Year 2 report - MVM MBChB Curriculum Executive Home Page
advertisement
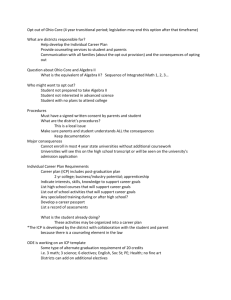
Page 1 of 5 PAPER 14/PC/01 MBChB YEAR 2 REPORT – 2013/2014 Dr I Johannessen (on behalf of the MBChB Year 2 Committee) 0/ GOVERNANCE Year 2 is governed by the MBChB Year 2 (Y2) Committee which sits thrice per academic year and reports to the MBChB Programme Committee (PC). Membership includes the Year Director (Dr I Johannessen), Deputy Year Director (Dr E Duvall) and Course/Module Organisers (CO/MO; see 1 below) together with Student and Pastoral Care representatives as well as key administrative staff. Mrs C Johnston is the Year’s Co-ordinator. In line with learning outcomes and overall curriculum, individual components are led by academic staff (see 1 below), and the Year works closely with the Centre for Medical Education (CME; Pr H Cameron) on research and development. Dr W Wallace is Chair of the Year’s Board of Examiners (BoE), and Dr N McCormick is the Assessment Officer. External Examiners are Dr A Stanley (Gastroenterology, U of Glasgow; Mol to Soc 2a), Pr GR Williams (Endocrinology, Imperial College London; Mol to Soc 2b) and Pr CM Jackson (Primary Care Medicine, U of St Andrews; ICP). Pr Williams’ term finishes at the end of the current academic year, and Year 2 has identified a possible successor within the UK renal medicine community in liaison with Pr N Turner (RIE Renal Medicine) but confirmation is pending. Y2 endeavours to ensure Student representation in all its bodies/groups. Y2 comprises of 4 interwoven courses: Molecules to Society (Mol to Soc) 2a and 2b in Semester 1 and 2 (S1-2), respectively; Introduction to Clinical Practice (ICP; CO: Dr D Thomson); Student Selected Components (SSC; CO: Dr S Riley). The Mol to Soc 2a and 2b courses are generally considered together with the Year Director as CO - but authority delegated to the MOs. Dr Thomson’s term as CO for ICP finishes at the end of the current academic year, and Dr H Young will take over at the beginning of the next academic year. 1/ INTRODUCTION The aim of Y2 is to continue (from Y1) to embed fundamental scientific knowledge relevant to subsequent medical teaching and future clinical practice whilst also introducing the students to key clinical skills. In terms of content, Mol to Soc 2a includes Neurosciences (MO: Dr C Smith), Gastrointestinal/ Liver (MO: Pr J Plevris) and Epidemiology/ Statistics (MO: Pr I Rudan) whereas Mol to Soc 2b includes Renal/Urology (MO: Pr J Davies), Endocrine (MO: Dr S Morley), Clinical Genetics (MO: Dr W Lam) and Virtual Clinic (MO: Dr E Duvall). ICP is centred on student placements in General Practice (GP) surgeries with additional input from Emergency Care, Clinical and Resuscitation Skills (ECCARS; Dr J Skinner). SSC2a (Dr S Riley to be succeeded by Dr C Harlow) and SSC2b (Dr R Mayes) take place in S1 and S2, respectively. Problem-based learning (PBL; Dr F Pender) is woven into the fabric of both semesters in a manner that facilitates translation of individual components into a meaningful clinical context. Similarly, the Virtual Clinic aims to summarise fundamental scientific material covered UoE MBChB Year 2 Annual Report 2013/2014 Page 2 of 5 during Y1-2 with a view to explain its clinical significance. Anatomy teaching (Dr F Kristmundsdóttir) is integral to the course. 2/ STRUCTURE OF ACADEMIC YEAR The Year consists of 30 weeks and is comprised of the following components: Semester 1: Wk 1-6: Neurosciences (6 weeks) Wk 7-12: Gastrointestinal/Liver (6 weeks) Wk 1-11: SSC2a and Epidemiology/Statistics (sessions over 11 weeks) Wk 13-14: Examinations (Mol to Soc 2a OSCA/Practical) Semester 2: Wk 1-2: Clinical Genetics (2 weeks) Wk 3-5: Renal/Urology (3 weeks) Wk 6-11: Endocrine (6 weeks) Wk 12-15: Virtual Clinic (5 weeks) Wk 1-11: SSC2b (sessions over 11 weeks) Wk 16-17: Examinations (Mol to Soc 2b OSCA/Practical; ICP OSCE/OSCA) Across Semester 1 and 2: ICP (weekly sessions at GP Surgeries) PBL (twice weekly sessions) ECCARS (see 6.ii below) 3/ STUDENT NUMBERS & RELATED ISSUES In 2013/14, 195 students joined Year 2 compared to 247 and 234 in 2011/2012 and 2012/13, respectively. On average, 3 direct graduate (direct) entrants joined Year 2 in each of these academic years (in 2013/14, 1 was dental and 2 were MedSci students). 4/ QUALITY OF TEACHING - External Quality Assurance Y2 ensures external quality assurance of the Year’s teaching through close collaboration with the Clinical Educator Programme and close monitoring of student feedback received from the Year’s student body. Y2 expects all its academic staff to have completed relevant Clinical Educator courses by end of August 2016 as guided by, and in liaison with, Dr D Aitken (CME) with administrative UoE MBChB Year 2 Annual Report 2013/2014 Page 3 of 5 assistance from Mrs E Fairchild (CME) and Mrs C Johnston (Year 2). A summary of student feedback is included in Appendix 1 (Mr K Wylde). 5/ QUALITY OF STUDENT PERFORMANCE - External Quality Assurance Y2 ensures external quality assurance of the Year’s assessments through close collaboration with the Year’s External Examiners. Furthermore, students are introduced to Peerwise (led by Dr S Morley and Pr H Cameron) at the outset of Y2 with a view to support their learning through question writing. Equally, the approach aids student revision closer to exams in concert with formative exams. A summary of student marks/grades is included in Appendix 2 (Dr N McCormick). 6/ ASSESSMENT - Formative Exams Formative OSCA exams are offered in both S1 and 2 of Y2. They take the shape of one 2hrs-long standard-set OSCA exam representing the breadth and depth of the particular semester that is offered on-line over a long weekend 3 weeks prior to the exam diet itself. Feedback is offered online for a period of time. The exam ‘pitch’ ensures appropriate insight into the Year’s expectations. - Mol to Soc 2 Combined OSCA/Practical An independent pass in each of the Mol to Soc 2 OSCA (90%)/Anatomy Practical (10%) examinations is required (December and May; each OSCA comprises of two 2hrs-long papers referred to as Paper 1 and 2). Examination marks are weighted 40:60 for Semesters 1 and 2, and there is no compensation between semesters. Both S1 and 2 OSCAs contain elements of Y1, and S2 Y2 OSCA also contains an element of the preceding S1. In-Course Assignment (ICA) reports Pass is required for an ICA in each of both semesters. SSC An independent pass is required for each of SSC 2a and SSC 2b (see also peer feedback below). Peer feedback Students are required to submit and pass each of four electronic peer feedbacks (two for PBL - one in S1 and one in S2 – and one for each of SSC 2a and SSC 2b). Professional Development Portfolio (PDP) Students are required to maintain their PDP throughout the year and submit/upload CV and completed Generic Professional Skills form on time. UoE MBChB Year 2 Annual Report 2013/2014 Page 4 of 5 e-Calc In principle, students are required to participate in all e-Calc tasks, but they were not offered in a systematic manner in Y2 in 2013/14 since their role is under review across the curriculum. - ICP Combined OSCE/OSCA examination Students are required to pass the ICP OSCE/OSCA examination independently of the other components of the course (May; OSCA comprises of one 1hr-long paper). Patient Study Clinical Reports Students are required to complete two such reports but do not formally have to pass these independently. However, marks for each report contribute to ICP. ECCARS Students are required to attend all skills sessions and perform the tasks satisfactorily (S1: Airways management; Nutrition assessment; Venepuncture; S2: Breast examination; Blood glucose monitoring & Insulin administration; Urinalysis). Overall ICP Mark The components of the overall ICP mark are as follows: OSCE 40%, OSCA 35%, Patient Study Clinical Reports 20% (ie, two Reports worth 10% each) and ECCARS 5%. 7/ INNOVATIONS Modes of Teaching Delivery Y2 continued to trial a ‘Flipped Class Room’ approach (Drs Duvall and Johannessen) as well as live streaming from theatres (Mr S Paterson-Brown; organised in liaison with Mr K Wylde). Both were well received by students as a result of the manner in which topics were placed in a clinical context. Further considerations include offering lectures on-line and/or via mobile apps. Clinical Component Currently, the clinical component in Y2 is provided primarily by ICP, but novel teaching (outlined above) adds to this approach. Equally, the Year is considering further ways of increasing clinical exposure and Y2 has already embarked on discussions with NES (Dr S Edgar) and NHSL (Ms S BallardSmith) to introduce students to hospital medicine in a nurse-led manner with a view to trial such an approach as a pilot in S2 of the next academic year. Virtual Clinic Teaching sessions of the Virtual Clinic (VC) were consolidated in a manner that provides revision of a particular topic followed by discussions centred on clinical context with additional input from clinical colleagues in a manner that is appropriate for a particular session. Whilst the revised approach emphasised clinical context, it also enabled the Year to free up some time for student revision. UoE MBChB Year 2 Annual Report 2013/2014 Page 5 of 5 However, the Year also recognises that the VC requires further re-structuring and such discussions have begun already with a view to achieve better the module’s aim of consolidating learning in the appropriate clinical context. Remedial Teaching Y2 continues to offer its re-sit students a structured programme of remedial teaching for all its Mol to Soc 2a and 2b modules. Direct (Graduate) Entrants Y2 has voiced its concern at PC meetings regarding direct graduate entry into Y2 and recommended that graduate students enter into Y1. Attendance Attendance at all ICP and PBL sessions is compulsory. The Year awaits guidance from the PC regarding lecture attendance. 8/ PLAN FOR 2014/2015 Student feedback informs subsequent Y2 Committee meetings. Thus, feedback from S2 (and PBL) will be addressed in October 2014 alongside proposals for re-structuring of ICA and VC as well as proposals for nurse-led teaching. 9/ FUTURE CHALLENGES Intercalated Degree In light of the UoE MBChB becoming a 6-year programme as of 2016/17, Y1-2 will seek to explore opportunities in what is understood to be the current proposal with a view to prepare students for a new Y3 (the current intercalated year). However, neither Year expects major changes in their approach at this time. 10/ REPORT WRITING The Report was drafted by Dr I Johannessen and circulated to Y2 Committee Members for their comments that were then incorporated into the final version, which was submitted to Ms C Tomlinson (CMVM) on 10 August 2014. Thus, the Report represents the consensus views of Y2. 11/ APPENDICES 1/ Summary of feedback from students (Mr K Wylde) 2/ Summary of student performance (Dr N McCormick) UoE MBChB Year 2 Annual Report 2013/2014