SPS3: Secondary Prevention of Small Subcortical Strokes Objective
advertisement

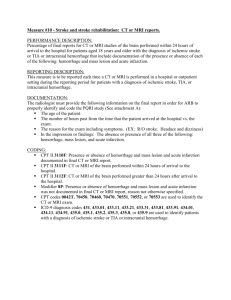
SPS3: Secondary Prevention of Small Subcortical Strokes Objective: To define efficacious therapies for prevention of stroke recurrence and cognitive decline in patients with symptomatic small subcortical stroke/subcortical TIA Specific Hypotheses: 1. Combined antiplatelet therapy will reduce recurrent stroke by 25% relative to aspirin therapy alone 2. Aggressive blood pressure lowering will reduce recurrent stroke by 25% relative to usual management Study Design (Treatment) Antiplatelet therapy: aspirin (325 mg/d, enteric coated) vs. aspirin + clopidogrel (75 mg/d) (double-blinded) Targeted blood pressure control: usual (systolic 130-149) vs. aggressive (systolic < 130 mmHg) (blinded event adjudication) Number of Subjects: 3000 patients randomized equally to four cells Inclusion/Exclusion Criteria Inclusion Criteria Inclusion criteria are based on TOAST criteria supplemented by required MRI data. All of the following criteria must be met, and the patient must be randomized within 6 months of the qualifying event defined s a small subcortical stroke or a *sub-cortical TIA with corresponding lesion on DWI. * The rationale for including TIAs with positive DWI is based on the evidence that TIA patients have a risk of stroke that is similar to that of patients with minor stroke. A population-based prospective cohort study found the early risk of stroke after TIA at 30 and 90 days was 12% and 17% respectively. For patients with minor stroke, the risk during of the corresponding time intervals was 15% and 18%. In addition, the presence of abnormalities on DWI on TIA patients, was found to be an independent predictor of stroke (OR 5.02, CI, 1.37-18; p=0.015) 1. One of the following lacunar clinical syndromes (adapted from Fisher) lasting > 24 hrs: a. Pure motor hemiparesis (PMH) b. Pure sensory stroke c. Sensorimotor stroke d. Ataxic hemiparesis e. Dysarthria-clumsy hand syndrome f. Hemiballism g. PMH with facial sparing h. PMH with horizontal gaze palsy i. PMH with contralateral III palsy j. PMH with contralateral VI palsy k. Cerebellar ataxia with contralateral III palsy l. Pure dysarthria 2. Absence of signs or symptoms of cortical dysfunction such as aphasia, apraxia, agnosia, agraphia, homonymous visual field defect, etc. 3. No ipsilateral cervical carotid stenosis (50%) by a reliable imaging modality done in an approved laboratory since the qualifying S3, if hemispheric. 4. No major-risk cardioembolic sources requiring anticoagulation or other specific therapy. Minor-risk cardioembolic sources will be permitted if anticoagulation is not prescribed by the patient’s primary care physician. Major risk sourcesa: Minor risk sourcesc: Atrial fibrillation Mitral valve prolapse + Marantic endocarditis myxomatous changes Mitral stenosis Mitral annular calcification Prosthetic cardiac valves Patent foramen ovaled Recent (< 3 mos transmural MI) Atrial septal aneurysm LV thrombus, especially if mobile Calcific aortic stenosis or protruding LV wall abnormalities (without thrombus) Atrial myxomas Infective endocarditis Non-ischemic dilating cardiomyopathiesb aAssociated with a substantial absolute risk of stroke, firmly linked to an embolic mechanism bRisk varies with the type and severity cAssociated with a low or uncertain absolute risk of initial or recurrent stroke or are incompletely established as direct embolic source dIf associated with pulmonary hypertension with sustained right-to-left shunting and venous source of emboli, it is a major risk. 5. MRI evidence of S3, specifically both A and B: A. S3 on MRI: at least one of the following four specific criteria i. Diffusion-weighted imaging lesion < 2.0 cm in size at largest dimension (including rostro-caudal extent), confirmed by ADC image, and corresponding to the clinical syndrome. This criterion must be met when the qualifying event is a TIA. The repeat MRIs that were required for patients with acute lesions > 1.5 cm and ≤ 2.0 cm have been eliminated. This is based on the results of an analysis that was performed on the initial 42 repeat MRIs. The baseline MRI was done, on average, 4.4 (SD=7.7) days after the qualifying stroke. On second MRI, 42 (100%) had a cavitated (hypointense) lesion on FLAIR. The average reduction in size between MRIs was 42% [0.85 (SD=0.6) cm]. In 81% of the repeat MRIs the lesion was reduced to ≤1.5 cm (mean 1.0, std 0.3) and in the remainder, all were ≤2.0 cm (mean 1.8, std 0.2). Based on the results of this analysis, it is clear that acute MRI infarcts on DWI overestimate the final lesion size and that the size of the chronic infarct (cavitated lesion on FLAIR) corresponds to classical lesion size described on pathology. ii. Well delineated focal hyperintensity < 2.0 cm in size at largest dimension (including rostro-caudal extent) on FLAIR or T2 and clearly corresponding to the clinical syndrome. If other focal hyperintensities are present, contact the Coordinating Center prior to randomization to discuss the case. The date of imaging must be within 2 months of date of qualifying stroke. If diffusion-weighted imaging is negative, this criterion alone is not sufficient for study entry. iii. Multiple (at least 2) hypointense lesions of size 0.3-1.5 cm at largest dimension (including rostro-caudal extent) only in the cerebral hemispheres on FLAIR or T1 in patients whose qualifying event is clinically hemispheric. If qualifying event is clinically brainstem or cerebellar, this criterion alone is not sufficient for study entry. iv. Well delineated hypointense lesion < 1.5 cm in size at largest dimension (including rostro-caudal extent) on FLAIR or T1 corresponding to the clinical syndrome. MRI must be done at least 1 month after the qualifying stroke. B. Absence of cortical stroke and large (> 1.5 cm) subcortical stroke, recent or remote. Note: “Microbleeds” < 2 mm in diameter detected by diffusion tensor imaging or other special sequences do not exclude the patient. Exclusion criteria: To be eligible for entry into the study, the patient must not meet any of the criteria listed below: 1. Disabling stroke (Modified Rankin Scale 4) 2. Previous intracranial hemorrhage (excluding traumatic) or hemorrhagic stroke 3. Age under 30 years 4. High risk of bleeding (e.g. recurrent GI or GU bleeding, active peptic ulcer disease, etc) 5. Anticipated requirement for long-term use of anticoagulants (e.g. recurrent DVT) or other antiplatelets 6. Prior cortical stroke (diagnosed either clinically or by neuroimaging), or prior cortical or retinal TIA 7. Prior ipsilateral carotid endarterectomy 8. Impaired renal function: characterized by estimated GFR < 40 9. Intolerance or contraindications to aspirin or clopidogrel (including thrombocytopenia, prolonged INR) 10. A score < 24 (adjusted for age and education; adapted from Crum et al, 1993; n = 18,056) on the Folstein Mini Mental Status Examination 11. Medical contraindication to MRI 12. Pregnancy or women of child-bearing potential who are not following an effective method of contraception 13. Geographic or social factors making study participation impractical 14. Unable or unwilling to provide informed consent 15. Unlikely to be compliant with therapy / unwilling to return for frequent clinic visits 16. Concurrent participation in another study with an investigational drug or device 17. Other likely specific cause of stroke (e.g. dissection, vasculitis, prothrombotic diathesis, drug abuse)