Anterior cruciate ligament reconstruction was brought to the public
advertisement

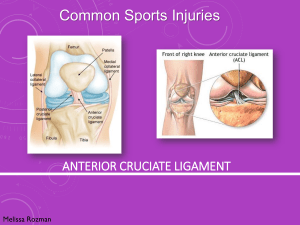
Anterior cruciate ligament reconstruction was brought to the public eye in January of 2013 when Robert Griffin III, a Rookie quarterback for the Washington Redskins, was injured during the NFL wild card game against the Seattle Seahawks. While he originally went in during surgery to reconstruct Griffin’s lateral collateral ligament, or LCL, the surgeon, Dr. James Andrews, also redid a previous reconstruction of the anterior cruciate ligament, or ACL, as well. Injury to the ACL is one of the most common problems seen by orthopedic doctors and surgeons in America; therefore, a lot of money and time is spent on researching the ACL more in depth. However, even with all this research done on the topic, which ACL reconstruction technique that is best for recovery of its patients is still greatly debated in the medical world. Reconstruction of the ACL can occur with an arthroscopic surgery, either with an allograft or autograft, as well as using mesenchymal stem cells. The ACL is a ligament in the human body that is located in the knee. Ligaments are fibrous connective tissues that connect two or more bones in the body. They are essential for joint stability and provide resistance of extensive motion of the joints. To understand the reconstruction of an ACL, one must first understand the anatomy of a knee. The knee is the largest joint in the human body and its forward motion is limited by the ACL. “Cruciate means “crossing”; therefore, the anterior and posterior cruciate ligaments “cross” each other to provide support and stability inside the knee joint. The ACL connects the femur bone to the tibia bone in the leg. Most ACL injuries are linked to stiff-leg standing, as well as quick twisting and turning movements of the knee. When an ACL is injured, a knee has more instability, is swollen, and could possibly have cartilage damage. The first noted mention of injury to the knee was Hippocrates of Cos, a ancient Greek physician, when he took notice of a subluxation of the knee. Although, he did not know of the ligaments in the knee, he was able to relate his observations to ligamentous-like injury. Aelius Galenus, a Roman surgeon and philosopher, later contributed to the Hippocratic understanding of pathology and medicine. Galenus was unable to dissect human cadavers due to Roman Law, but rather dissected animals to complete his studies. He was the first to describe the anatomy of the knee, as well as the first to name the ligaments, ‘ligamenta genu cruciate’ (Galen). The modern history of the diagnosis of an ACL tear dates back to 1845 when Amédée Bonnet wrote a formal dissertation on bloody effusions caused by joint issues. Bonnet was Professor of Surgery at Lyon University and was one of the first people to discuss the pivot-shift phenomenon of the knee, which eventually was used to test the instability of a knee. Later, he tested the use of a hinged knee brace as rehabilitation technique for knee instability. He analyzed an acute ACL rupture to have occurred by the consequential events. In his “Traite ́ des maladies des articulations”, Bonnet states that three signs that indicate an ACL rupture were “patients who have no suffered a fracture, a snapping noise, hemarthrosis, and loss of function are characteristic of ligamentous injury in the knee” (Bonnet, A.). The first surgeon known to reconstruct an ACL was MayoRobson of Leeds in 1895. Then, in 1917, Hey Groves of Bristol described an ACL reconstruction much like one of the techniques used today. His description was of an ACL reconstruction with autologous tissue graft, like the present day technique of autograft (Schindler OS.). According to the American Orthopedic Society of Sports Medicine, there are over 150,000 ACL injuries in the United States yearly. The society also stated that ACL injuries account for over half a billion dollars in healthcare costs (Hewitt), (Boden). There are currently two main types of reconstruction that use a human tendon to replace the patients’ ACL. A human cadaver’s tendon can be used, allograft, or the patient’s own tendon can be used, autograft, to replace the torn ligament. Stem cells can also be used to replace a ligament, despite the fact there is far less research and development of this technique than allografts and autografts. Although stability, strengthening, and plyometrics exercises are the best ways to prevent an ACL injury, it is still undetermined with type of reconstruction is best for a patient recovery, both short and long term. Autograft describes the surgical process that a tendon or ligament graft of oneself is used to replace their torn ACL. For an autograft ACL reconstruction, surgeons most commonly use the patient’s own patellar or hamstring tendon. The patellar tendon connects the patella (knee cap) to the tibia bone, or shinbone. An adult patellar tendon can range anywhere from 25 to 30 millimeters in width. To take the patellar tendon for the graft, the surgeon must take about one-third of the tendon (roughly 9-10 millimeters) from the center of the tendon to replace the ACL. Surgeons sometimes prefer using a patellar graft because it closely resembles the ACL in length. A patellar graft is “bone to bone” healing; therefore, it is heals quicker than a hamstring graft that must heal into place. When surgeons take part of the patellar tendon for the graft, they also must take part of the kneecap bone. This removal of bone has the possibility of causing anterior knee pain, as well as a fracture or rupture of the patellar tendon. The hamstring muscles are the group of muscles in the back of the thigh that are made up by the bicep femoris, semitendinosus and semimembranosus. The hamstring muscles’ main purposes are knee flexion and hip extension. During ACL surgery, the surgeon removes two tendons of these muscles and “bundle” them together to form a replacement ACL. Since the anterior portion of the knee is not disturbed with this type of graft, anterior knee pain is not usually an issue. The incisions are usually smaller for this type of graft. Pain from a hamstring graft usually occurs right after surgery and lessens as strength is regained in the leg. However a hamstring graft is not “bone to bone”, so patients with this type of graft must have a delayed start of rehabilitation with the graft heals into place. When surgeons go to take a hamstring graft, there is a chance of damaging the saphenous nerve branches during the process. It is possible that the patient could face problems with deep knee flexion, due to the weakened hamstring (Barrett). Allograft describes the process of using a human cadaver to harvest a graft to replace a patient’s torn ACL. For an allograft ACL reconstruction, surgeons most commonly use patellar tendon, hamstring tendon, and Achilles tendon from a cadaver. An advantage to using an allograft for a reconstruction is that there is harvest site morbidity from the donor site. There is also no pain or scars, as well, from the donor site for a graft in an allograft surgery because the graft is from a cadaver donor. Allografts, in general, have disadvantages caused by external factors. The cost of using a graft from a human cadaver is higher than harvesting an autograft. The availability of human cadavers also limits the use of harvesting grafts. Allografts also have a higher failure rate than autografts due to bacterial infection risk and delayed graft incorporation that both lead to an allograft failing to replace an ACL. Recent studies have tried to determine whether an autograft or allograft has a predominately better recovery than the other. However, a common result has emerged that neither type of graft show better results years after the surgery. Another downfall of conventional ACL reconstruction, whether it is allograft or autograft, is the requirement that patients’ must be skeletally mature before going in for the surgical reconstruction. Conventional adult ACL reconstruction could potentially cause a growth disturbance in the area of bone where cartilage grows, between the metaphysis and the epiphysis. This area, the growth plate, provides humans with longitudinal growth of bones. Conventional ACL reconstruction usually involves a surgeon drilling a tunnel in the bone through the area of the growth plates. If the tunnel is drilled in the bone before the growth plates naturally close themselves, the tunnel could cause the growth plates to close prematurely. These growth plates are responsible for the length of the femur and tibia bone. Therefore, trauma or iatrogenic damage to the physeal can lead a child to not grow properly due to unequal lengths of legs and angular deformity. Young children who are not skeletally mature are usually given the option to postpone their ACL reconstruction until the growth plates are closed. Patients with complete or partial ACL tears that must seek out nonreconstructive treatment are more likely to have issues with stability in the knee, as well as possible future damage to meniscal and articular cartilage (Kosher, MS., 2003). Although, patients will partial tears have a chance of the ligament naturally healing. Recent studies have shown that the instability of a knee due to a torn ACL in children that are not physiologically mature have worse consequences than stunting the growth in the leg by disturbance of the physeal (Kosher, MS., 2004). Mesenchamyl stem cells are adult, non-embryonic multipotent stem cells that are able to be differientated into different types of cells. Stem cells have made large advancements in ligament tissue engineering in the last decade. When an ACL of a knee ruptures, it limits the regenerative ability of the knee. Stem cells found in a human ACL are able to differentiate into chondrocytes, osteoblats, and adipocytes. Mesenchamyl stem cells can be used in surgery through in vitro or coating to try to regenerate the ligament. To use mesenchamyl stem cells for reconstructive ACL surgery, a harvest site in either a donor’s ACL or from the damaged ACL of the patient is set up to reproduce more stem cells. The mesenchamyl stem cells are then injected into the injury site of the ACL or used for coating of the allograft or autograft of the ACL reconstruction. Usually human growth factors are injected or coated with the stem cells for a ligament repair to help with the healing process. These growth factors include insulin like growth factor I (IGF-I), transforming growth factor (TGF), platelet derived growth factor (PDGF), growth vascular endothelial growth factor (VEGF), and epidermal growth factor (EGF). These growth factors help regulate cellular activities during the healing process of the graft, as well as ligament cell proliferation (Fan, H.). Human growth factors are major factors in the influence of the differentiation of mesenchymal stem cells into fibroblasts (CIR Campus Bio-Medico University). The Journal of Arthroscopic and Related Surgery published an article that used rabbits that underwent bilateral ACL constructions to test whether or not the coating of stem cells around a hamstring autograft would improve the quality and healing of the graft. The results from this study showed that the grafts coated with mesenchamyl stem cells formed an intervening zone of cartilage during the healing of the graft. This zone was in the area that usually produces collagen fibers and scar tissue, which hinder the recovery of an ACL reconstructive surgery. Instead of collagen fibers and scar tissues, the zone is made of cartilage that resembles the chondral enthesis of normal ACL insertions. These reconstructive ACLs performed better than the controls during the experiments when it came to testing of biomechanical aspects of the ligament (Arthroscopy). Because mesenchamyl stem cells are a more recent discovery as surgical treatment there are very little studies done to support or discourage the use of them. A study done by the Children’s Hospital of Pittsburgh showed that ACL – derived CD34(+) cells that were used during reconstruction surgery through in vitro were beneficial to the tendon-bone healing. The stem cells were able to increase the processes of angiogenesis and osteogeneis; which resulted in an increase in biomechanical strength. These cells were also proven to be better than other groups of cells in their cell proliferation and VEGF secretion capacities (Mifune, Y.). Although autograft and allograft ACL reconstructions are the more popular choice of grafts at this current time, stem cells could develop as a major treatment for ACL ruptures once more research can be conducted. While allografts and autografts show the same results years post operation, it is clear that a new treatment needs to be discovered that cuts down on the pain, as well as graft healing time, after a surgery. Once mesenchamyl stem cells have been more thoroughly developed, it is very possible that they could become the new solution to ACL tears and other ligament replacements that are more biochemically sufficient. Arthroscopy: The Journal of Arthroscopic and Related Surgery - November 2004 (Vol. 20, Issue 9, Pages 899-910, DOI: 10.1016/j.arthro.2004.06.035) Barrett G.R., Luber K, Replogle WH et al: Allograft anterior cruciate ligament reconstruction in the young, active patient: Tegner activity level and failure rate. Arthroscopy 2010 26(12):1593-1601. Epub 2010 Oct 16. Bonnet, A., Traite ́ des maladies des articulations [Treatise on joint diseases]. Baillie`re, Paris, 1845. Boden BP, Dean GS Feagin JA et al. Mechanisms of anterior cruciate ligament injury. Orthopedics. 200;23:573-578. Centro Integrato di Ricerca (CIR) Campus Bio-Medico University, Via Alvaro del Portillo, 21, 00128, Rome, Italy Fan H, Liu H, Wong EJ, Toh SL, Goh JC. In vivo study of anterior cruciate ligament regeneration using mesenchymal stem cells and silk scaffold. Biomaterials 2008; 29: 3324-37. Galen, On the usefulness of the parts of the body. Clin Orthop Relat Res, 2003(411): p. 4-12. Hewett TE, Lindenfeld TN, Riccobene JV et al. The effect of neuromuscular training on the incidence of knee injury in female athletes: A prospective study. American Journal of Sports Medicine. 1999;27:699-706. Kocher MS, Foreman ES, Micheli LJ. Laxity and functional outcome after arthroscopic reduction and internal fixation of displaced tibial spine fractures in children. Arthroscopy. 2003;19(10):1085-90. Kocher MS, Mandiga R, Klingele KE, Bley L, Micheli LJ. Anterior cruciate ligament injury versus tibial spine fracture in the skeletally immature knee: a comparison of skeletal maturation and notch width index. J Pediatr Orthop. 2004;24(2):185-188. Mifune, Y., Matsumoto, T., Ota, S., Nishimori, M., Usas, A., Kopf, S., & ... Huard, J. (2012). Therapeutic potential of anterior cruciate ligament-derived stem cells for anterior cruciate ligament reconstruction. Cell Transplantation, 21(8), 16511665. doi:10.3727/096368912X647234