OS 213 Lec 15: Leptospirosis OS 217: Infectious Diseases Lec 19
advertisement

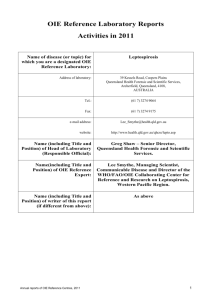
OS 217: Infectious Diseases 1 Lec 19: Leptospirosis Dr. Evalyn A. Roxas, MD, FPCP. DPSMID TOPIC OUTLINE I. II. III. IV. V. VI. VII. VIII. IX. X. XI. Introduction Epidemiology Causative Agent Pathogenesis Natural Course of the Disease and Manifestations A. Leptospiremic Phase B. Leptospiruric Phase Classification of Leptospirosis A. Mild B. Moderate to Severe C. Weil’s Syndrome Diagnosis A. WHO Criteria for Definitive Leptospirosis B. Laboratory Diagnosis C. Faine’s Criteria Treatment Prophylaxis Management of Complications A. Acute Kidney Injury B. Pulmonary Involvement Prevention and Control I. INTRODUCTION 1. Leptospirosis infectious, zoonotic disease asymptomatic infection to severe and fatal illness usually peaks after periods of high rainfall storms Most important reservoir are rats; Others: domestic/wild animals (dogs, cats, swine, cattles, raccoons,) Transmission – contact of mucous membranes or broken skin with water, moist soil or vegetation contaminated with the urine of infected animals Incubation period - 10 days (2-30 days) II. EPIDEMIOLOGY Actual incidence of leptospirosis in the Asia Pacific region is not well-documented, similar to the situation in many regions worldwide Aside from under reporting, incidence data are further compromised by the unavailability of laboratory diagnosis Within the Asia pacific region, Southeast Asia and Oceania have the highest incidence of leptospirosis. Philippines has moderate incidence of leptospirosis in the Asia pacific Region (1 to 10 annual incidence per 100,000) along with China, mainland India, Indonesia and Malaysia Prevalent Leptospira serovars (1960-1970) Pyrogenes, Bataviae, Pomona, Grippotyphosa, Manilae and Javanica Outbreaks of leptospirosis due to flooding were reported in prisons, penal farms, and in many parts of the country DOH statistics after typhoon Ondoy (October 27, 2009) o Total Leptospirosis Cases = 2,292 o Mortality = 178 (7.6%) From 2016 trans: Endemic throughout the world May be the most common zoonosis o Temperate zones: 0.1 to 1/100,000/year o Tropics: >10/100,000/year o Outbreaks: >100/100,000 may be affected Peak incidences o Tropics: Rainy season o Temperate regions: Late summer to fall Shen, Franz, Jerry Underdiagnosed due to wide range of presenting clinical pictures Reasons for resurgence of leptospirosis o Rapid urbanization o Forested areas converted to residential or business zones o Forested areas has decreased from 70% in 1900 to 18% in 1999 o Typhoons hit the country an average of 20x/yr with associated heavy rainfall o Flooded areas are expanding o Drainage, creeks, esteros are clogged with garbage o Poor waste disposal system o Rat infestation Pathogenic Leptospires o long corkscrew-shaped bacteria, too thin to be visible under the ordinary microscope o dark-field microscopy is required Phenotypic classification o Genus Leptospira o Species L. interrogans (pathogenic) o L. biflexa (saprophytic) 240 pathogenic serovars Clinical Legends: From the Powerpoint presentation From the lecturer From other sources (textbook, Internet, etc.) From 2016 September 10, 2014 III. CAUSATIVE AGENT Table 1. Prevailing Leptospira serovars in humans in the Philippines Prevailing Serovars Pyrogenes Grippotyphosa Autumnalis Hardjo Bataviae Manilae Icterohemorrhagiae Poi Pomona Javanica Hyos Tarrasoni 1. Natural Habitat o Leptospires can be: o Free living in water, soil or sewage contaminated with the animal urine; or o Associated with renal infection with animals o Incidence is high in warm climate countries because they survive longer in humid condition. o Saprophytic leptospires – free-living organisms found in wet or humid environments ranging from surface waters and moist soil to tap water o Saprophytic halophilic leptospires – found in seawater 2. Transmission o Human become incidental/ accidental host: o direct contact with infected animals, or o indirectly through contact with water contaminated with excreta. o Human infections can be acquired through occupational (rice field fever, cane cutter’s disease, swineherd’s disease, dairy farm fever, mud fever) and recreational exposures o Human to human transmission is rare by sexual intercourse, transplacentally from mother to fetus, via breast milk 3. Transmission Cycle o Mammals are the maintenance host of leptospires o an MH is a carrier animal/specie which becomes a reservoir of a distinct serovar o includes rodents, livestock, companion animals o MH do not show signs of illness but once infected shed the organism in their urine for life o Pathogenic leptospires are maintained in the renal tubules o Transmission of leptospires requires continuous circulation of the pathogen among maintenance hosts o Leptospires survive for weeks or months in moist soil and water after excretion in the urine o Cell aggregation and biofilm formation contribute to survival of leptospires outside their hosts o Knowledge on the prevalent serovars and their maintenance host is essential for epidemiologic identification. Page 1 / 8 Lec 15: Leptospirosis 4. Persistent Colonization o Essential component of the life cycle of pathogenic leptospires is persistent renal carriage in reservoir animals o In rats, systemic infection occurs but is subsequently cleared from all organs except the renal tubules o Colonized tubules are densely populated with leptospires which aggregate into an amorphous biofilm o Expression of LPS O antigen facilitates carriage in the tubules o Renal tubule is an immunopriviledged site, contributing to high-grade persistence of the pathogen Figure 1. The Cycle of Leptospiral Infection IV. PATHOGENESIS o o o o o o o o o o o o Organism gains entry in the body through o skin abrasions or cuts o intact mucosa: conjunctiva, oro/nasopharynx, gut o waterlogged skin o inhalation of droplets of urine o ingestion of contaminated water or food After entry, it multiplies in the blood and tissues including CSF Leptospires can damage the wall of small blood vessels causing vasculitis Vasculitis is responsible for the most important manifestations of the disease. The most important known pathogenic properties of leptospires are adhesion to cell surfaces and cellular toxicity Kidneys o Leptospires migrate to the interstitium, renal tubules, and tubular lumen, causing interstitial nephritis and tubular necrosis. o Much recent work has focused on the role of surface lipoprotein The major surface lipoprotein seen among pathogenic serovars, LipL32 LipL32 is the major target of the human immune response and is involved in pathogenesis of tubulointerstitial nephritis Liver o Centrilobular necrosis with proliferation of Kupffer cells o Severe hepatocellular necrosis is not a feature of leptospirosis o Liver involvement – not a feature of severe leptospirosis Pulmonary o Involvement is the result of hemorrhage and not of inflammation o Pulmonary hemorrhage is secondary to vasculitis, not thrombocytopenia Skeletal Muscle o Invasion of leptospires results in swelling, vacuolation of the myofibrils and focal necrosis o Skeletal muscle involvement – manifests as calf tenderness Prolonged leptospiremia until the host mounts an effective immune response Leptospires evade the host innate immune response during the initial stages of infection; resist the alternative pathway of complement activation Widespread hematogenous dissemination and penetration of tissue barriers o Facilitated by systemic vasculitis Pulmonary haemorrhage Acute tubular necrosis Destruction of hepatocytes Shen, Franz, Jerry o o o o OS 213 Onset of disease correlates with appearance of agglutinating antibodies and clearance of leptospires by antibody-mediated opsonization and lysis Vascular endothelial damage – hallmark of severe leptospirosis causing capillary leakage, hemorrhagic gastroenteritis, vasculitis Activation of coagulation cascade causing DIC Production of pro-inflammatory cytokines which mediate inflammation and damage of end-organ tissues 1. Determinants of Disease o Host susceptibility factors – HLA DQ6 o first genetic susceptibility factor identified o synergism between HLA-DQ6 and environmental exposure found during the triathlon outbreak is the first gene-envt interaction to be identified for an infectious disease o Dose of infecting inoculum o Virulence characteristics of the infecting strain, which include: o Surface proteins which mediate interaction between bacteria and host tissues o Loa22 – first virulence factor gene exposed on bacterial surface o Motility of leptospira and its ability to swim through viscous media; impt in the initial infection and dissemination of organisms from site of entry to sites of end-organ o Hemolysins, proteases, sphingomyelinase, microbial collagenase o Leptospiral LPS is less toxic than the gram negative LPS, activates macrophages via TLR2 instead of TLR4 2. o o o o o o o Determinants of Disease Incubation period : 5-14 d, range 2-30 d Febrile illness which resolves after the first week of symptoms 5-15% develop severe leptospirosis Severe late phase manifestations occur 4-6 days after onset of illness but may vary depending on inoculum dose Classic presentation o Septicemic phase (5 to 7 days) o Interphase (1 to 3 days) o Immune phase (4 to 30 days) In severe cases, no distinct phases Some present only with immune phase Figure 2. Disease Kinetics of Leptospirosis V. NATURAL COURSE OF THE DISEASE AND CLINICAL MANIFESTATIONS 1. Natural Course of the Disease (see Appendix 1) A. Leptospiremic/Septicemic Phase o first week after entry, proliferation of spirochetes, appearance of systemic/non-specific manifestations (see manifestations in accompanying slides/pictures) o High remittent fever o Headache, chills, rigors, myalgias Page 2 / 6 Lec 15: Leptospirosis o o o o o o o B. Conjunctival suffusion without discharge and calf tenderness are most specific findings Anorexia, nausea, vomiting Abdominal pain Cough, pharyngitis Pretibial maculopapular eruption U/A: mild proteinuria, pyuria, hematuria with or without hyaline/granular casts Death rare in this phase of illness OS 213 Severe pulmonary hemorrhages Cardiac involvement Weil’s Syndrome Most severe form of leptospirosis Manifests as: o Profound jaundice o Renal dysfunction o Hepatic necrosis o Pulmonary dysfunction o Hemorrhagic diathesis Leptospiruric/ Immune Phase o Second week; immune phase or production of antibodies against the spirochetes; appearance of more specific signs and symptoms o Weil’s Disease - Impaired hepatic function Disturbance of liver function out of proportion to pathologic findings (mild and nonspecific) Degenerative changes in hepatocytes Kupffer cells are hypertrophied Cholestasis, erythrophagocytosis Mononuclear cell infiltrates Necrosis almost absent Direct bilirubin > 80 mg/dL AST and ALT ≤ 200 U/L Jaundice is slow to resolve BUN usually < 100 mg/dL Crea 176 – 707 mg/dL Initially non-oliguric hypokalemic renal insufficiency Impaired sodium reabsorption (loss of ENaC channel in proximal tubule) Increased distal sodium delivery Potassium wasting Progresses to oliguric renal failure if electrolyte and volume losses are not replaced 3 most common manifestations: fever, headache, myalgia; however, diarrhea is becoming a more common manifestation in a recent study C. Clinical Manifestations Many Leptospira-infected persons remain asymptomatic Among the symptomatics, more than 90% have relatively mild and usually anicteric form of leptospirosis Severe leptospirosis develops in only 5-10% of infected individuals D. When to Suspect Leptospirosis? Any individual with acute febrile illness of at LEAST 2 days Residing in a flooded area OR High risk exposure (Wading in flood waters, contact with contaminated animal fluids, swimming in or ingestion ofcontaminated water ) At LEAST 2 of the following symptoms: o Myalgia o Calf tenderness o Conjunctival suffusion o Chills o Abdominal Pain o Headache o Jaundice o Oliguria VI. CLASSIFICATION OF LEPTOSPIROSIS WHO NEEDS HOSPITAL ADMISSION? A. Mild – outpatient management Stable vital signs Anicteric sclerae Good urine output (-) Meningismus (-) Sepsis/ Shock (-) Dyspnea (-) Jaundice Tolerates oral medications B. Moderate to Severe – requires hospitalization Unstable vital signs Jaundice/ icteric sclerae Abdominal pain Nausea, vomiting, diarrhea Oliguria/ anuria Meningeal irritation Sepsis/ Shock Altered sensorium Difficulty breathing Hemoptysis Figure 3. Common Presenting Features of Leptospirosis Mild leptospirosis Fever Body aches (severe myalgia) Headache Conjunctival suffusion Diarrhea &/ or vomiting Moderate to severe leptospirosis Jaundice Fever > 40 C Hypotension Active Bleeding Oligura/Anuria Sensorial changes Shen, Franz, Jerry Basis for determining management E. Weil’s Syndrome VII. DIAGNOSIS A. WHO Criteria for Definitive Leptospirosis a. Positive leptospiral culture of the blood and/or urine b. High positive single lepto Microagglutination Test (MAT) titer of 1:1600 c. Seroconversion from initial MAT negative to a positive antibody titer d. Fourfold rise in antibody titers by MAT from acute to convalescent Page 3 / 6 Lec 15: Leptospirosis B. Laboratory Diagnosis 1. Direct Detection Method Gold standard is culture isolation of the organism Uses specialized culture media (EMJH or Fletcher’s) Additional/alternative test: Korthof Media; (+) Dinger’s Ring: whitish aggregation indicative of growth of spirochetes 2. Indirect Detection Method [Microagglutination Antibody Test for Leptospirosis (MAT)] Utilizes live antigens of leptospires (non-pathogenic) against patient’s serum and examined under dark field for agglutination Genus specific MAT o Uses Leptospira biflexa as live antigen o Available only in UP- PGH Medical Reseach Laboratory o 10 to 12 leptospiral serovars prevalent in the country MAT Postive – a single antibody titer of 1:200- 1:800 (locally, 1:1600) Cross reactions: syphilis, relapsing fever, Lyme disease, viral hepatits, HIV, legionellosis, autoimmune disease Interpretation of MAT o MAT Positive a single antibody titer of 1:200 to 1:800 (locally, the cut-off is 1:1600 because of the prevalence in the country) Preferably, a fourfold or greater rise in titer is detected between acute- and convalescent-phase serum specimens. Initial high titer of 1:1600 Seroconversion Interpretation of MAT results: o Probable Cases -– cases combining with epidemiologically suggestive features with compatible clinical, laboratory, and radiographic findings, with no other diagnosis envisioned o Confirmed case -– finding microorganism on direct examination or culture of blood or urine or seroconversion or by a significant increase in the antibody titer between two samples e. Faine’s Criteria (see Appendix 2) also used for prognostication; not definitive Based on WHO Faine’s Criteria o Scoring system for diagnosis of Leptospirosis on the basis of clinical, epidemiological and laboratory data (A+B+C). o Current Leptospirosis : Score of ≥26 when using PART A, PART A+B Score of ≥ 25 using PART A+B+C Modified Faine’s Criteria o Sensitivity – 58 % o Specificity – 97 % o Positive Predictive Value – 86 % o Negative Predictive Value – 90 % Clinical Utility of Modified Faine’s Criteria in the Diagnosis of Leptospirosis o The sensitivity (Sn) of the Modified Faine’s Parts A+B (4%, 95% CI 1 to 8) increased with the addition of Part C (73%, 95% CI 64 to 81). o Initial high titer MAT was most sensitive at a cut-off titer level of 1:400 (57%, 95% CI 48 to 67). o No significant correlation was found between disease severity and either time to culture positivity (p=0.74) or initial MAT titer levels (p=0.16). Clinical Diagnosis based on WHO Faine’s Criteria o Inclusion of malaise, chills and oliguria, and revision of the point allocation and the use of MAT titer level of 1:400 resulted in a criteria with a significantly higher Sn (95%, 95% CI 92 to 99%) o Conclusion: The Modified Faine’s Criteria did not reflect local leptospirosis symptomatology. Taken singly, the diagnostic utility of Lepto IgM test, initial high titer MAT and Modified Faine’s Criteria remained poor. However, revision of the Modified Faine’s symptom checklist and scoring based on local data plus reassessment of the cut-off values for MAT yielded a criterion of greater clinical utility in the diagnosis of leptospirosis. Shen, Franz, Jerry OS 213 VIII. TREATMENT Table 2. Treatment of Mild and Moderate-Severe Leptospirosis Primary Drug Alternative Drug Mild Leptospirosis Doxycycline Amoxicillin 500 mg 100 mg BID PO x 7 q 6 hours PO or 1g days q8 Azithromycin Dihydrate 1g initially then 500 mg OD PO x 2 more days Moderate to Severe Penicillin G1.5 Ceftriaxone 1gm M IV q 6 hours x 7 IV q 24 hours Leptospirosis Ampicillin 0.5-1gm days IV q 6 hours Azithromycin dihydrate 500 mg OD x 5 days Cefotaxime 1gm IV q 6 hours 1. The Evidence Doxycycline for anicteric leptospirosis in Panama showed a reduction in the duration of fever Randomized controlled trial involving 42 patients with severe leptospirosis showed that length of febrile period, length of hospital stay, creatinine level, and leptospiruria was significantly shorter in the penicillin group compared to placebo Prospective, open-label, randomized trial in Thailand: ceftriaxone and IV penicillin had comparable treatment outcomes in terms of duration of fever, duration of organ dysfunction, and mortality rate in severe leptospirosis. 2. Cost-effectiveness Empiric treatment is potentially cost-effective Early treatment resulted in fewer hospitalizations and complications Cost per patient with doxycycline was low 3. Jarisch-Herxheimer Reactions Systemic reaction resembling bacterial sepsis Begins 6-8 hours after administration of penicillin Sudden rise and gradual fall in body temperature and blood pressure Abrupt onset of chills, myalgia, headache, tachycardia, hyperventilation, vasodilation with flushing, obtundation Peripheral leukocytosis and lymphopenia Postulated etiology - inflammatory process that results from activation of the cytokine cascade (increase IL-1 and IL-6) secondary to release of heat stable protein from degenerating spirochetes. Patients receiving penicillin should be monitored for these reactions No report of a Jarisch-Herxheimer reaction in leptospirosis patients given Penicillin IX. PROPHYLAXIS 1. Pre-exposure Prophylaxis Pre-exposure prophylaxis: NOT ROUTINE. However if you feel that you are of high risk of acquiring leptospirosis such as that you will be engaging in water-related recreational and occupational activities, pre exposure prophylaxis can be taken Pre-exposure prophylaxis for high risk exposure (e.g. travelers, soldiers, those engaged in water-related recreational and occupational activities) Recommended: Doxycycline 200mg once weekly starting 1-2 days pre-exposure continued throughout the period of exposure o Contraindications Pregnant Breast feeding mother Children younger than 8 years, can cause permanent yellowing or graying of teeth Allergic reaction Page 4 / 6 Lec 15: Leptospirosis o Doxycycline can make your skin more sensitive to sunlight and sunburn as a result o May also make birth control pills less effective o Don’t lie down for an hour following doxycycline intake to prevent pill esophagitis o If 200 mg OD is not tolerated, take doxycycline 100 mg capsule BID Pregnant Patients: NO Recommendation 2. Post-exposure Prophylaxis Patients who actually waded in floodwater Risk exposure assessment o LOW-RISK EXPOSURE- single history of wading in flood or contaminated water without wounds, cuts or open lesions of the skin o MODERATE-RISK EXPOSURE- single history of wading in flood or contaminated water with wounds, cuts, or open lesions of the skin OR accidental ingestion of contaminated water o HIGH-RISK EXPOSURE- individuals with continuous exposure of wading in flood or contaminated water with or without wounds, cuts or open lesions of the skin; Swimming in flooded waters especially in urban areas Individuals should continue to monitor themselves for fever and other flu-like symptoms and should continue to wear personal protective measures since antibiotic prophylaxis is not 100% effective. OS 213 Wasting sodium and potassium defect has been consistently documented C. Management of ARF Indications for dialysis o any of the ff: ARDS, ph <7.2, HCO3 <10, CrCl < 20 ml/min, K> 5 o for hypovolemic patients, persistent oliguria despite hydration and vasopressors o for hypervolemic or euvolemic patients, persistent oliguria despite furosemide D. Prognosis of ARF Full renal recovery is the rule within two weeks after clinical improvement Impaired capacity to concentrate urine osmolarity may last for up to 6 months D. Prognosis of ARF 196 consecutive cases of lepto-associated AKI from 1985-2006 in Fortaleza, Brazil Crackles (OR 5.2, 95% CI 1.9 to 14.4) Elevated direct bilirubin levels (OR 1.05, 95% CI 1.001 to 1.093) See Appendix III for the algorithm for the management of oliguria in leptospirosis 2. Pulmonary Involvement (see Appendix 4) A. Clinical Features Tachypnea (RR >30) – First Sign New onset cough, dyspnea and hemoptysis Symptoms appear on the 4th to 6th day of disease chest pain, cough, dyspnea, hemoptysis, ARDS Occur in both anicteric and icteric leptospirosis Severity of pulmonary disease is unrelated to jaundice Smoking – risk factor for devt of pulmo manifestations See Appendix IV for the algorithm for the diagnosis and management of leptospirosis with pulmonary complications. B. Complications Acute Respiratory Distress Syndrome Pulmonary Hemorrhage usually associated with worse prognosis and high mortality In a multicenter retrospective analytical study of leptospirosis patients after typhoon Ondoy last 2009, most of pulmonary hemorrhage is the only significant complication and 71 % of those who died had pulmonary hemorrhage In the same study, pulmonary hemorrhage is the only significant predictor for mortality In a study done at National Kidney and Transpalnt Institute, determing the predictors for dialysis, pulmonary hemorrhage is also a significant predictor of mortality. Figure 4. Post-exposure Prophylaxis recommended by the Lepto Task Force algorithm as X. MANAGEMENT OF COMPLICATIONS 1. Acute Kidney Injury (see Appendix 3) a. Clinical Features Mild proteinuria to severe anuric acute renal failure COMMONLY – Non-oliguric renal failure with mild hypokalemia Poor Prognosis: Oliguria with hyperkalemia B. Acute Renal Failure Occurs in 16-40% of severe leptospirosis May present as isolated proteinuria to severe anuric ARF Non-oliguric forms have better prognosis Oliguria and hyperkalemia identified as predictors of a lethal outcome Commonly presents as a non-oliguric and a hypokalemic state, low potassium levels may be detected in 41%-45% of patients Shen, Franz, Jerry C. Management Leptospires = release of inflammatory mediators = vasculitis = pulmonary involvement in leptospirosis; hence there is a possible role for steroids in treatment Methylprednisolone (1 g IV bolus) preferably given within 12 hrs of onset of respiratory involvement Methylprednisolone should be given for 3 days o Methylprednisolone with non-invasive ventilation is lifesaving in ARDS owing to leptospirosis -Abraham Ittyachen et al. Methylprednisolone as an adjuvant treatment of ARDS owing to Leptospirosis. Indian J Crit Care Med. July-Sept 2005. o Corticosteroids reduce mortality and change outcome significantly when used early in the management of pulmonary leptospirosis – Shenoy, VV. Et. Al. Pulmonary leptospirosis: an excellent response to bolus Methylprednisolone. Postgrad Med J 2006;82:602–606 o On the other hand, In a retrospective study on patients with leptospirosis with pulmonary involvement admitted to PGH from 2003 to 2006 comparing the mortality rates among patients given adjunctive steroids, there was No reduction in mortality and assisted ventilation were observed among those given steroids. However, there was A trend towards a reduction in dialysis rates, but it was not significant. – Villanueva, R. Use of Steroids in Leptospirosis to Improve Survival: An Exploratory Study. Page 5 / 6 Lec 15: Leptospirosis OS 213 Shift to oral Prednisone 1 mg/kg/day for 7 days D. Steroids for Severe Leptospirosis Case reports on the use of glucocorticoids in severe cases 24 patients successfully treated with 7-day course of amoxicillin and steroids (prednisone 60 mg OD x 7 days, MPPT x 3 days, or Hydrocortisone 200 mg LD then 100 mg q6) in 1978 in Hungary 1 patient treated successfully with Hydrocortisone 200 mg LD then 100 mg q6, presenting with thrombocytopenia and bleeding, in the US 1 patient in France with multiple organ failure with methyprednisolone 500 mg and IV immunoglobulin XI. PREVENTION AND CONTROL Leptospirosis is a preventable disease Control measures o Risk communications - Leptospirosis has been considered an occupational disease, thus control measures towards agriculture and other at risk workers o Improvement in sanitation and living conditions o Rodent control o Prophylactic and therapeutic medical o Vaccination On going research into numerous vaccine preparations for humans and animals is well documented The local variability in serovars of endemic leptospiral strains complicates the development of vaccine that can be used worldwide In the Region, human vaccines against Leptospira are available in China, Japan, Korea and Vietnam Vaccine Development o Whole-leptospire based vaccines administered to livestock & domestic animals associated with high rates of adverse reactions; short-term serovar specific immunity o Subunit vaccine candidates that will protect against multiple Leptospira sp o Determine whether infection with leptospira protects against reinfection in high-risk populations and identify mechanisms of immunity o Protective Immunity Serovar-specific Abs against leptospiral LPS are protective Patient is immune to reinfection with the same serovar as long as the Ab titer is high enough mmunity is serovar-specific 1. Control of Infection Source Control of rodent population Separation of animal reservoirs from human habitations by fences or screens Removal of rubbish, garbage disposal system Keep surroundings clean Sewerage, drainage system Do not leave food around especially in recreational areas where rats may be present 2. Interruption of Transmission Avoid high-risk exposure o Immersion in freshwater o Contact with animals and urine-contaminated soil, food and water Protective measures o Boots, goggles, overalls, gloves o Avoid walking barefoot o Cover wounds with waterproof dressing END Shen, Franz, Jerry Page 6 / 6 APPENDIX 1. Natural Course of Disease Appendix B. Faine’s and Modified Faine’s Criteria Shen, Franz, Jerry Page 7 / 8 Lec 15: Leptospirosis OS 213 Appendix 3. Algorithm for the Management of Oliguria in Leptospirosis Appendix 4. Algorithm for the Diagnosis and Management of Leptospirosis with Pulmonary Involvement Shen, Franz, Jerry Page 8 / 6