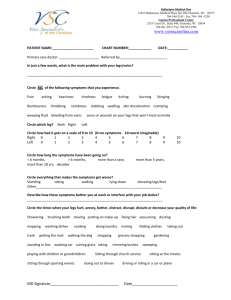
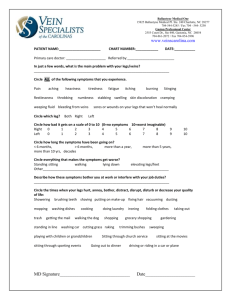
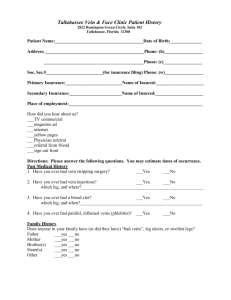
Confidential Health and History Form
advertisement

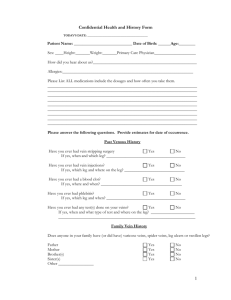
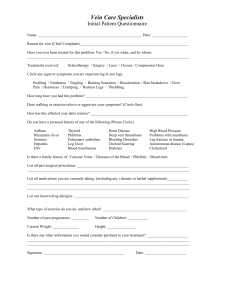
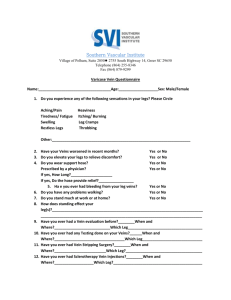
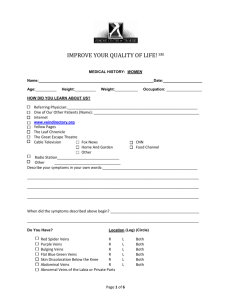
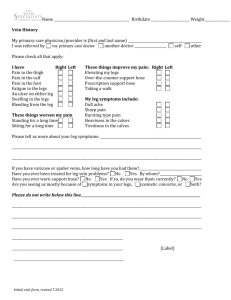
Confidential Physical Examination Date of Service: ________________________ Patient Name: __________________________ Date of Birth: ______________ Age: ________ Blood Pressure: R________ L________ HR________ RR________ Temp ________ SaO2________ General: Obese Thin Malnourished Healthy Head: Atraumatic Normocephalic Eyes: PERRLA EOM’s intact Sclera anicteric ENT: Pharynx clear Dentition good Neck: Supple No mass No JVD No bruit Thyroid /trachea midline Lungs/Chest: Symmetrical movement w/ breathing No wheeze No rub No rhonchi Heart: RRR Normal S1/S2 No murmur No rub or gallop ABD: Soft Nontender No mass No organomegaly Lower extremities: Edema Telangiectasias Bulging Varicosities Corona Phlebectasia Lipodermatosclerosis Ulceration Cellulitis PT pulse DP pulse Other ______________________ Measurements: Ankle circumference Calf circumference Thigh circumference Height Right Left Right ______ cm Right ______ cm Right ______ cm Calf ______ cm Thigh ______cm Both Left ______ cm Left ______ cm Left ______ cm Labs: ______________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ Diagnostic Test:______________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ Impression: _________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ Plan:_______________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ Physician Signature: ____________________________ 1 Confidential Health and History Form Today’s Date: __________________________ Phone: ________________________________ Patient Name: __________________________ Date of Birth: ______________ Age: ________ Sex: ____ Height: _____ Weight: _____ Primary Care Physician: ____________________________ How did you hear about us? __________________________________________________________ Please List ALL medications, include the dosage and how often you take them: Name the Drug Strength Frequency Taken Allergies to medications Name the Drug Reaction You Had Please answer the following questions. Provide estimates for date of occurrence. Past Venous History Have you ever had vein stripping surgery? Yes No If yes, when and which leg? ______________________________________________________________________________________________ Have you ever had vein injections? Yes No If yes, which leg and where on the leg? ____________________________________________________________________________________ Have you ever had a blood clot? Yes No If yes, where and when? ________________________________________________________________________________________________ Have you ever had phlebitis? Yes No If yes, which leg and when? ______________________________________________________________________________________________ Have you ever had any test(s) done on your veins? Yes No If yes, when and what type of test and where on the leg? ______________________________________________________________________ Family Vein History Does anyone in your family have (or did have) varicose veins, spider veins, leg ulcers or swollen legs? Father Yes No Mother Yes No Brother(s) Yes No Sister(s) Yes No Other ___________________________________ Yes No 2 Symptoms Do you experience any of the following in your legs? Aching / pain? Yes No Heaviness? Yes No Tiredness / fatigue? Yes No Itching / burning? Yes No Swollen ankles? Yes No Leg cramps? Yes No Restless legs? Yes No Throbbing? Yes No Other? _________________________________________________________________________________________________________ Have your veins gotten worse Yes No Yes No Describe: _____________________________________________________________________________________ Do you take any medication for pain or discomfort in your legs? ( i.e., Advil , Motrin) If yes, what medication do you take and how many times / mgs per day? __________________________________________________ Do you elevate your legs to relieve your leg discomfort? Yes No If yes, how long per day do you elevate and does it provide relief? ________________________________________________________ Does walking / exercise relieve your leg discomfort? Yes No Does walking / exercise make your leg discomfort worse? Yes No Do you exercise? Yes No If yes, what kind of exercise and how often? ____________________________________________________________________ Do you wear medical grade compression stockings? Yes No If yes, what type and gradient? __________________________________________________________ How long have you worn them? __________________________________________________________ If yes, what is the name of the physician who prescribed your compression stockings? ________________________________________ When were they prescribed? _______________________________________________________________________________________ Do you wear light support hose (i.e., Sheer Energy)? If yes, do they provide relief? Yes No Yes No What type of work do you do? _______________________________________________________________________________________________ How often do you stand (hours per day) at work? __________ at home? _________ Please be specific and describe how your symptoms are interfering with your activities of daily living: _________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ Past Medical History 3 Do you have a history of? Anemia Hypertension Atherosclerosis Kidney Disease Ankle skin changes Leg Ulcers Bleeding / blood disorder Liver disease Cancer Lupus Chest pain or discomfort Migraine headaches Crohn’s disease / IBS Myocardial Infarction Constipation Mitral Valve Prolapse Deep Vein Thrombosis / Clot Pulmonary Embolus Diabetes Rupture of a vein Easy bruising Superficial Thrombophlebitis Hepatitis Trauma to your legs HIV Other ______________________________________________________________________ Please list any surgeries or injuries you have had: __________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________ Family History Is there a history in your family of venous disease, deep vein thrombosis, stroke, clotting disorders or heart disease? Mother Father Grandparents Siblings Aunt / Uncle Child Social History Who do you live with? ____________________ What do you do for a living? ________________________________________________________________________________________________ Activity level? ______ Very active ______Some activity ______ Sedentary Do you smoke? ___ yes ___ no If yes, how much? ___________ For how long? __ If no, did you ever smoke? _____When did you quit? ______ Review of Symptoms Are you currently experiencing or recently experienced any of the following? Please mark yes or no. Cardiovascular: Yes Pulmonary: No Chest pain, pressure Tightness or heaviness in your chest Any of the above with exertion Irregular heart beat High cholesterol Shortness of breath Coughing up blood Asthma or tuberculosis Pneumonia or pleurisy Cough Patient Signature: _______________________________________________________________ Date: ____________________________________ 4