Improving depression management within the haemodialysis
advertisement
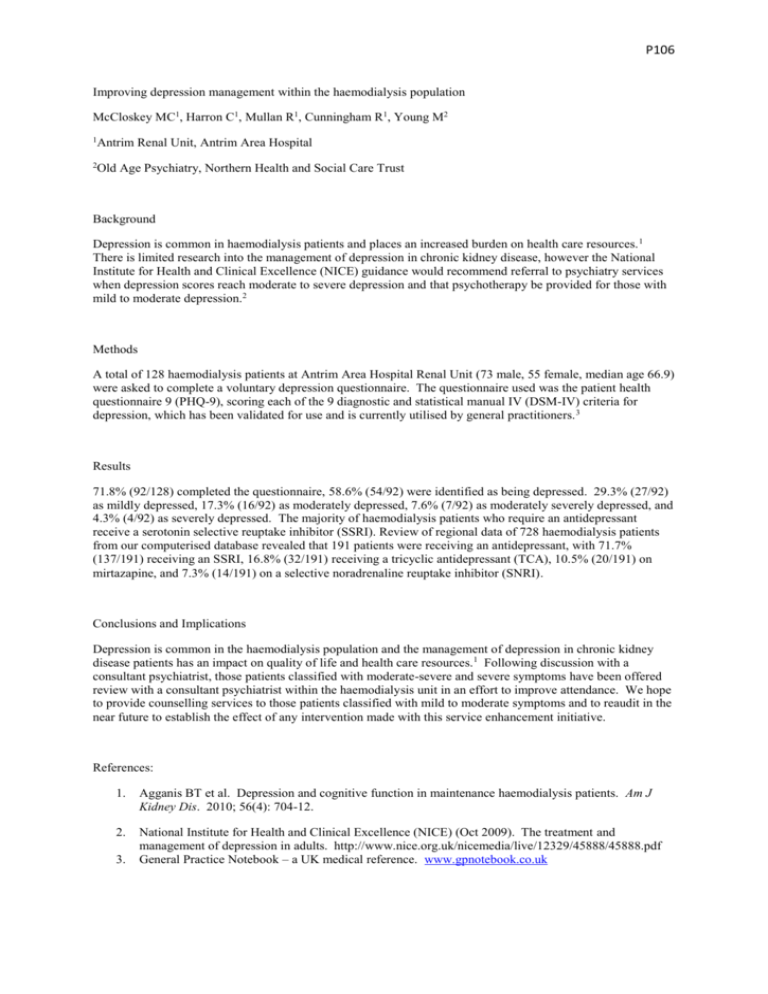
P106 Improving depression management within the haemodialysis population McCloskey MC1, Harron C1, Mullan R1, Cunningham R1, Young M2 1 Antrim Renal Unit, Antrim Area Hospital 2 Old Age Psychiatry, Northern Health and Social Care Trust Background Depression is common in haemodialysis patients and places an increased burden on health care resources. 1 There is limited research into the management of depression in chronic kidney disease, however the National Institute for Health and Clinical Excellence (NICE) guidance would recommend referral to psychiatry services when depression scores reach moderate to severe depression and that psychotherapy be provided for those with mild to moderate depression.2 Methods A total of 128 haemodialysis patients at Antrim Area Hospital Renal Unit (73 male, 55 female, median age 66.9) were asked to complete a voluntary depression questionnaire. The questionnaire used was the patient health questionnaire 9 (PHQ-9), scoring each of the 9 diagnostic and statistical manual IV (DSM-IV) criteria for depression, which has been validated for use and is currently utilised by general practitioners. 3 Results 71.8% (92/128) completed the questionnaire, 58.6% (54/92) were identified as being depressed. 29.3% (27/92) as mildly depressed, 17.3% (16/92) as moderately depressed, 7.6% (7/92) as moderately severely depressed, and 4.3% (4/92) as severely depressed. The majority of haemodialysis patients who require an antidepressant receive a serotonin selective reuptake inhibitor (SSRI). Review of regional data of 728 haemodialysis patients from our computerised database revealed that 191 patients were receiving an antidepressant, with 71.7% (137/191) receiving an SSRI, 16.8% (32/191) receiving a tricyclic antidepressant (TCA), 10.5% (20/191) on mirtazapine, and 7.3% (14/191) on a selective noradrenaline reuptake inhibitor (SNRI). Conclusions and Implications Depression is common in the haemodialysis population and the management of depression in chronic kidney disease patients has an impact on quality of life and health care resources. 1 Following discussion with a consultant psychiatrist, those patients classified with moderate-severe and severe symptoms have been offered review with a consultant psychiatrist within the haemodialysis unit in an effort to improve attendance. We hope to provide counselling services to those patients classified with mild to moderate symptoms and to reaudit in the near future to establish the effect of any intervention made with this service enhancement initiative. References: 1. Agganis BT et al. Depression and cognitive function in maintenance haemodialysis patients. Am J Kidney Dis. 2010; 56(4): 704-12. 2. National Institute for Health and Clinical Excellence (NICE) (Oct 2009). The treatment and management of depression in adults. http://www.nice.org.uk/nicemedia/live/12329/45888/45888.pdf General Practice Notebook – a UK medical reference. www.gpnotebook.co.uk 3.