evidence of infection, stones, or obstruction. The etiology of this pain is unclear. These patients may be treated best by physicians comfortable with the management of chronic pain disorders.
MSK is the most common anatomical problem found in calcium nephrolithiasis patients, affecting approximately 2% overall. Most stones in patients who have MSK are composed of calcium oxalate with or without calcium phosphate. Stones tend to be small and are usually passed spontaneously. Renal hemihypertrophy is more common in MSK patients. Up to
10% of all patients with hemihypertrophy of the kidney have
MSK and 25% of all MSK patients demonstrate renal hemihypertrophy.
In most cases, MSK is not hereditary, although rare autosomal inherited forms have been described. The exact cause is unknown, but it could be caused by tubular obstruction due to calcium oxalate calculi from infantile hypercalciuria or collecting duct dilation from blockage by fetal uric acid stones, embryonal remnants, or other material.
Beckwith-Wiedemann syndrome (ie, high birth weight, macroglossia, omphalocele, adrenal cortical cysts, mental retardation, visceromegaly, renal enlargement, hemihypertrophy, and MSK) has a high tumor rate, particularly Wilms tumor, hepatoblastoma, and adrenal cancer. For this reason, when MSK is found in pediatric patients, routine screening for Wilms and other tumors is recommended, particularly when microscopic or gross hematuria is present. Hemihypertrophy also suggests the need for periodic screening for renal tumors or masses.
No specific treatment is available for MSK. Therapy is aimed toward avoiding complications of calcium nephrolithiasis and urinary infection. The author recommends early metabolic evaluations (ie, serum and 24-h urine determinations for preventive analysis) to identify correctable causes such as hypercalciuria and hypocitraturia. Appropriate hygienic advice and sometimes long-term, low-dose antibiotics (eg, nitrofurantoin, trimethoprim-sulfamethoxazole, cinoxacin) may be needed for UTI prophylaxis (see Preventing UTIs in
Women).
CT Scans
CT scans were first used in 1972 but have only become popular in the initial evaluation of acute renal colic since
1995. Part of the reason CT scans became popular was the need for faster scanners, such as the helical or spiral units
that have been in widespread use since 1989. These improved scanners allowed studies to be completed much faster than earlier machines, usually during a single breath, which improves image quality by reducing respiratory motion and artifact.
Many institutions now have a renal colic study or protocol that consists of a noncontrast or unenhanced CT scan of the abdomen and pelvis with a helical or spiral machine. Very narrow cuts are taken through the kidneys and bladder areas, where symptomatic stones are most likely to be encountered. An abdominal flat plate or KUB radiograph is sometimes automatically included in a renal colic study, depending on the institution and the preferences of the medical staff. Technically, a relatively high pitch of more than
1.5 with thin collimation of 2-3 mm is generally considered a good compromise between imaging quality and radiation dosage. No rectal, oral, or intravenous contrast is used because contrast material obscures any calcium-containing stones; both the stone and the contrast material would appear radiopaque or white on the scans. Optimally, the patient's bladder is filled, which facilitates viewing the ureterovesical junction.
In equivocal cases in which an indeterminate calcification is found along the course of the ureter or an abrupt change in ureteral caliber is found without a conclusively identified stone, an overlapping retrospective series can be performed to better evaluate this specific area and eliminate any sampling error.
Phleboliths are often confused with calcific ureteral stones.
On a KUB radiograph, the characteristic lucent center of a phlebolith is often visible, which is not present in a true calculus. Unfortunately, CT scans usually fail to reveal this central lucency or a bifid peak if a central lucency cannot be identified. Why this finding of a central transparency is so uncommon with CT scanning is unclear, but it may involve the orientation of the veins that form the phleboliths.
The "rim sign," originally reported by Smith in 1995, is described as a rim, ring, or halo of soft tissue visible on CT scans that completely surrounds ureteral stones.
5 The effect is enhanced by the local inflammation a stone produces in the ureteral wall, with subsequent edema at the site of the calculus. The rim sign is generally missing or incomplete with phleboliths. While not absolutely definitive, the rim sign is strong evidence that the calcific density it surrounds is a stone and not a phlebolith. In several studies, more than 75% of all ureteral stones demonstrated a rim sign, while only 2-
8% of phleboliths demonstrated it. The rim sign is more likely to be present in small or medium stones up to 5 mm in diameter. Larger stones, bigger 6 mm, tend to lose the rim sign, presumably from stretching and thinning of the ureteral wall around a relatively large calculus.
Another way to differentiate a phlebolith from a calculus is to find a comet's tail or comet sign, which is the noncalcified portion of a pelvic vein that is contiguous with the phlebolith.
It appears as a small linear area of soft tissue that seems to pass obliquely through the CT scan section and attaches to the calcific density at one end. This is not observed in ureteral stones, although a ureter can mimic this sign to some degree. The comet sign is found in less than 20% of phleboliths, so its absence helps little, and its reliability is still unproved.
CT scans are readily available in most hospitals and can be performed and read in just a few minutes. Overall sensitivity from multiple studies is reported at 94-100%, with accuracy rated at 93-98%. CT scans do not require contrast, eliminating the risk of allergic reactions or renal failure.
Stones, including relatively radiolucent uric acid calculi, cystine, matrix, and xanthine, show up as bright white spots, making identification easy. While they do not contain calcium, the stones are still much denser than the surrounding soft tissue. The only exception is stones made of various metabolites of medications, such as indinavir
(Crixivan), which is a protease inhibitor used in the treatment of HIV disease; these stones are not be visible on CT scans.
These patients require a contrast study, such as an IVP.
Spiral CT scans allow for anatomical 3-dimensional image reconstruction, which may be useful in the evaluation and pretreatment planning of large staghorn stones prior to percutaneous nephrostolithotomy. However, not all experts agree on the usefulness of this test for this purpose.
Secondary CT signs of obstruction
1.
Secondary signs of obstruction may be visible only on CT scans. In some cases, if a stone was passed shortly before the study, these signs may be the only evidence that the patient has or ever had a stone. These secondary signs include ureteral dilation with hydronephrosis, renal enlargement from interstitial edema (nephromegaly), and inflammatory changes, such as stranding or streaking in the perinephric fatty tissue.
2.
In a 1996 study of 54 ureteral stone patients reported by
Katz et al, hydronephrosis was present in 69%, proximal ureteral dilation was found in 67%, and perinephric stranding was detected in 65%. The other secondary signs had a similar frequency in adults and children. In the study, only 2 of the patients with ureteral calculi did not demonstrate any of the secondary signs of obstruction. The other secondary signs had a similar frequency in adults and children.
6
3.
A similar 1996 study by Smith et al involving 220 patients found an even higher correlation between these secondary signs of obstruction and the presence of a ureteral calculus. In particular, the combination of collecting system dilation and perinephric stranding had a positive predictive value of 98%, while the absence of both of these secondary signs had a negative predictive value of 91%.
7 However, perinephric stranding was found less often in children with ureteral calculi than in adults in a 2001 study by Smergel and associates; therefore,
this secondary sign, at least in the pediatric population, may be less reliable.
8
4.
An additional secondary sign of acute renal obstruction on noncontrast CT scans has been reported by investigators from Johns Hopkins University. This sign is defined as a reduction in renal parenchymal attenuation
(radiologic density) on the nonenhanced CT scan of the acutely obstructed renal unit compared with the normal unobstructed contralateral kidney. The difference in density is at least 2 standard deviations. This sign was identified in 95% of patients with acute ureteral obstruction, which suggests it is a reliable indicator.
5.
Rarely, in indeterminate cases in which the secondary signs are negative and a stone is strongly suspected clinically but not clearly visible on the unenhanced CT scan, intravenous contrast can be used to help visualize the ureter. Repeat scanning after contrast infusion allows for improved visualization of the ureters. This allows physicians to make direct comparisons with the earlier studies to help make the correct diagnosis. Flat abdominal radiograph films taken after the contrast provide information similar to an IVP, but delayed films or scans are likely to be needed.
Currently, CT scans can be used to estimate the relative stone density and composition to some extent, although the results certainly have not replaced the formal stone chemical composition analysis. However, this information may some day be used to help plan therapy. Higher-density stones may be more amenable to laser lithotripsy and ureteroscopy, while low-density readings are more likely to have good results with ESWL. Uric acid is the lowest-density stone material visible on unenhanced CT scans.
Researchers at the University of Wisconsin at Madison carefully studied the unenhanced CT scans of 129 patients with renal stones. They concluded that the peak Hounsfield attenuation level of a kidney stone, used either by itself or divided by the size of the calculus in millimeters, may be a useful indicator of the stone's chemical composition. An attenuation-to-size ratio of 80 or greater was found to be highly suggestive of calcium oxalate stone material, especially in larger calculi. Uric acid stones have relatively low peak attenuation levels, and their attenuation-to-size ratios were generally below 80. In this Wisconsin study, uric acid stones averaged a mean peak Hounsfield reading of 344 HU, while the mean for calcium oxalate calculi was 652 HU. Overall sensitivity was 94% and specificity was 84%, with a negative predictive value of 99%.
This information, combined with the KUB radiographic appearance and low urinary pH values, can be helpful in identifying uric acid calculi, which are amenable to alkalinization therapy. Calculating the peak attenuation level and attenuation-to-size ratio adds no financial cost, patient morbidity, or time delay. While this study and similar reports are interesting and suggestive, the precise clinical role of CT scans in predicting stone fragility and chemical composition remains unclear.
If the patient's true underlying pathology is something other than a kidney stone, the CT scan is more clinically useful than an IVP for examining other possible problems such as aneurysms, pancreatitis, appendicitis, ovarian problems, and various bowel disorders.
Disadvantages of a CT scan include increased cost and difficulties in identifying a stone if the patient exhibits limited hydronephrosis and multiple pelvic calcifications. A CT scan cannot provide precise information about relative renal function and usually cannot be used to diagnose MSK. CT scans can be used to estimate the overall size, width, and location of a stone, but they can only approximate the stone's shape. For example, the CT scan does not necessarily reveal the stone precisely at its widest point, which would provide an accurate measurement of the stone's maximum width. CT scan measurements of stone widths have a reported error rate as high as 12%. Further, a 2002 review by
Narepalem et al found that CT scans are even less accurate and reliable in measuring ureteral stone length compared with a simple KUB radiograph.
9 Stone location can be described in anatomical terms, but the scan lacks the surgical orientation that most urologists prefer.
Curved planar reformatting using CT software can be performed to convert the cross-sectional images of the CT scan into an image that approximates a traditional abdominal radiograph study. Because of the relatively high dose of ionizing radiation it uses, CT scans should not be performed on pregnant women.
Finally, the CT scan alone does not allow visual differentiation between a radiolucent and a radiopaque calculus. If a KUB or flat plate radiograph is performed at the same time as the CT scan, many of these objections and problems disappear.
However, obtaining the extra films involves some additional delay, the patient is exposed to more ionizing radiation, and the total cost for the workup increases.
A digital CT scout radiograph has been suggested as a possible reasonable substitute for a formal KUB radiograph in some cases. Stones 3 mm and larger can be observed routinely on these studies. If the findings from a noncontrast
CT scan are positive for a stone and the findings from the scout CT radiograph are negative, a separate KUB radiograph should be performed.
A computer program is available on the Internet
(through UroComp) that is able to calculate the KUB stone appearance size from CT scan data. In cases in which a KUB radiograph is not available or KUB radiograph stone visualization is inadequate (as in uric acid calculi), this online program converts CT-derived stone size data into expected dimensions based on the KUB radiographic appearance. The clinical usefulness of such a tool is unclear; however, this new online stone size calculator could be the first of a series of
online computer programs with true clinical utility in the future.
Certain medications (eg, protease inhibitors) can form urinary stones composed of drug metabolites that are invisible on CT scans. For this reason, if a patient is taking a protease inhibitor drug such as indinavir (Crixivan) and presents with a history suggestive of renal colic, the study of choice is an IVP.
In current clinical practice, the renal colic noncontrast CT scan with a modern helical or spiral machine is the standard of care in most EDs when a patient is thought to have renal colic or a patient presents with acute flank pain. Because of the limitations of CT scans, many urologists routinely request additional studies, such as KUB radiographs or IVPs, to help them make critical decisions about management, follow-up, and possible surgical interventions.
As noted earlier, the author recommends adding a KUB radiograph when a renal colic CT scan study is performed for acute flank pain, especially when the CT scan findings are positive for urolithiasis. The KUB radiograph not only provides more precise information about the size and shape of any stone, it also quickly reveals whether stones are nonopaque and radiolucent (eg, uric acid calculi), which indicates stones that are dissolvable with alkalinizing medication, or opaque and calcific, which indicates stones that are not dissolvable with medication alone.
Follow-up evaluations are easier because only a repeat KUB radiograph is needed for comparison. A KUB radiograph also helps the urologist determine if a stone will be visible on fluoroscopy images, which is essential for possible ESWL. This fluoroscopic visualization is needed for stone targeting and positioning. While the addition of an abdominal flat plate study (KUB radiograph) adds to the overall financial cost and requires additional time, the extra information the study provides is often quite valuable and ultimately beneficial to the patient.
Retrograde Pyelograms
The most precise imaging method for determining the anatomy of the ureter and renal pelvis and for making a definitive diagnosis of any ureteral calculus is neither the IVP nor the renal colic CT scan. It is the retrograde pyelogram. In this study, the patient is taken to the operating room cystoscopy suite and an endoscopic examination is performed with the patient under anesthesia. After a cystoscope is placed in the bladder, a thin ureteral catheter can be inserted into the ureteral orifice on the affected side.
A radiographic picture is taken at the appropriate time, while contrast material is injected through the ureteral catheter directly into the ureter. Any stone, even if radiolucent, and any ureteral kinks, strictures, or tortuousities that may not be visualized easily on other studies become clearly visible.
Urologists perform retrograde pyelograms when a precise diagnosis cannot be made by other means or when a need clearly exists for an endoscopic surgical procedure and the exact anatomical characteristics of the ureter must be clarified. They are also useful for estimating ureteral length prior to placement of an indwelling double-J stent.
Retrograde pyelograms are rarely performed merely for diagnostic purposes because other less invasive studies are usually sufficient. They are considered essential when surgery is deemed necessary because of uncontrollable pain, severe urinary infection or urosepsis with a blocked kidney, a solitary obstructed kidney, a stone that is considered unlikely to pass spontaneously because of its large size (generally >7 mm), or the presence of possible anatomical abnormalities
(eg, ureteral strictures).
Retrograde pyelograms can be performed safely both in patients highly allergic to intravenous contrast media and in patients with renal failure because the contrast medium never enters the bloodstream and therefore requires no renal filtration or excretion and causes no anaphylaxis.
Magnetic Resonance Imaging
MRI has virtually no role in the current evaluation of acute renal colic in the typical patient. Direct detection of most stones is not possible with MRI, and MRI should not be used for that purpose in most instances. MRIs are generally more expensive than other studies, such as CT scans, which reveal stones much better. However, MRI produces no dangerous radiation, the gadolinium contrast it uses has minimal nephrotoxicity, and the technology can readily show urinary obstruction even if the stones themselves are not easily visualized. These attributes make using MRI reasonable in selected cases in which other technologies are too toxic or potentially dangerous, such as in some children, in renal transplant recipients, in pregnant women, and in azotemic patients. MRI may also be appropriate in the evaluation of hydronephrosis when stones have been excluded based on
CT scans and other means are too toxic or inadequate.
Gadolinium-enhanced 3-dimensional fast low-angle shot
(known as 3D FLASH) magnetic resonance urographic imaging was found to be superior to the T2-weighted MRI technique, while combining the two produced the best overall results.
Use of MRI in pregnant patients is controversial. Long-term effects on the fetus are unknown, and MRI is not specifically indicated in pregnancy, although it is not specifically contraindicated either. Anecdotal reports suggest that MRI has no immediately detectable deleterious effects. When other imaging modalities cannot be used or are insufficient, magnetic resonance urographic imaging can be considered on a case-by-case basis when the benefits to the mother and fetus outweigh the potential risks.
IVP Versus CT Scan: Which Is Better?
Imaging
Study
CT scan
Details
Pro Fast
No intravenous contrast necessary so no risk of nephrotoxicity or acute allergic reactions
With only rare exceptions, shows all stones clearly
May demonstrate other pathology
Can be performed in patients with significant azotemia and severe contrast allergies who cannot tolerate intravenous contrast studies
Clearly shows uric acid stones
Shows perinephric stranding or streaking not visible on IVP and can be used as an indirect or secondary sign of ureteral obstruction
No radiologist needs to be physically present
Preferred imaging modality for acute renal colic in most EDs
Con
Without hydronephrosis, cannot reliably distinguish between distal ureteral stones and pelvic calcifications or phleboliths
Cannot assess renal function
Difficult or impossible to identify MSK
No nephrogram effect study to help identify obstruction
Size and shape of stone only estimated
Lacks surgical orientation*
Unable to identify ureteral kinks, strictures, or tortuousities
May be hard to differentiate an extrarenal pelvis from true hydronephrosis
Gonadal vein sometimes can be confused with the ureter
Does not indicate likelihood of fluoroscopic visualization of the stone, which is essential information in planning possible surgical interventions
Needs a KUB radiograph to be a complete study according to many experts †
Cannot be performed during pregnancy because of high dose of ionizing radiation exposure
Usually more costly than an IVP in most institutions
Higher radiation dose than IVP
IVP Pro
Clear outline of complete urinary system without any gaps
Clearly shows all stones either directly or indirectly as an obstruction
Nephrogram effect film indicates obstruction and ureteral blockage in most cases, even if the stone itself might not be visible
Shows relative kidney function
Able to diagnose MSK
Ureteral kinks, strictures, and tortuousities often visible
Can modify study with extra views (eg, posterior oblique positions, prone views) to better visualize questionable areas
Stone size, shape, surgical orientation, and relative position more clearly defined
Orientation similar to urologists' surgical approach
Limited IVP study can be considered in selected cases during pregnancy, although plain ultrasound is preferred initially
Lower cost than CT scan in most institutions
Includes KUB film automatically
Con
Relatively slow; may need multiple delay films, which can take hours
Cannot be used in azotemia, pregnancy, or known significant allergy to intravenous contrast agents
Risk of potentially dangerous reactions to intravenous contrast material ‡
Cannot detect perinephric stranding or streaking, which is visible only on CT scans
Harder to visualize radiolucent stones (eg, uric acid), although indirect signs of obstruction are apparent
Presence of a radiologist generally necessary, which can cause extra delay
Cannot be used to reliably evaluate other potential pathologies
*Many urologists find CT scans inadequate to help plan surgery, predict stone passage, or monitor patients.
† This causes a delay, which may be significant in some institutions, and adds additional patient radiograph exposure and cost.
‡ These include significant allergic responses and renal failure.
Summary of IVP versus CT scan
The noncontrast or renal colic-type CT scan is good for the initial diagnosis of a stone, especially in unusual or atypical cases or when patients are unable to tolerate intravenous contrast because of allergy or azotemia. To be most effective and helpful, a CT scan must be coupled with a KUB radiograph. Without definite hydronephrosis, a CT scan may not be able to isolate a specific stone, although secondary signs, such as perinephric streaking and nephromegaly, may be present. The CT scan can be performed quickly in most institutions, even with an additional KUB radiograph, but it usually costs more than the IVP. In one series of 397 consecutive emergency urolithiasis patients from several university centers, the average fee for a CT scan was $1407, compared with $445 for an IVP.
CT scans are generally preferred by most ED physicians for the initial evaluation of patients with acute flank pain, except for HIV-positive patients who may be on protease inhibitors, who require an IVP, and pregnant women, who require ultrasound for their initial imaging modality.
The IVP is better for clearly outlining the entire urinary tract and determining relative renal function. This test clearly shows stones causing blockage, whether the stones are radiolucent or opaque. While an IVP can reliably help in the diagnosis of an MSK, the clinical importance of this diagnosis is limited. The IVP is sometimes preferred by urologists in certain situations because of its better orientation and superior value in predicting possible stone passage, although these advantages are mostly negated if a KUB radiograph routinely accompanies the CT scan.
Differential Diagnoses of Flank Pain
Most Common and Significant Causes of Flank Pain
Abdominal aortic aneurysms
Patients with abdominal aortic aneurysms may present with symptoms of flank pain that mimic renal colic. This occurs in approximately 10% of patients with abdominal aortic aneurysm who are initially thought to have a renal cause for their pain. The aneurysm is thought to be caused by injury or stretching of the nerve plexus around the celiac axis and other aortic arterial branches that also supply the nerve innervation for the kidneys. The aneurysm can lie immediately adjacent to the ureter and cause hematuria from local ureteral irritation or trauma. Lateral deviation of the ureters, especially on the left side, is a common finding.
Abdominal aortic aneurysms are best diagnosed with ultrasound or a CT scan. This is one of the reasons why CT scanning is especially useful in cases of suspected renal colic in patients older than 50 years, who are at increased risk for an abdominal aortic aneurysm.
Pyelonephritis
Pyelonephritis is a common cause of flank pain, but its discomfort is usually described as a relatively mild dull ache rather than typical renal colic pain. Fever, chills, nausea, and vomiting are the most common symptoms, along with headache and a stiff neck. Flank and costovertebral angle tenderness are present and often are more severe than with renal colic. Patients with pyelonephritis often tend to lie very still in comparison to patients with renal colic, who move constantly in search of a comfortable position. Suprapubic pain with dysuria, frequency, and urgency often accompany the flank pain in persons with pyelonephritis, but distal ureteral calculi can produce similar symptoms. Fever, leukocytosis, and pyuria are typical findings in persons with pyelonephritis.
Extensive imaging studies may not be required in cases of obvious pyelonephritis, but, in some cases, a renal ultrasound may be helpful to identify hydronephrosis because pyelonephritis does not demonstrate any renal pelvic or ureteral dilation. Any collecting system dilation found suggests a possible obstruction with pyonephrosis. Perform appropriate studies immediately, and promptly institute surgical intervention for drainage. Uncomplicated pyelonephritis without obstruction can be treated with antibiotics alone.
Renal abscesses
Renal abscesses tend to cause more intense pain than pyelonephritis, possibly because the increased edema and inflammation produced further stretch the renal capsule.
Sometimes, a flank mass may be palpable. Urinalysis often demonstrates a urinary infection, but, in some cases, the urinalysis findings may be normal. Fever and chills are common. Diaphragmatic irritation may be present, causing rales and decreased breath sounds on the affected side.
People with diabetes are at increased risk.
Consider a possible renal abscess in any patient with pyelonephritis who does not improve with antibiotic therapy.
Renal ultrasound and CT scans are the most useful imaging studies for making this diagnosis.
Renal abscesses can be divided generally into 2 types. The corticomedullary renal abscess is usually derived from an ascending urinary infection and is often associated with some type of urinary tract abnormality such as vesicoureteral reflux or obstructive uropathy. Escherichia coli is the most common organism involved, found in 75% of these lesions. The second type, the cortical renal abscess, develops from the hematogenous spread of bacteria, usually Staphylococcus
aureus, from a primary focus point elsewhere in the body.
Drainage of the abscess, either by open surgery or percutaneous methods, is the recommended treatment, along with culture-specific antibiotics whenever possible.
Blood clots
Blood clots sometimes cause an acute renal colic attack when they form a sudden ureteral obstruction. These blood clots can be from iatrogenic causes, such as percutaneous renal biopsies, or from underlying medical problems, such as blood dyscrasias, renal pelvis or parenchymal tumors, angiomyolipomas, hemophilia, sickle cell disease, or glomerulonephritis. Treatment with a ureteral stent or percutaneous nephrostomy is usually sufficient therapy for the immediate blockage. Direct infusion of a clot-dissolving medication such as streptokinase has been successful in selected cases.
Herpes zoster
Herpes zoster causes a moderately severe burning pain, usually in a band around the flank corresponding to a dermatome. The pain usually appears before characteristic skin changes appear. Eventually, the vesicles appear over the affected area, and the diagnosis can then be made easily.
Although the pain distribution may be similar, the clinical presentation and location of the discomfort allow differentiation from renal colic. Suspect herpes zoster when the pain is described as burning and constant with a very limited and clearly demarcated distribution, even if no skin
lesions are present. Treatment is symptomatic in nature, with analgesics and antiviral agents.
Muscle pain
Muscle pain from a strain or other injury of the back or flank can lead to a dull aching discomfort in the thoracolumbar area. The quadratus lumborum muscle may be involved. The discomfort is exacerbated by lifting and bending. The patient may reveal a history of heavy lifting or repetitive bending at work. The affected area is likely to be tender to palpation.
Injection of a local anesthetic into the trigger points may afford significant relief and may help in the diagnosis. Treat such pains with analgesics, NSAIDs, and heat applications.
Papillary necrosis
Papillary necrosis can cause an acute ureteral obstruction from the sloughed papilla. Underlying pathologies include analgesic abuse, liver cirrhosis, and diabetes. A ring sign caused by the outline of a round or triangular filling defect surrounded by contrast in a renal calyx upon IVP characterizes this disorder. The actual sloughing of the renal papilla is caused by vascular ischemia, which leads to coagulative necrosis of the renal medullary pyramids.
Women are affected more often than men. Underlying pathologies include analgesic abuse, liver cirrhosis, recurrent pyelonephritis, urinary tract obstruction, tuberculosis, sickle cell disease, systemic vasculitis, renal transplant rejection, and diabetes. Treatment of the underlying pathology and bypassing the obstruction with a nephrostomy or stent is the recommended therapy.
Pleuritis and pneumonia
Pleuritis can cause a sharp stabbing pain in the thoracolumbar region, which, in some cases, can simulate renal colic. The etiology of the pleuritis may be infectious causes (eg, tuberculosis, pneumonia) or noninfectious causes
(eg, lupus, pulmonary emboli). The presence of respiratory symptoms or atypical pain involving the chest suggests these possible differential diagnoses and the need for chest radiography, which may help clarify the issue. Treatment is based on the underlying etiology.
Radiculitis
Radiculitis occurs when the lumbar or lower thoracic nerve roots are injured. An injury to the costovertebral junctions can also produce a radiculitis-type pain. When the pain affects the 10th, 11th, or 12th ribs, the discomfort mimics renal colic in its distribution but is usually described as sharp or stabbing. The pain is often acute and can radiate anteriorly and inferiorly, identical to renal colic pain. Movement exacerbates the pain. The fracture of a transverse process in the thoracic or lumbar regions can also produce this pain.
Most patients are female. Predisposing factors include a history of rib fractures, arthritis, and a prior open renal surgery. The actual source of the pain is usually scarring or injury of the intercostal nerve. Radiculitis is a common cause of flank pain that is not of renal origin and should be suspected in patients with normal urinalysis findings and normal imaging findings from studies of the urinary system.
Rib pain
Rib pain from a fractured or injured 11th or 12th rib can cause flank pain with anterior and inferior radiation similar to the pain distribution of renal colic. While this is usually from trauma, sometimes prolonged violent coughing can cause injury. Displacement of the fractured rib is rare. The rib usually produces intense pain when palpated directly. Deep respiration is also painful. Renal injury from the fracture is uncommon but possible. Radiographic findings establish the diagnosis. Costochondritis or inflammation of the rib without a fracture can also duplicate the pain distribution of renal colic but does not demonstrate a fracture on radiographs.
The diagnosis is usually made on clinical grounds and by excluding other etiologies.
Fungal bezoars
Fungal bezoars are most commonly composed of Candida or Aspergillus species and are found primarily in patients who are immunocompromised, such as renal transplant recipients or neonates. Predisposing factors include transplantation, cancer, long-term antibiotic use, and diabetes. Besides the usual drainage or bypass procedures, urinary alkalinization and antifungal medications are also recommended therapies.
Kidney tumors
Kidney tumors may cause flank pain either directly, from renal capsular stretching, or indirectly. Tumor thrombi that have broken off from their primary base because of necrosis can cause an acute ureteral obstruction. Primary tumor extension can also cause an obstruction, although this is usually a slow and insidious process during which patients are often asymptomatic. Renal tumors, such as renal cell cancers, oncocytomas, and angiomyolipomas, can cause renal capsular stretching and pain as well as hematuria, with possible ureteral obstruction from subsequent blood clots.
Angiomyolipomas are especially prone to bleeding and ureteral blood clot formation.
UPJ obstruction
UPJ obstruction is one of the more common causes of renal pain. This condition is often detected as an incidental finding during imaging for unrelated problems. The pain is similar to an acute ureteral obstruction and usually follows the ingestion of large amounts of fluid, which causes a brisk diuresis resulting in renal pelvic distension and colic. The diagnosis is confirmed by a diuretic-enhanced renal nuclear medicine scan, although an IVP with an accelerated diuresis from intravenous furosemide (Lasix, usually a 20-mg dose) frequently demonstrates the obstructed renal pelvis.
Palliation sometimes requires temporary drainage with a stent, ureteral catheter, or nephrostomy tube. This temporary drainage can also help confirm the diagnosis by eliminating the pain if the cause is truly UPJ obstruction.
Permanent curative therapy requires surgical repair of the
obstruction by various endourological means, either percutaneously (antegrade) or cystoscopically (retrograde).
Open pyeloplasty surgery and laparoscopic surgical repairs can also be performed. A nephrectomy is sometimes performed in selected cases.
Retroperitoneal fibrosis
Retroperitoneal fibrosis is an idiopathic disease in which fibrous tissue overgrows the retroperitoneal organs, starting at the midline. When this process involves the ureters, it causes ureteral midline deviation, hydronephrosis, and even renal failure. Retroperitoneal fibrosis has been associated with the use of methysergide (used for migraine headaches) and some malignancies, but the cause of most of these cases is unknown. Males are affected twice as often as females, and patients are usually aged 40-60 years.
The pain of retroperitoneal fibrosis is usually located first in the lower flank and abdominal regions. Testicular and periumbilical pain develops later. The pain is usually described as dull with an insidious onset that progressively becomes more severe. Ureterolysis, in which the ureters are surgically removed from the fibrous tissue, can relieve the pain, which suggests that pain is ultimately from a ureteral source even if it is not typical ureteral colic. The pain possibly stems from involvement of the peripheral ureteral nerves or from nerve centers in the outer wall of the ureter or even outside the ureter rather than the intramural submucosal free nerve endings that typically cause renal colic.
Ureteral strictures
Ureteral strictures usually result from trauma, surgical intervention, radiation, stone passage, infection, or other injury to the ureters. They are found most commonly at the
UPJ, at the ureterovesical junction, and overlying the bifurcation of the iliac vessels where the middle and distal thirds of the ureter join. Treatment is by surgical intervention.
Acute renal infarction
While acute renal infarction is assumed to be a rare disorder, the fact that it is almost always misdiagnosed at initial presentation makes accurately predicting the actual incidence difficult. It is now believed to be a relatively common clinical entity that is frequently misdiagnosed initially as acute renal colic, pyelonephritis, or acute abdomen. Acute renal infarction affects both kidneys and both sexes equally. The average age of affected patients is approximately 65 years. High-risk factors for acute renal infarction include age older than 50 years and an increased risk for thromboembolism such as patients with a prior history of a thromboembolic event and chronic atrial fibrillation with inadequate anticoagulant therapy.
The most common presenting symptoms are unilateral flank pain and hematuria, which affect virtually every patient with this disorder. Other common symptoms include fever, nausea, and vomiting. Serum lactate dehydrogenase levels and WBC counts are usually elevated. Definitive diagnosis is usually made using a CT scan. Treatment is with intravenous heparin, intra-arterial clot-busting infusions, or both.
Other causes
Other causes of flank pain include retrocaval ureter, Crohn disease, diverticulitis, appendicitis, acute myocardial infarction, ureteral obstruction from bullet fragments and shotgun pellets, various retroperitoneal disorders (eg, lymphoceles, lymphoma), renal vein thrombosis, "nutcracker syndrome" (in which the left renal vein is compressed between the superior mesenteric artery and the aorta), left renal vein–aorta fistula, oral contraceptive–induced loin pain syndrome, glomerulonephritis, Berger disease, acute nephritis, polycystic kidney disease, pyelocalyceal diverticulum, iliac osteomyelitis, ulcer disease, cholecystitis, adrenal tumors and hemorrhage, colon cancer, and splenic infarction.
Gynecological Causes of Flank Pain
Ectopic or tubal pregnancy
Ectopic or tubal pregnancy usually causes unilateral pain in the lower abdomen. The pain may be either colicky or constant. A personal history of menstrual problems or irregularities, especially with increased beta-human chorionic gonadotropin levels in the blood or urine, is highly suggestive. Pelvic ultrasound is diagnostic. Surgical intervention is required.
Endometriosis
Endometriosis may occasionally involve the ureters, especially the distal portions, where it can cause ureteral colic and flank pain. Endometriosis usually causes extrinsic compression from scarring but also may directly involve the ureteral wall, although this is less common. Imaging studies are often not helpful for identifying endometriosis because it commonly appears as a stricture or tumor. Hormonal treatment is not always successful when the ureters are involved, and surgical resection of the affected ureteral segment is needed to provide relief.
Ovarian cyst rupture or torsion
Ovarian cyst rupture or torsion may cause unilateral lower abdominal quadrant pain, which tends to increase over time.
A pelvic examination may suggest this diagnosis, but confirmation usually requires pelvic ultrasound.
Ovarian vein syndrome
Ovarian vein syndrome occurs when the overlying ovarian veins become dilated and compress the ureters, causing an extrinsic obstruction. This condition is often associated with pregnancy. Surgical ligation of the offending ovarian veins cures the problem. This syndrome has been suggested to be fictitious, with the observed ureteral dilation noted in these patients probably resulting from postpregnancy-related changes without any true anatomical or functional obstruction.
Pelvic inflammatory disease
Pelvic inflammatory disease generally causes bilateral lower quadrant pain, but patients may sometimes present with
unilateral symptoms. Patients usually have fever and leukocytosis, but as many as 35% of patients with acute salpingitis may be afebrile. A pelvic and bimanual examination of the adnexal organs, which is necessary in any female patient presenting with abdominal or pelvic pain, usually suggests the diagnosis, which can be confirmed by pelvic ultrasound. Adnexal and cervical tenderness coupled with a history of sexually transmitted diseases suggest this diagnosis.
Pregnancy
Pregnancy is usually associated with a physiologic hydronephrosis, which cannot be distinguished easily from dilation due to a stone. Diagnostic and therapeutic options are limited. Renal ultrasound may be helpful, but the findings are often inconclusive. A plain radiograph is often the next step. In early pregnancy, the routine use of radiographs cannot be justified unless the clinical situation is urgent.
While the risk of any radiation exposure is a concern, a limited IVP can be performed with relative safety. The number of films must be limited and the clinical situation sufficiently serious to justify the radiation exposure risk.
Treat possible pyelonephritis with antibiotics; ampicillin is usually preferred until culture results are available.
Cephalosporins are used in penicillin-allergic patients.
Preventing UTIs in Women
1.
Wipe front to back. Always wipe from the front to the back after using the bathroom. Do not try to reach from behind because germs from the rectum can be transferred to the hand and tissue. After bowel movements, clean the area around the anus gently, wiping from front to back. Never wipe twice with the same tissue. Wipe the same way for washing and showering. Do not rub. Soft, white, unscented tissues or
"baby wipes" are recommended. A disposable antiseptic towelette may also be used. Most urinary infections are from bacteria that normally live around the rectum. Any wiping motion that starts nearer to the rectum and then approaches the bladder opening area moves dangerous bacteria closer to the bladder.
2.
Wash hands before wiping. Wash hands before using the toilet or at least before wiping. Hands should be washed before showering to avoid passing germs from the hands to the bladder area.
3.
Take showers and avoid baths. Showers are much preferred to baths. If a bath is absolutely necessary, do not use any bubble bath or other cosmetic bath additives. Bath water is full of bacteria from the skin.
Sitting in a tub allows bacteria to reach the bladder opening area.
4.
Wash properly in the shower. Wash hands before getting into the shower. Use a fresh, clean washcloth. Use a liquid soap because bar soap can harbor bacteria. Do not use soap for the bladder opening area that has perfumes, creams, or other additives. (The author usually recommends Dial or Ivory.) Clean the bladder opening area first, before the washcloth comes into contact with any new germs or bacteria. The washcloth or hand that washes the rest of the body picks up dirt, germs, and bacteria from the skin. These germs should not be moved closer to the bladder. Wipe only once with each washcloth. If more extensive cleaning is necessary, use a second washcloth. Try not to over-clean this area because washing with soap removes some of the natural protection (ie, mucus) from the bladder opening area.
Rinse well and remember to wipe correctly from front to back. The washcloth that cleans the bladder opening area should be used only for that purpose and then laundered.
5.
Douches may be okay, but avoid other personal products. In most cases, a vinegar and water douche with povidone-iodine solution (Betadine) or benzalkonium chloride is helpful if performed correctly at appropriate intervals. Do not use any feminine hygiene sprays, cosmetics, perfumes, towelettes, or similar products in the vaginal area unless approved by a physician.
6.
Use tampons for periods. Tampons are advised during the menstrual period rather than sanitary napkins or pads. A tampon keeps the bladder opening area drier than a sanitary pad and helps keep bacterial growth and contamination away.
7.
Avoid long intervals between urinating. Try to empty the bladder at least every 4 hours during the day while awake, even if the need or urge to void is absent. When feeling the need to empty the bladder, do not try to
"hold it" until a more convenient time or place.
8.
Do not wear tight clothes. Avoid wearing pantyhose or tight slacks for prolonged periods. Cotton underwear for general use is suggested. Avoid wearing a wet bathing suit for prolonged periods. Try to avoid habitual leg crossing. All of these actions tend to press the skin folds around the vagina into the body and may introduce more bacteria into the area around the bladder opening.
9.
Drink more water. Start with one extra glass with each meal. If the urine appears any darker than a very pale yellow, this means not enough liquid is being ingested; increase the fluid intake. Cranberry juice is helpful, but other beverages can be substituted.
10.
Avoid irritating foods such as caffeine. Symptoms of bladder irritation may be aggravated by coffee, tea, alcohol, hot spices, caffeine, artificial sweeteners containing aspartame (ie, NutraSweet), chocolate, and cola drinks.
11.
Take vitamin C and drink cranberry juice. Some patients may be instructed to take some additional vitamin C.
This vitamin may help increase the body's resistance to infection. Extra vitamin C that the body cannot use immediately is released into the urine, where it helps
block bacterial growth. Cranberry juice may be of some extra benefit in reducing urinary infections. The same benefit can be obtained from cranberry pills.
12.
Avoid activities that increase the risk of bladder infections. Prolonged bicycling, motorcycling, horseback riding, and similar physical activities and exercises may increase the risk of bladder infections. Limiting these types of activities may be necessary. When engaging in physical activity and exercise, make sure to empty the bladder frequently and drink plenty of water and other fluids. Sexual activity may also increase risk because it can introduce bacteria into the bladder area (see below).
13.
Take special precautions after sexual activity. The bladder should be emptied after intercourse; drink 2 extra glasses of water. Some patients are advised by their physician to take a urinary antiseptic or antibiotic after sexual activity. Make sure to take the medication according to the physician's recommendation.
14.
An estrogen vaginal cream may help increase resistance to bladder infections. An estrogen cream for the vagina may be suggested for women after menopause even if an oral estrogen supplement or patch has already been prescribed. The cream helps keep the tissues around the bladder healthy and more resistant to infection.
15.
Take antibiotics only as prescribed by a doctor. If a medication has been prescribed as preventive therapy, follow the physician's instructions carefully. Be aware that medications may be necessary for up to a year or more depending on the nature and severity of the urinary infection problem. For some patients, a small amount of urinary antibiotic or antiseptic taken daily prevents most urinary infections and allows the bladder to heal and restore its natural resistance. Other patients may be told to take an antibiotic only when they think they are getting an infection. Take any prescribed medication exactly according to the physician's advice.
Contact the physician or pharmacist if no clear instructions are on the bottle of medicine.
16.
The guidelines and suggestions listed here help most women avoid bladder infections most of the time. If an infection develops in spite of these precautions, promptly seek medical help. A urine specimen for examination should be provided. Seek prompt attention for excessive vaginal discharge or other signs of vaginal inflammation and infection. If an antibiotic has been prescribed for this purpose, begin taking it. In some cases, the physician may request additional tests such as kidney radiographs or an examination of the bladder.
Sterilizing washcloths may be the next reasonable step to take.
Sterilizing washcloths for home use
Sterilizing washcloths for washing and personal hygiene to help prevent recurrent UTIs may be recommended. This extra step is probably unnecessary for most patients with recurrent infections, but for the more resistant or severe cases, it may be very helpful. Home sterilization of washcloths is only one part of an ongoing program to help prevent these infections. Use only those washcloths purchased for this purpose and remember to wipe correctly, front to back.
1.
Wash the washcloths with hot water and soap in a clothes washer. If a clothes washer is unavailable, use soap and hot water in the sink.
2.
Boil the washcloths in water for at least 20 minutes
(optional).
3.
Take the washcloths out of the water and allow to dry or use a clothes dryer.
4.
When dry, place each washcloth in a separate sealable plastic bag, such as a zip-lock bag. Leave the bags open; do not seal them yet.
5.
Place the bags containing washcloths in a microwave oven. Put a large glass of cold water in the center of the microwave oven. Do not place the bags with the washcloths in the water.
6.
Put the microwave oven on high power, set the timer for
5 minutes, and turn it on. Replace the glass (which is very hot) with a new glass of cold water, and run the microwave oven on high power for an additional 5 minutes.
7.
Let the bags cool, then close the bags. The sterile washcloth is now inside a sterile bag.
This technique kills the germs and bacteria by using microwave radiation to sterilize the washcloths. Without the glass of cold water to absorb the heat, the bags would melt and the washcloths would burn.
Summary of tips for preventing urinary infections
1.
Wipe in the correct direction, from front to back, after using the bathroom.
2.
Wash hands before using washcloths, tissues, or toilet paper for wiping or washing.
3.
Use a liquid soap because it is usually cleaner than bar soap.
4.
Only wipe once with each washcloth or tissue. Use a second washcloth for additional washing.
5.
Clean the bladder area first when washing to prevent contamination with bacteria from other parts of you the body.
6.
Do not use these washcloths for any other purpose except to clean the area around the bladder opening.
7.
Drink extra water. Take vitamin C (but not >1000 mg).
Drink cranberry juice (or take cranberry pills). Use an estrogen cream if postmenopausal. Take any medication as prescribed by a physician.
Medical and Surgical Treatment
Most small stones with relatively mild hydronephrosis can be treated with observation and acetaminophen. More serious cases with intractable pain may require drainage with a stent or percutaneous nephrostomy. The double-J stent is usually
preferred in these situations because of decreased morbidity.
Acetaminophen can be used in pregnancy for mild-tomoderate pain. Opioid drugs, such as morphine and meperidine (Demerol), are pregnancy category C medications, which means they can be used but they cross the placental barrier. Opioids can cause respiratory depression in the fetus; therefore, opioid medications should not be used near delivery or when other medications are adequate.
Medical Treatment
Initial treatment of a renal colic patient in the ED starts with obtaining intravenous access to allow fluid, analgesic, and antiemetic medications to be administered. Many of these patients are dehydrated from nausea and vomiting.
Using hydration and diuretics as a therapy to assist stone passage remains controversial. Some experts believe hydration may increase the speed of passage of a stone through the urinary tract, while others worry that the extra liquid only increases the hydrostatic fluid pressure inside the blocked renal unit, exacerbating the pain. The ED at the author's affiliated hospital prefers to administer extra hydrating fluid, especially when the stone is 4 mm or smaller, but no firm data support either theory. Clearly, extra fluid should be administered to patients with laboratory or clinical evidence of dehydration, diabetes, or renal failure.
Straining the urine
Collecting any passed kidney stones is extremely important in the evaluation of a patient with nephrolithiasis for stonepreventive therapy. Yet, in a busy ED, the simple instruction to strain all the urine for stones can be easily overlooked.
Knowing when a stone is going to pass is impossible regardless of its size or location. Even after a stone has passed, residual swelling and spasms can cause continuing discomfort for some time. Be certain that all urine is actually strained for any possible stones. An aquarium net makes an excellent urinary stone strainer for home use because of its tight nylon weave, convenient handle, and collapsible nature, making it very portable; it easily fits into a pocket or purse.
Hospitalization
The decision to hospitalize a patient with a stone is usually made based on clinical grounds rather than on any specific finding on a radiograph. Hospital admission is clearly necessary when any of the following is present:
1.
Oral analgesics are insufficient to manage the pain.
2.
Ureteral obstruction from a stone occurs in a solitary or transplanted kidney.
3.
Ureteral obstruction from a stone occurs in the presence of a UTI, fever, sepsis, or pyonephrosis.
Relative indications to consider for a possible admission include comorbid conditions (eg, diabetes), dehydration requiring prolonged intravenous fluid therapy, renal failure, or any immunocompromised state. Larger stones (ie, >7 mm) that are unlikely to pass spontaneously require some type of surgical procedure. In some cases, hospitalizing a patient with a large stone to facilitate surgical stone intervention is reasonable. However, most patients with acute renal colic can be treated on an ambulatory basis.
Generally, hospitalization for an acute renal colic attack is now officially termed an observation because most patients recover sufficiently to go home within 24 hours.
Consultations
The presence of urosepsis in a patient with an obstruction from stone disease (ie, pyonephrosis) is a true surgical emergency. Consult a urologist immediately. This condition requires hospital admission; intravenous fluids; antibiotics; and, most importantly, early drainage of the affected kidney using double-J stents, stone removal, or percutaneous nephrostomy. Depending on the individual circumstances, generally the least invasive option is selected, which is usually the double-J stent or a percutaneous nephrostomy.
Later, when the infection is under control and the patient is no longer septic, a more definitive procedure can be performed to remove or fragment the obstructing stone.
Other conditions for which a urologist should be consulted include with the presence of unusually large stones, high-risk medical conditions, uncontrollable pain, renal failure, solitary kidneys, renal transplants, pregnancy, and prior history of stones that required surgical intervention.
Patients who are pregnant require a consultation with an obstetrician-gynecologist, and those with a history of severe cardiac disease or congestive heart failure may benefit from involvement of an internal medicine specialist or cardiologist.
Patients with strong motivation to prevent all future stones, those with multiple recurrences or single functioning kidneys, and all children younger than 16 years with nephrolithiasis should be referred to a specialist in nephrolithiasis prevention. A medical expert in metabolic stone prevention testing, interpretation, and prophylactic therapy is available in most communities.
Medications
Narcotics and opioids
The mainstay of medical therapy for patients with acute renal colic is parenteral narcotic analgesics. These medications work primarily on the central nervous system to reduce the perception of pain. They are inexpensive and quite effective.
When considering a medication and dosage range, remember that acute renal colic is probably the most painful malady to affect humans. Adverse effects of narcotic analgesics include respiratory depression, sedation, constipation, a potential for addiction, nausea, and vomiting.
Choosing any particular agent tends to be somewhat arbitrary. Morphine, meperidine (Demerol), and butorphanol
(Stadol) are the most commonly used. Butorphanol has some theoretical advantages based on studies that suggest it causes less smooth muscle spasm and respiratory depression than either morphine or meperidine. Butorphanol costs approximately $10/mg, compared with approximately
$0.05/mg for meperidine. One mg of butorphanol is roughly
equivalent in pain relieving efficacy to 20 mg of meperidine, making butorphanol approximately 10 times as costly.
Morphine is the principal opium alkaloid product.
Neutralization with sulfuric acid produces morphine sulfate.
As a potent narcotic analgesic, morphine sulfate controls severe pain primarily through a central nervous system mechanism via specific receptor site interactions. Adverse effects include respiratory depression, drowsiness, mood changes, nausea, vomiting, increases in the cerebrospinal fluid pressure, and cough reflex depression. The most bothersome is respiratory depression caused by a direct effect on the brain stem respiratory center. This effect is most severe in patients who are elderly, debilitated, or both.
The usual dose of morphine sulfate is 10 mg/70 kg of body weight intramuscularly or subcutaneously every 4 hours. The actual dosage required varies according to each individual patient's tolerance and severity of discomfort. For more rapid results, morphine sulfate can be administered intravenously in doses of 4-10 mg but must be administered slowly or in small increments to avoid excessive adverse effects and potentially dangerous respiratory depression.
Meperidine is a potent parenteral narcotic analgesic that is very similar in overall effect to morphine sulfate. Doses of 60-
80 mg of meperidine is roughly equivalent to 10 mg of morphine. Meperidine offers a slightly more rapid onset of action and slightly shorter duration of analgesic activity than morphine sulfate. Some evidence suggests that meperidine may have slightly fewer adverse effects than morphine. The dosage range is usually 50-150 mg IM or SC every 3-4 hours.
This dosage is reduced by at least 50% when administered IV.
The actual effective dosage varies according to the source of the pain and the individual's tolerance. As with morphine sulfate, intravenous administration should be performed slowly. Meperidine is contraindicated in patients taking monoamine oxidase inhibitors.
Naloxone (0.4 mg or 1 mL) is a specific narcotic antagonist for both meperidine and morphine sulfate that can be administered to counteract inadvertent narcotic overdosage or unusual opioid sensitivity. Naloxone has no analgesic properties.
Nalbuphine (Nubain) is a potent parenteral analgesic that is partly antagonistic to narcotics. Its overall effectiveness in relieving pain is equivalent to the opioids. The usual starting dose is 0.5 mg IV or 1-1.5 mg IM every 4-6 hours as needed.
Nonsteroidal anti-inflammatory drugs
The only NSAID approved for parenteral use in the United
States is ketorolac (Toradol). Ketorolac works at the peripheral site of pain production rather than on the central nervous system. It has fewer adverse effects and often provides dramatic improvement in pain symptoms due to renal colic. The dosage is an initial 30-60 mg IM or 30 mg IV followed by 30 mg IV or IM every 6-8 hours. A dose of 15 mg is recommended in patients older than 65 years.
In more severe cases, ketorolac is particularly effective when used together with narcotic analgesics. Oral ketorolac is available in 10-mg pills, but the efficacy of this form in persons with acute renal colic is less clear. Some practitioners use parenteral ketorolac in the hospital but recommend either ibuprofen (Motrin, Advil) or one of the newer oral cyclooxygenase-2 inhibitors (eg, celecoxib [Celebrex], meloxicam [Mobic]) for pain management in outpatients.
A new intranasal ketorolac (Sprix) is now available and may be particularly useful for outpatient use in patients unable to take oral medication. A maximum of 5 days of ketorolac therapy is recommended.
Chemically, ketorolac is similar to aspirin and may increase the prothrombin time when administered with anticoagulants. Ketorolac can increase methotrexate toxicity and phenytoin levels. It is potentiated by probenecid and should be avoided in patients with peptic ulcer disease, renal failure, or recent GI bleeding.
Antiemetics
Because nausea and vomiting frequently accompany acute renal colic, antiemetics often play a role in renal colic therapy. Several antiemetics have a sedating effect that is often helpful. Metoclopramide (Reglan) is the only antiemetic that has been specifically studied in the treatment of renal colic. In 2 double-blinded studies, metoclopramide apparently provided pain relief equivalent to narcotic analgesics in addition to relieving nausea. Its antiemetic effect stems from its dopaminergic receptor blockage in the central nervous system. It has no anxiolytic activity and is less sedating than other centrally acting dopamine antagonists.
The effect of metoclopramide begins within 3 minutes of an intravenous injection, but it may not take effect for as long as
15 minutes if administered IM. The usual dose in adults is 10 mg IV or IM every 4-6 hours as needed. Metoclopramide is not available as a suppository.
Other medications commonly used as antiemetics include promethazine (Phenergan), prochlorperazine (Compazine), and hydroxyzine (Vistaril). The author usually recommends antiemetics when patients with renal colic have been vomiting actively or report nausea sufficient to interfere with oral therapy. They also may be useful as anxiolytics in some cases. While metoclopramide is the antiemetic of choice in the hospital or ED setting, a suppository formulation such as promethazine or prochlorperazine is recommended for outpatient use.
Antidiuretics
Several studies have now demonstrated that desmopressin
(DDAVP), a potent antidiuretic medication that is essentially an antidiuretic hormone, can dramatically reduce the pain of acute renal colic in many patients. Animal studies have demonstrated a significant reduction in mean intraureteral pressure following an acute obstruction in subjects administered desmopressin compared with controls. In human studies, approximately 50% of 126 patients tested
had complete relief of their acute renal colic pain within 30 minutes after the administration of intranasal desmopressin without any analgesic medication. For patients in whom desmopressin therapy failed, suitable analgesics were administered. No adverse effects from the antidiuretic medication occurred.
Desmopressin acts quickly, has no apparent adverse effects, reduces the need for supplemental analgesic medications, and may be the only immediate therapy necessary for some patients. It is available as a nasal spray (usual dose of 40 mcg, with 10 mcg per spray) and as an intravenous injection (4 mcg/mL, with 1 mL the usual dose). Generally, only one dose is administered.
Desmopressin is thought to work by reducing the intraureteral pressure, but it may also have some direct relaxing effect on the renal pelvic and ureteral musculature.
A central analgesic effect through the release of hypothalamic beta-endorphins has been proposed but remains unproved. Whether this therapy significantly affects eventual stone passage is unknown.
While some of the human studies lack adequate controls and further studies must be conducted, desmopressin therapy currently appears to be a promising alternative or adjunct to analgesic medications in patients with acute renal colic, especially in patients in whom narcotics cannot be used or in whom the pain is unusually resistant to standard medical treatment.
Antibiotics
Antibiotic use in patients with kidney stones continues to be controversial. Overuse of the more effective urinary antibiotics leaves only highly resistant bacteria, but failure to adequately treat a urinary infection complicated by an obstructing calculus can result in potentially life-threatening urosepsis and pyonephrosis.
Use antibiotics if a kidney stone or ureteral obstruction has been diagnosed and the patient has clinical evidence of a UTI.
Perform a urine culture in these cases because a culture cannot be performed reliably later should the infection prove to be resistant to the prescribed antibiotic. Evidence of a possible UTI includes an abnormal finding upon microscopic urinalysis, showing pyuria of 10 WBCs per high-power field
(or more WBCs than RBCs), bacteriuria, fever, or unexplained leukocytosis. Approximately 3% of patients being treated for renal colic are reported to develop a newly acquired UTI.
While case numbers are not high, such an infection can dramatically complicate the clinical outcome for that patient.
Base selection of the antibiotic on the patient's presentation, reserving the most effective parenteral antibiotics for patients with frank sepsis or other high-risk characteristics.
The author's preference for initial medical therapy for pain in patients with acute renal colic is to use intravenous or intramuscular ketorolac for pain with metoclopramide for nausea. If this therapy is unsuccessful or if the case is deemed more severe, a narcotic such as morphine sulfate or meperidine is added as needed to control pain. An antibiotic is administered if any question of potential infection exists.
An oral antibiotic is always used if the patient is able to return home.
Aggressive Medical Therapy
Based on data that suggest a higher rate of spontaneous stone passage, fewer days lost from work, and fewer surgeries, some authorities advocate a more aggressive therapeutic medical approach for the period immediately after an acute renal colic attack. This treatment plan is intended for short-term use only but may benefit selected patients who can take medications reliably and can tolerate any adverse effects. The protocol was developed based on the possible causes of failure to spontaneously pass a stone, including ureteral stricture, muscle spasm, local edema, inflammation, and infection. Various common drugs were considered that would potentially benefit these problems, improve spontaneous stone passage, and alleviate renal colic discomfort. The reported regimen consists of the following:
1.
Ketorolac at 10 mg orally every 6 hours for 5 days
2.
Nifedipine XL at 30 mg/d PO for 7 days
3.
Prednisone 20 mg PO twice a day for 5 days
4.
Trimethoprim/sulfamethoxazole DS once a day for 7 days
5.
Acetaminophen (Tylenol) 2 tablets 4 times a day for 7 days
6.
An oral opioid
(oxycodone/acetaminophen) pain as medication needed for breakthrough pain
7.
Prochlorperazine suppository as needed for control of nausea
Nifedipine is indicated for angina, migraine headaches,
Raynaud disease, and hypertension, but it can also reduce muscle spasms in the ureter, which helps reduce pain and facilitate stone passage. Ureteral smooth muscle uses an active calcium pump to produce contractions, so a calcium channel blocker such as nifedipine would be expected to relax ureteral muscle spasms.
Prednisone is an oral corticosteroid that acts as a potent antiinflammatory agent to reduce local edema in the ureter.
Short-term (ie, 5 d) use of prednisone poses little danger of adverse effects and no need for any steroid tapering.
Trimethoprim/sulfamethoxazole is a urinary antibiotic used in this case for prophylaxis, although other urinary antibiotics can be substituted. Even a mild infection can reduce ureteral peristalsis and may reduce spontaneous stone passage.
While acquired urinary infections in patients with stones is uncommon, a 3% reported rate suggests that a prophylactic agent for UTI is not unreasonable, especially considering the complications of a possible proximal infection in a blocked renal unit, particularly in a patient of high medical risk.
Acetaminophen is used for analgesia in addition to the other medications mentioned. Acetaminophen has no anti-
inflammatory activity but raises the pain threshold and reduces the need for narcotic pain medications.
An oral narcotic (oxycodone/acetaminophen) is used as needed to control breakthrough pain. An antiemetic suppository (prochlorperazine 25 mg) is also made available to the patient.
In one study of 70 subjects randomized to receive either standard treatment or the more aggressive medical protocol described above, results showed a 32% increase in stone passage rate and an average of 3 fewer work days lost for the more aggressively treated group than the controls, with no significant difference in adverse effects or complications.
In the author's practice ibuprofen has been substituted for the ketorolac tablets recommended in the original study.
Fewer complications with ibuprofen occur while maintaining efficacy for pain relief. Tamsulosin (Flomax) has also been substituted for the nifedipine based on several published studies indicating that tamsulosin is effective as an antispasmodic in the distal ureter and particularly at the ureterovesical junction.
Alpha-blockers such as tamsulosin are usually used as muscle relaxants for the lower urinary tract. Specifically, tamsulosin is a highly selective alpha1-adrenergic receptor antagonist that has been shown to greatly increase urinary flow rates for patients with symptomatic prostatic hyperplasia. Studies have shown substantial alpha1-adrenergic receptors in the distal ureter and ureterovesical junction, where antagonists such as tamsulosin are able to inhibit basal muscle tone, reduce peristaltic frequency, and weaken ureteral contractions in the distal and intramural ureter. Spontaneous stone passage rates have increased approximately 30% in patients with ureterovesical and distal ureteral stones treated with tamsulosin compared with controls.
Stents
A stent is a hollow plastic tube of varying lengths that is used in various types of urological surgery on the kidney, ureter, and bladder. The most commonly used stent, called a double-
J, forms a coil at either end when the stiffening insertion guide wire is removed. One coil forms in the renal pelvis and the other in the bladder. They are available in lengths from
20-30 cm and in 3 widths of 6F, 7F, and 8.5F. Some are designed to soften after placement in the body; others are rather stiff to resist crushing and obstruction by large stones or external compression with occlusion from an extrinsic tumor or scar tissue.
To select the correct size double-J stent, the author recommends measuring the ureteral length. This is best performed on a retrograde pyelogram film. The distance from the tip of the retrograde catheter to the UPJ is measured in centimeters, using a tape measure. Ten percent of this reading is subtracted to account for the average magnification effect of the film. If the result is an odd number, a double-J stent one size longer is used. The most common lengths used are 26 cm in men and 24 cm in women. Width depends on both the relative diameter and course of the ureter and the purpose of the stent. If the patient has a stricture or a tortuous ureter, a stiffer or largerdiameter stent is placed if possible.
When used for stone disease, stents perform several important functions. They virtually guarantee drainage of urine from the kidney into the bladder and bypass any obstruction. This relieves patients of their renal colic pain even if the actual stone remains. Over time, stents gently dilate the ureter, making ureteroscopy and other endoscopic surgical procedures easier to perform later. Because they are also quite radiopaque, stents provide a stable landmark when performing shockwave lithotripsy. A landmark is particularly important with small or barely visible stones, especially in the ureter because the shockwave lithotripsy machine uses radiographic visualization to target the stone.
Once big stones are broken up, stents tend to prevent the rapid dumping of large amounts of stone fragments and debris into the ureter. The stent forces the fragments to pass slowly, which is more efficient and prevents clogging. Finally, a stent helps prevent any stone in the kidney from passing into the ureter, an important factor for shockwave lithotripsy, which works best on stones within the renal pelvis.
Stents do have drawbacks. They can become blocked, kinked, dislodged, or infected. Checking a double-J stent for malfunction is an important ED procedure. A simple KUB or abdominal flat plate radiograph can be used to determine stent position, while infection is easily diagnosed by urinalysis. A renal ultrasound can sometimes be helpful if the findings are positive for increased dilation. Questionable cases can be evaluated further using a radiographic cystogram or an IVP. The cystogram is performed by filling the urinary bladder with diluted contrast media through a
Foley catheter under gravity pressure. A stent that is unclogged and functioning normally should show free reflux of contrast from the bladder into the stented renal pelvis.
Stents are often quite uncomfortable for patients due to direct bladder irritation, spasm, and reflux. This discomfort can be alleviated by pain medications, anticholinergics (eg, oxybutynin [Ditropan], tolterodine [Detrol]), and topical analgesics (eg, phenazopyridine [Pyridium], Urised).
Percutaneous nephrostomy
In some clinical situations, drainage of an obstructed kidney is necessary and a stent is either inadvisable or impossible to place. In particular, such cases include patients with pyonephrosis who have a urinary infection or urosepsis exacerbated by an obstructing calculus. In these cases, retrograde endourological procedures such as retrograde pyelograms and double-J stent placement may exacerbate the infection by pushing infected urinary material into the obstructed renal unit. These situations clearly indicate the need for a percutaneous nephrostomy, especially in patients who are hemodynamically unstable.
Proximal urinary diversion is usually used to alleviate symptoms such as persistent pain, renal failure, and fever.
Stents require no external appliance for drainage and no skin perforation. They can also be used to localize stones for
ESWL therapy and to passively dilate the ureter for ureteroscopy. Percutaneous nephrostomy can be placed more safely in patients with infection or patients who are unstable, avoiding the bladder irritation that frequently accompanies stent placement. Percutaneous nephrostomy also seems to alleviate symptoms better, reduce patient radiation exposure, require shorter courses of antibiotics, and demonstrate a superior quality of life compared with double-J stents in similar groups of patients with kidney stones, despite the need for an external appliance with the nephrostomy catheter.
Causes of Nephrolithiasis and Preventive Therapy
The most common causes of kidney stones are hypercalciuria, hyperuricosuria, hyperoxaluria, hypocitraturia, and low urinary volume. Each of these major factors can be measured easily with a 24-hour urine sample using one of several commercial laboratory packages now available. Kidney stone preventive therapy consists of dietary adjustments, nutritional supplements, medications, or combinations of these. Discovering the underlying cause of a patient's stones and starting preventive therapy is not the primary responsibility of the ED physician. However, the ED physician is the first medical professional to treat the patient with an acute attack, and the physician should educate the patient and family members about the availability of preventive testing and treatment. When properly performed and evaluated, preventive treatment plans can eliminate virtually all new stone formation from most patients with stones.
Strongly encourage patients who have a stone at a young age
(ie, <25 y), multiple recurrences, a solitary functioning kidney, renal failure, or a history of prior kidney stone surgery to obtain a 24-hour urine collection for stone prevention analysis, especially if they are motivated to comply with a long-term stone prevention program. These 24-hour urine collection kits can be obtained from a number of commercial medical laboratories, including the following:
1.
Dianon Systems, Inc; phone, (800) 328-2666
2.
Mission Pharmacal; phone, (800) 531-3333
3.
LabCorp; phone, (800) 222-7566, extension 63455
4.
Litholink; phone, (800) 338-4333
5.
Quest Diagnostics, Nichols Institute; phone, (800) 642-
4657
6.
UroCor Labs; phone, (800) 634-9330
All of the listed commercial laboratory programs provide good, reliable, basic 24-hour urine metabolic studies at reasonable cost, but only the Comprehensive Kidney Stone
Prevention Program from LabCorp (test # 242339) offers a computerized evaluation report coordinated with the patient's serum laboratory data and the clinical history.
Surgery for Recurrent Renal Colic
Whether calyceal stones cause pain continues to be controversial. In general, in the absence of infection, how a renal stone causes pain remains unclear, unless the stone also causes obstruction. Arguably, proving that a calyceal stone is causing an obstruction can be difficult. However, a stone trapped in a calyx plausibly could block the outflow tract from that calyx, causing an obstruction and subsequent pain. Treatment by ESWL is reasonable for situations in which calyceal stones are suspected of causing symptoms and pain, and ESWL is usually successful. However, indications for using
ESWL for asymptomatic patients with calyceal stones are less clear.
In rare instances of intractable colic due to recurrent stones not amenable to medical prophylaxis, surgical intervention can be used. One approach is to perform an ileal interposition in which a section of ileum is used to replace the ureter. Because the diameter of the ileal segment is considerably greater than the diameter of the ureter, obstruction caused by stones is unlikely. Potential complications include unwanted reabsorption of waste products from the urine passing through the ileal segment and mucus production.
A viable alternative to ileal interposition might be autotransplantation of the affected kidney, with a pyelovesicostomy using a Boari flap as a large-caliber urinary conduit. This has the advantage of bypassing a scarred ureter and avoiding some of the complications of an ileal interposition, such as urinary reabsorption and mucus production.
Summary
Acute renal colic and resultant flank pain is a common and sometimes complex clinical problem. While noncontrast renal colic CT scans have become the standard imaging modality of choice, in some situations a renal ultrasound or a contrast study such as an IVP may be preferred. Many urologists recommend a KUB radiograph in addition to the renal colic CT scan to facilitate their review and follow-up of these patients. Adding contrast to the CT scan study may sometimes help clarify a difficult or confusing case, but the contrast also obscures any calcific stone and causes delays.
Size and location of the stone are the most important predictors of spontaneous passage. Aggressive treatment of any proximal urinary infection is important to avoid potentially dangerous pyonephrosis and urosepsis. In these cases, consider percutaneous nephrostomy drainage rather than retrograde endoscopy, especially in very ill patients.
Aggressive medical therapy has shown promise in increasing the spontaneous stone passage rate and relieving discomfort while minimizing narcotic usage.
A stone chemical composition analysis should be performed whenever possible, and information should be provided to motivated patients about possible 24-hour urine testing for long-term nephrolithiasis prophylaxis. This is particularly
important in patients with only one functioning kidney, those with very high medical risk factors or renal failure, those who have undergone renal transplantation, and all children.
However, any strongly motivated patient can benefit from a prevention analysis and prophylactic treatment if they are willing to pursue long-term therapy.