Spark 4 Outline - Adolescent Health Initiative
advertisement
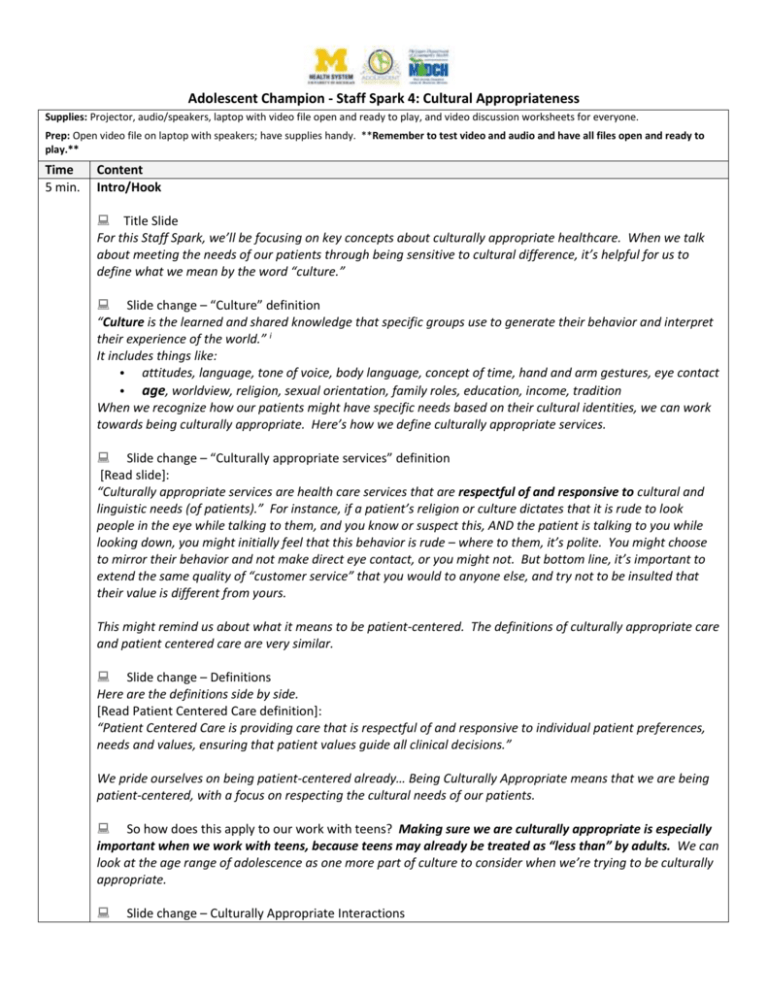
Adolescent Champion - Staff Spark 4: Cultural Appropriateness Supplies: Projector, audio/speakers, laptop with video file open and ready to play, and video discussion worksheets for everyone. Prep: Open video file on laptop with speakers; have supplies handy. **Remember to test video and audio and have all files open and ready to play.** Time 5 min. Content Intro/Hook Title Slide For this Staff Spark, we’ll be focusing on key concepts about culturally appropriate healthcare. When we talk about meeting the needs of our patients through being sensitive to cultural difference, it’s helpful for us to define what we mean by the word “culture.” Slide change – “Culture” definition “Culture is the learned and shared knowledge that specific groups use to generate their behavior and interpret their experience of the world.” i It includes things like: • attitudes, language, tone of voice, body language, concept of time, hand and arm gestures, eye contact • age, worldview, religion, sexual orientation, family roles, education, income, tradition When we recognize how our patients might have specific needs based on their cultural identities, we can work towards being culturally appropriate. Here’s how we define culturally appropriate services. Slide change – “Culturally appropriate services” definition [Read slide]: “Culturally appropriate services are health care services that are respectful of and responsive to cultural and linguistic needs (of patients).” For instance, if a patient’s religion or culture dictates that it is rude to look people in the eye while talking to them, and you know or suspect this, AND the patient is talking to you while looking down, you might initially feel that this behavior is rude – where to them, it’s polite. You might choose to mirror their behavior and not make direct eye contact, or you might not. But bottom line, it’s important to extend the same quality of “customer service” that you would to anyone else, and try not to be insulted that their value is different from yours. This might remind us about what it means to be patient-centered. The definitions of culturally appropriate care and patient centered care are very similar. Slide change – Definitions Here are the definitions side by side. [Read Patient Centered Care definition]: “Patient Centered Care is providing care that is respectful of and responsive to individual patient preferences, needs and values, ensuring that patient values guide all clinical decisions.” We pride ourselves on being patient-centered already… Being Culturally Appropriate means that we are being patient-centered, with a focus on respecting the cultural needs of our patients. So how does this apply to our work with teens? Making sure we are culturally appropriate is especially important when we work with teens, because teens may already be treated as “less than” by adults. We can look at the age range of adolescence as one more part of culture to consider when we’re trying to be culturally appropriate. Slide change – Culturally Appropriate Interactions Adolescent Champion - Staff Spark 4: Cultural Appropriateness This is much easier to understand when we think about concrete examples of how we can be culturally appropriate. For example - [Read slide] Slide change – Worksheet We’ll watch two video clips that show staff and providers interacting with a patient – in some cases, the providers and staff in the videos demonstrate culturally appropriate interactions, and in other cases, they show interactions that need improvement. [Hand out worksheet for video discussion. If you choose not to use the worksheet, suggest participants make mental notes about video observations.] There are two scenarios. While watching the video, use the worksheet to jot down your thoughts. The left column is for examples of culturally appropriate care – write examples of positive, culturally sensitive behaviors you notice. The right column is for examples that are not culturally sensitive, or that could be improved. Keep an eye out for two aspects of culture in particular (they might be easy to miss) – sexual orientation and religion. The teen male patient refers to his imam, and for those who may not know, an imam is a Muslim religious leader. 3 min. Show video clip. Slide has photos of Mariana and Sharif scenarios. Click link at bottom for video. [Use this link to play the YouTube video. https://www.youtube.com/watch?v=cytETc6FTJ0] Key Concepts Let’s discuss scenario #1 with Mariana (patient), the receptionist and Dr. Simon: 1. It’s pretty clear that the receptionist was rude, and being polite is basic common courtesy. But let’s look beyond that. What ways could the receptionist have improved her interaction with Mariana, especially as it relates to cultural appropriateness? [Have people share responses] Possible responses: apologizing for mispronouncing name, not announcing that patient is late, changing tone of voice, review clinic policies (late arrivals) with patient if needed 2. Also, Dr. Simon was short and dismissive with Mariana. But focusing on cultural appropriateness more, what could Dr. Simon have done differently or better in his interaction with Mariana? Possible responses: establish rapport with patient, not check his phone, asked the patient about sexual orientation/sexual activity (Mariana implied that she did not need condoms but was sexually active – this might mean she is in a relationship with a woman), better eye contact 3. Did you notice the “thumbs up” sign from Dr. Simon? Why may this not be appropriate? Nonverbal communication varies greatly among people and often leads to misunderstandings. For example, making direct eye contact is a sign of disrespect in some cultures. The thumbs-up gesture is commonly used in many cultures to signify a job well done. However, in Australia, Greece, or some cultures in the Middle East, it can have a rude meaning. Now let’s discuss scenario #2 with Sharif (patient) and Dr. Bell: 1. In what ways did Dr. Bell model culturally appropriate care with Sharif? Possible responses: assured him of confidentiality/privacy, established relationship with patient, commended patient for seeking care, acknowledged family and religious beliefs when Sharif said it was ©2015 Adolescent Champion - Staff Spark 4: Cultural Appropriateness important to his parents and imam for him not to have sex (an imam is a Muslim religious leader). 2. Is there anything Dr. Bell could have done differently or better in his interaction with Sharif? 1 min. If no one responds: This video clip is meant to be an example of how to be culturally appropriate, so… good for Dr. Bell. Application It can be a lot easier to notice when someone is culturally in-appropriate than when someone is culturally appropriate. The videos outline some of the ways to be culturally appropriate with patients, but thinking about the “platinum rule” can come in handy here. Slide Change – The Platinum Rule goes one step further than the Golden Rule, which says that we should treat others as we would want to be treated. The platinum rule includes cultural appropriateness when it says, “Treat others as they want to be treated.” You may want to be treated a certain way, but that doesn’t mean that all others want to be treated that exact way – especially when we think of the wide range of cultural values, and the values of our adolescent patients. If a patient does not feel comfortable shaking hands, or wants to call you “Mr” or “Mrs” instead of your first name, being culturally appropriate means we do our best to accommodate their value. If a teen is wearing headphones that are playing music you find offensive, it can be challenging to maintain politeness. 1 min. In the context of culturally appropriate care, this means that we need to be respectful of and responsive to our patients’ cultural needs. Sparkler To keep our theme of Cultural Appropriateness on our minds this month, instead of doing activities for Sparklers, we’ll suggest that each person give some thought throughout the month to the ways that you are culturally appropriate. Some things we might do without thinking about it, and some we might do intentionally, to be culturally respectful. Just being aware of these moments can help us improve our quality of care. We’ll post this reminder on the board to keep it on your radar. Next month, our Spark is on Adolescent Centered Care, which will look more closely at what we know about adolescent development, and think more specifically about ways we can be respectful of and responsive to their needs. i National Center for Cultural Competence, Georgetown University Child Development Center, 2007. ©2015