Chapter 35: Chest Trauma
advertisement

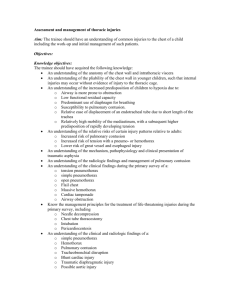
Chapter 35: Ready for Review The thorax contains the ribs, thoracic vertebrae, clavicle, scapula, sternum, heart, lungs, diaphragm, great vessels (including the aorta), esophagus, lymphatic channels, trachea, mainstem bronchi, and nerves. Oxygenation and ventilation (delivery of oxygen and removal of carbon dioxide) take place within the thorax, as well as some aspects of circulation. Injuries to the thorax can cause air or blood to enter the lungs, or may prevent the organs from being able to move properly, inhibiting oxygenation and ventilation. Begin the assessment of a thoracic trauma patient as you would any other patient—with a scene size-up and assessment of the ABCs. When you are assessing breathing, note any signs of injury to the thorax, which could indicate additional underlying injuries. Look for paradoxical motion, retractions, subcutaneous emphysema, impaled objects, or penetrating injuries. Consider the adequacy of ventilation and oxygenation. Watch for signs of hypoxia, an irregular pulse, changes in blood pressure, and jugular vein distention. Because the mechanism of injury that caused the thoracic problem may have been traumatic, always consider cervical spine stabilization in such cases. Several types of chest injuries may have similar signs and symptoms, such as hypoxia, pain, tachycardia, cyanosis, and shock. Managing the various chest injuries involves several common steps: maintaining the airway, ensuring oxygenation and ventilation, supporting circulatory status, and transporting quickly. Learning the subtle differences between various chest injuries will help you manage them more specifically. Chest wall injuries include flail chest, rib fractures, sternal fractures, and clavicle fractures. In flail chest, two or more ribs are broken in two or more places. It can result in a freefloating segment of rib that moves paradoxically when compared with the rest of the chest wall. As a result, the lung tissue beneath the flail segment is not adequately ventilated. Management of flail chest includes airway management and possibly positive-pressure ventilation, if the patient experiences respiratory failure. Intubation may also be necessary. Rib fractures produce significant pain and can prevent adequate ventilation. Sternal and clavicle fractures are also problematic because they are usually associated with other serious injuries. Management of rib fractures should focus on the ABCs and gentle splinting of the patient’s chest by having the patient hold a pillow or blanket against the area. Lung injuries include simple pneumothorax, open pneumothorax, tension pneumothorax, hemothorax, and pulmonary contusion. A pneumothorax occurs when air leaks into the space between the pleural surfaces from an opening in the chest or the surface of the lung. The lung collapses as air fills the pleural space. The result is a mismatch between ventilation and perfusion. Management of a pneumothorax begins with the ABCs and administration of highconcentration oxygen. Cover a sucking chest wound with a nonporous dressing. A tension pneumothorax is a life-threatening condition and results from collection of air in the pleural space. The air exerts increasing pressure on surrounding tissues as it accumulates, compromising ventilation, oxygenation, and circulation. Patients with a tension pneumothorax should be placed on high-flow supplemental oxygen via a nonrebreathing mask. Cover open wounds with a nonporous or occlusive dressing. If signs of tension are present, lift one corner of the dressing to allow air to escape. In the event of a closed tension pneumothorax, immediate relief of the elevated pressures must then be accomplished through a needle decompression. A hemothorax is the accumulation of blood between the parietal and visceral pleura. It results in compression of structures around the collection of blood and compromises ventilation, oxygenation, and circulation. If the airway of a patient with a hemothorax does not require intervention, place the patient on high-flow supplemental oxygen via a nonrebreathing mask. Initiate two largebore peripheral IVs, with fluid resuscitation being guided by local protocols and directed at limiting the duration of hypotension. A hemopneumothorax is the collection of both blood and air in the pleural space. A pulmonary contusion occurs from compression of the lung. It results in alveolar and capillary damage, edema, and hypoxia. For patients with a pulmonary contusion or cardiac tamponade, assess and manage the ABCs and consider administering IV fluids. Myocardial injuries include cardiac tamponade, myocardial contusion, myocardial rupture, and commotio cordis. Cardiac tamponade occurs when excessive fluid builds up in the pericardial sac around the heart. The heart becomes compressed and stroke volume is compromised. The treatment of the patient with cardiac tamponade begins by managing the ABCs, ensuring adequate oxygen delivery, and establishing IV access. Provide a rapid fluid bolus to maintain cardiac output. Pericardiocentesis is the ultimate treatment option for this condition, a risky technique that is rarely performed by paramedics. Myocardial contusion is essentially blunt trauma to the heart. Hemorrhage, edema, and cellular damage result, and dysrhythmias may occur. Management of patients with a myocardial contusion should be supportive, but also includes cardiac monitoring and establishing IV access. Fluid resuscitation should be instituted as needed to maintain the patient’s blood pressure. Consultation with online medical control may precede the administration of antidysrhythmic agents. Myocardial rupture is perforation of one or more elements of the anatomy of the heart, such as the ventricles, atria, or valves. It can occur from blunt or penetrating trauma. Patients with myocardial rupture should receive supportive care and be rapidly transported to a trauma center where a thoracotomy can be performed. Commotio cordis occurs from a direct blow to the chest during a critical portion of the heart’s repolarization period, resulting in possible cardiac arrest. ALS treatments for commotio cordis must follow standard ACLS guidelines for sudden cardiac arrest and treatments of the underlying rhythm must be initiated early if successful resuscitation is to occur. Vascular injuries include traumatic aortic disruption and great vessel injury. Traumatic aortic disruption is literally ripping of the aorta. Injuries to other great vessels may cause similar problems of potentially fatal bleeding. Care for patients with traumatic aortic disruption focuses on symptom control. After assessment and management of the ABCs, the patient should receive gradual IV hydration for the treatment of hypotension. Management of patients with great vessel injuries is no different from those with acute blood loss. Other thoracic injuries include diaphragmatic injuries (abdominal contents may herniate through the injury and cut off the blood supply); esophageal injuries, which can be rapidly fatal; tracheobronchial injuries (injury to the airways); and traumatic asphyxia (sudden compression of the chest leading to pressure on the head, neck, and kidneys, causing capillary beds to rupture).