SAINT ANTHONY EMERGENCY DEPARTMENT PHYSICIANS
advertisement

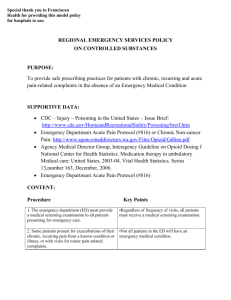
SAINT ANTHONY EMERGENCY DEPARTMENT PHYSICIANS ORIENTATION CHECKLIST The following checklist is to be used in the orientation of any new TeamHealth NorthWest physicians or mid-level providers working in the Emergency Department at Saint Anthony Hospital. The Medical Director/designee and the orienting physician should initial each item. All arriving physicians should receive the basic orientation package from TeamHealth prior to arrival. During the initial orientation the Medical Director will ask for and answer any questions generated by this package. Prior to Orientation Day: □ Log in to TeamHealth Institute Online https://thi.th-ext.com/portal/server.pt o Call 1-800-424-3672 x 2849 for access information M – F 9am – 5pm ET o View the Discharge Vital Signs Project o View the Patient Safety Fables o Complete the Mine Field Navigator for Emergency Medicine □ View the Franciscan Health System New Physician Orientation o https://www.fhshealth.org/physicians/newPhysOrientation.asp o Password: newdoc □ Obtain ID from Human Resources at St. Anthony’s and parking sticker from Security out by the ED Entrance. □ Arrange for Epic and Dragon dictation training: Contact AbigailPritchard@fhshealth.org □ Ask about having one of our physicians spend some time with you to set up your Epic smartphrases and Dragon orders before starting work. □ Give your phone number(s) to the ED Desks and Admin. Office o Please call the HUC station 253-530-2100 to give them your current cell phone and home numbers. o Email Tom Minter with the same info. tjminter@comcast.net Tour of the Emergency Department including: Patient entrances 119# / ambulance entrance (119*) Location and use of fire alarms, fire extinguishers and oxygen shut-off valves ED break room and physician’s office Mailboxes Lockers Treatment Areas: Intake rooms, Acute care rooms Location and use of emergency patient care equipment including: Defibrillators and Code Carts Intubation equipment Emergency drugs Difficult Airway Bag Ultrasound machine Cardiac monitors Oxygen supplies Suction equipment Central line equipment Cardiac pacing equipment Glidescope Nursing stations Introduction to nursing personnel, unit secretaries and ED techs Medications, location and prescribing in the ED Pyxis - No to go meds Charity Care Use the red ‘CHARITY CARE’ stamper as you see appropriate or ask pharmacist to facilitate. Pharmacies: The SAH Outpatient Pharmacy is now open in the Milgard Building from 9-5 M-F. In addition to filling employee prescriptions for the newly announced FHS Mail Order system the pharmacy can fill all discharge prescriptions during their hours of operation, including for patients requiring Prescription Assistance. The outpatient pharmacy can be reached at 130.2066 from inside the hospital. Walgreens – only 24 hour pharmacy in the area is in Tacoma. 15-20 minutes away. 4315 6th Ave, Tacoma, WA 98406 (253) 756-5159 Walgreens in Gig Hargbor open M-F 9-9p, Sat & Sunday 10-6p Target Pharmacy in Gig Harbor open M-Sat. 8-10, Sunday 8-9p EMS expectations Location and use of radio – o We are the Base Station for West Pierce County EMS. We handle calls from Gig Harbor and Key Peninsula EMS departments. Still receive calls from South Kitsap EMS, not as a Base Station, but as a receiving facility Prehospital Protocols, see Patient Care Protocol booklet and note Signal 1,2,3 and AMA info (page 7) Security Issues Suicidal or agitated patient; ask for a security 1 to 1; search and stand-by (Referred to as a Code 1) Code Gray– agitated person Code Red – Fire Code Yellow –Hospital-Only Trauma Code Blue- Cardiac/Respiratory Arrest Amber Alert – Infant/Child Abduction Rapid Response Team- Activate Rapid Response Team Code Silver- Weapon/Hostage Code 5 Shelter in Place o Code Triage – Disaster Response (Phase 1: Alert or Planning Phase 2: Activate) Registration staff/process Physician work stations (Max of 2 providers to the East or West stations to give nurses a place to work) Document time that patient was initially seen, this is used to calculate the Door to Doc time. This is performed by clicking the “Initial Provider Exam” button in Epic. Medical Decision Making – your best defense o Critical care time – unstable patient, lifesaving intervention see TeamHealth guidelines o Admission/Order sets: Transition, Rapid Rule out (Outpatient observation for Chest pain), Pneumonia, Sepsis, Procedural sedation, Transfusion and procedure consent forms, Code Neuro, tPA, Alcohol Withdrawal, Heparin, DKA, PCA, and Transfusion, Remember to document “Time outs” for procedures! Location and use of referral and on-call lists for local physicians Admission process After speaking with the admitting physician (usually Franciscan Inpatient Team) place an order for “ED to Hospital Bed request”. Place transition orders as soon as you have time or immediately if Charge Nurse asks you to write them. Med/Surg, Med-Tele, PCU, ICU, All new onset afib go to PCU All beds in hospital are Tele-capable Currently patients on NTG drips go to PCU Franciscan Inpatient Team (FIT) – unattached patients Group Health – (Marked as “G” on track board or personally informed by registration staff). Ask HUC to contact EPRO, (Emergency Patient Resources and Options). Present the case to the Group Health Triage physician for location of admission. Usually a transfer to St. Joseph Medical Center in Tacoma which is the Group Health base facility. Private MD’s who admit their own patients: Dr. Bill Roes and Dr. Mark Craddock. Call them first, they may request that FIT admit their patients but want to decide themselves. Mental Health – seek ED Social Worker assistance in disposition. Involuntary or Voluntary or any need of auxiliary Mental Health care – Call single point of Care: Optum Health Pierce RSN at 1-800-576-7764 Transfer of Care in Department to following provider Complete Transfer of Care form in Epic Do not hand off incomplete patients At end of shift, THIN SLICE: start work-up on new patients for oncoming provider, and document “Initial Provider Exam” time. Explain to patient concern for efficient evaluation/hand-off Transfer process to other facility With the exception of Trauma Transfers, Code Neuro Transfers, Pediatric & OB transfers you ask the HUC to contact the FPPC (Franciscan Patient Placement Center) where a trained nurse will discuss the case with you and then find an appropriate bed and contact an accepting physician and consultants. Complete transfer forms in Epic completely Send x-ray/CT copies if outside Franciscan System. (Trauma Team at Multicare does have same Diagnostic Imaging equipment so you don’t need to send copies for them. Transfer Risk includes worsening of specific disease process written on COBRA Form Discharge Vital Signs: Vital signs are taken within 30 minutes of discharge. If they are abnormal, the nurse will confront you with them. If you still wish to discharge a patient with abnormal vital signs (high risk!), you should add to your note why you are doing so. Discharge instructions Identify follow-up time and doctor Discuss reasons to return to ER Instruct what to do/not to do Medication counseling o (FMG clinic. You can arrange for a 1-2 day follow up even for no doc patients.) Franciscan Health Systems and TeamHealth Northwest have adopted the OXYFREE Emergency Department policy. Please read the Regional Emergency Services Policy on Controlled Substances which is added to the end of this document. It is a requirement for all providers to register for the Washington State Prescription Monitoring Program. This is a tool to improve patient care and work to assure patient safety by the review of a patient’s controlled substance dispensing records. https://wapmp-provreg.hidinc.com At the end of this Orientation document is a letter from the Department of Health detailing how to register. The Franciscan EDs are partners in the Statewide Emergency Department Information Exchange (EDIE). Which faxes an orange document that indicates that a patient has had more than 5 visits in a year and may include a care plan. Restraint process Do not write ‘restrain as necessary’ Chart reason and pre-restraint evaluation, date and time order Dictation now happens extremely rarely, but in the situation that Epic is nonfunctional, you could actually dictate. Dictation process 1-888-322-6104 or pick up dedicated dictation phone enter site code 7 + then hit pound key enter your MD dictation code (WA license #) + pound enter SAH facility code 5 + pound sign enter work type 340 (ER Report) enter 9-digit MRN number + pound dictate pt name + your name + MRN + date at the end of the dictation, hit "9" and write down the number that verifies your dictation on the chart 4 = pause 2 = resume 3 = rewind & listen 81 = rewind to beginning 7 = fast forward 63 = go to end and resume dictating 5 = begin new report Code 4 – In-House Code Materials Location and use of Code Blue Red Binder Complete reimbursement sheet Include patient face sheet or sticker Document a note in Epic. Tom Minter checks the Red Binder weekly and sends them in for coding. Radiology Location of x-rays and instructions for initial readings of x-rays by the ED physician X-ray discrepancy – radiology tech will present discrepancy notice dictate resolution cc: Tom Minter Radiology Reading Room at SAH 530-2162 (or in house 130- 2162) After 9 pm (Ford Building) Room 1 253-680-3586 Room 2 253-680-3584 Room 3 253-680-3585 NEP / FHS Expectations Professional Conduct Professional Attire Quality Medical Practice State and Federal Law Compliance MD/PA Resource Book Risk-adverse Medical Practice o Hand-off: and sign out. o MLP Supervision o Cardiac Equivalents o Missed FB o Poor Documentation Patient Satisfaction the 5 S’s of Satisfaction. o Smile: be nice. People appreciate this more than anything. o Say: your name, the members of your team, the patient’s name, that you are concerned, that you have time, that we are all one team with the pts best interest at heart. Sit is also important but many of us interact in the ED while standing, and moving around, so I did not include it. o Solicit: ask for input from pt and family. Ask their expectations. It’s hard to meet expectations if you don’t know them. And if you meet them they will be satisfied. o Summarize: make sure they know what you think, what’s going on, and what’s the plan. o Satisfy: ask if there is anything else you can do to make their visit satisfactory and meet their expectations. Knowing this is a priority with you is deeply satisfying. Patient Interactions o Introduction: greet, introduce, sit, listen, establish expectations. o Initial Scripting Any more information we haven’t covered What I think is going on What I think we need to do to evaluate/treat you o How long I think it will take Can I get you something for pain right now (or anything else) Do you have any questions o “Do the Show” o Updates on Progress o Final Scripting What’s wrong with you What we’re doing about it Who to follow-up with and when. What to do if I get worse o Discharge Instructions o Referrals General Specific o Introduction to ED Quality Assurance program Complaint Resolution/Chart reviews/Peer Reviews Patient Advocate Resolution process Dr.Tom Minter tjminter@comcast.net Office: 253-530-2133 cell phone: 253-948-2048 ThomasMinter@fhshealth.org Vocera system: To call from outside the hospital on a cell or landline to person at hospital currently using Vocera: 253-426-6991 Before beginning your first shift, you will need to: 1.Be signed up for Vocera 2.Have Epic and PACS access. 3.Completed AIDET training (watch a video and complete simple test obtain from Tom M) 4.Completed NIHSS training and certification ( the following is the free web site) http://nihss-english.trainingcampus.net/uas/modules/trees/windex.aspx 5.Be a registered Practitioner of the Washington State Prescription Monitoring Program SJMC EMERGENCY DEPARTMENT PHYSICIANS ORIENTATION CHECKLIST PHYSICIAN/MLP BEING ORIENTED (signature) Date___________ MEDICAL DIRECTOR/DESIGNEE (signature) Date___________ When complete, please sign and return to: 505 South 336th Street, Suite 600 Federal Way, WA 98003 Regional Emergency Services Policy on Controlled Substances PURPOSE: To provide safe prescribing practices for patients with chronic, recurring and minor pain-related complaints in the absence of an Emergency Medical Condition SUPPORTIVE DATA: ● CDC – Injury – Poisoning in the United States – Issue Brief: http://www.cdc.gov/HomeandRecreationalSafety/Poisoning/breif.htm ● Agency Medical Director Group, Interagency Guideline on Opioid Dosing for Chronic Non-cancer Pain: http://www.agencymeddirectors.wa.gov/Files/Opioid/Gdline.pdf National Center for Health Statistics. Medication therapy in ambulatory Medical care: United States, 2003-04. Vital Health Statistics. Series 13, number 163, December, 2006. ● Emergency Department Acute Pain Protocol (#816) ● CONTENT PROCEDURE 1. 2. 3. The emergency department (ED) must provide a medical screening examination to all patients presenting for emergency care. Some patients presents for exacerbations of their chronic, recurring pain from a known condition or illness, or with visits for minor painrelated complaints. Patients with any painful condition may request treatment with narcotic medications, but treatment with narcotic medication is not always the best medical care. KEY POINTS ▪Regardless of frequency of visits, all patients must receive a medical screening examination. ▪Not all patients in the ED will have an emergency medical condition ▪Treatment of chronic pain outside of a Primary Care Provider (PCP), or treatment of minor complaints with narcotic pain medications, puts patients at risk for accidental overdose, diversion, morbidity and mortality ▪The lowest potency medication should generally be prescribed to reduce the side effects and morbidity associated with these medications ▪For the above reasons 4. The treatment of pain will be guided by the provider’s judgment. 5. Narcotic medications should not be used for the treatment of minor pain-related complaints. 6. If chronic pain is to be treated in the ED, the use of oral analgesic is preferred over IV/IM administration. ▪Oral analgesics provide a more level, less dangerous treatment option 7. If the ED provider deems treatment of a chronic or minor condition necessary with controlled substances, no more than 5 pills will be given and not more often than every 30 days. ▪This is an exception to the rule and should ideally be coordinated with the patient’s PCP or pain specialist 8. The following medications will generally not be prescribed from the ED: Oxycontin, MS Contin, Dilaudid, Methadone, Fentanyl, Soma, Oxymorphone, or other long acting Opioids, except for compelling circumstances to be specifically documented by the provider on why they are necessary beyond the standard choices. 9. Oxycodone (Percocet, Roxicet, etc.) will be provided only in the presence of an objective source of new pain, documented on examination or by diagnostic testing. 10. If a provider feels that IV analgesic is indicated for treatment, generally no more than three weight based doses will be provided. ▪If the patient does not have a PCP the ED will provide a list of community primary care providers to the patient ▪These medications are for use in long term pain management and not appropriate out of the ED ▪They have a high rate of abuse ▪Oxycodone is associated with significant abuse and risk of morbidity and mortality ▪Use of higher doses of IV analgesia in the acute setting may result in patient harm in opiate naïve patients. In those with chronic pain, IV medications should be used only if PO medication is felt to be inadequate or contra-indicated ▪Refer to Emergency Department Acute Pain Protocol (#816) Franciscan Health Systems Emergency Department Chronic, Recurring and Minor Pain Control Policy The Franciscan Health System, in coordination with our Emergency Medicine Physicians, has developed an Emergency Department policy to govern the utilization of pain medications for the treatment of chronic, recurring and minor pain conditions. The State of Washington has seen a 400% increase in the death rate associated with prescription pain medications. Accidental overdoses are due to prescription drugs in 90% of cases. Emergency departments provide 39% of the prescriptions for controlled substances. As a result, this has become a public health issue and one we are working to address through this policy. Thank you for your assistance with this important issue and thank you for choosing Franciscan Health Systems. The goal of treatment of chronic, recurring and minor pain will be the use of oral medications. Oral medications have a longer course of action and provide a longer lasting relief of pain. In addition to oral medications, your emergency department provider may recommend ice/heat, relaxation, positioning or other measures which may provide relief. Treatment Guidelines While we strive to treat pain in an aggressive manner, it is important to remember that the decision on what medications to use is complicated and within each provider’s individual judgment. We generally encourage the use of oral pain medications given their longer duration of action, better safety, and safety in administration. In the rare instances where intravenous (IV) pain medication is needed, these will be limited to a few weight based doses with the plan for the conversion to oral medications as soon as possible. The following medicatons will not be prescribed in the emergency department: Oxycodone (Percocet, Roxicet) Oxycontin Fentanyl Dilaudid MS Contin Oxymorphone Methadone Soma Long acting opioids Chronic Pain It is important for your safety and good care that chronic pain issues be managed by a single care provider. This care provider should be your primary care provider or a pain management specialist. The emergency department cannot provide the appropriate level of monitoring and safety checks to manage chronic pain. As a result, we do not provide medication refills, replacement or supplementation of narcotic pain medications. Your providers will discuss medication options with you that will focus on non-controlled substances to help you get to your provider. Thank you again for choosing Franciscan Health Systems, we look forward to serving you now and in the future with all of your healthcare needs.