TOCC-PR-021 Anaphylaxis Policy
advertisement

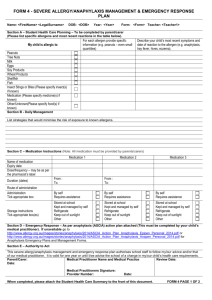
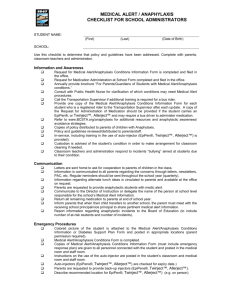
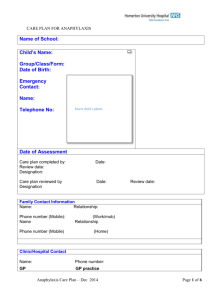
Document No: Approval Date: Approved By: TOCC–PR–021 07/11/2007 Children’s Services ANAPHYLAXIS POLICY Coordinator Review Date: 1/07/2012 Responsible Officer: Expiry Date: N/A Early Years Team Leader Version No: 4 Authorising Officer: Chief Executive Officer 1. Purpose To minimise the risk of an anaphylactic reaction occurring while the child is in the care of the Early Years service. To ensure that staff members respond appropriately to an anaphylactic reaction by initiating appropriate treatment, including competently administering an EpiPen® or Anapen®. To raise the service community’s awareness of anaphylaxis and its management through education and policy implementation. 2. Scope This policy applies when a child is diagnosed as being at risk of anaphylaxis, by a qualified medical practitioner and is enrolled at the Early Years service. It applies to children enrolled at the service, their parents/guardians, staff and licensee and other relevant members of the service community, such as volunteers and visiting specialists. Promote awareness that it is not possible to achieve a completely allergen-free environment in any service that is open to the general community: Staff should not have a false sense of security that an allergen has been eliminated from the environment. Instead the licensee recognises the need to adopt a range of procedures and risk minimisation strategies to reduce the risk of a child having an anaphylactic reaction, including strategies to minimise the presence of the allergen in the service. Legislation Children’s Services Act 1996 Children’s Services Regulations 2009 (Part 6) Health Act 1958 Health Records Act 2001 Occupational Health and Safety Act 2004 3. Definitions Allergen: a substance that can cause an allergic reaction. Allergy: an immune system response to something that the body has identified as an allergen. People genetically programmed to make an allergic response will make antibodies to particular allergens. Allergic reaction: a reaction to an allergen. Common signs and symptoms include one or more of the following: hives, tingling feeling around the mouth, abdominal Printed copies of this document are uncontrolled. The controlled version is available on the computer network at Page 1 of 6 pain, vomiting and/or diarrhoea, facial swelling, cough or wheeze, difficulty swallowing or breathing, loss of consciousness or collapse (child pale or floppy), or cessation of breathing. Anaphylaxis: a severe rapid and potentially fatal allergic reaction that involves the major body systems, particularly breathing or circulation systems. Anaphylaxis action plan: a medical management plan prepared and signed by a Doctor providing the child’s name and allergies, a photograph of the child and clear instructions on treating an anaphylactic episode including the prescribed anaphylaxis medication for that child. Anaphylaxis Management Training: comprehensive training provided by allergy nurse educators or other qualified professionals such as doctors or first aid trainers, which includes strategies for anaphylaxis management, recognition of allergic reactions, emergency treatment and practise with an EpiPen® and Anapen® trainer, and is reinforced at yearly intervals. EpiPen® a device containing a single dose of adrenaline, delivered via a springactivated needle, which is concealed until administered. Two strengths are available, an EpiPen® and an EpiPen Jr®, and are prescribed according to the child’s weight. The EpiPen Jr ® is recommended for a child weighing 10-20kg. An EpiPen® is recommended for use when a child is in excess of 20kg. Anapen® is a registered trademark for a commonly used auto injector of epinephrine (adrenaline),used to reverse anaphylactic shock. Anapens are commonly carried by persons with severe allergies and a risk of anaphylactic shock because they can be self-administered and are very fast-acting. Anapens are regulated medical devices and require a medical prescription in all countries. The Anapen contains a prefilled needle syringe combination which delivers adrenaline intramuscularly. EpiPen® and Anapen® Kit: an insulated container, for example an insulated lunch pack containing a current EpiPen® or Anapen® a copy of the child’s anaphylaxis action plan, and telephone contact details for the child’s parents/guardians, the doctor/medical service and the person to be notified in the event of a reaction if the parent/guardian cannot be contacted. If prescribed, an antihistamine may be included in the kit. Intolerance: often confused with allergy, intolerance is a reproducible reaction to a substance that is not due to the immune system. Risk Minimisation: a practice of reducing risks to a child at risk of anaphylaxis by removing, as far as is practicable, major sources of the allergen from the service and developing strategies to help reduce risk of anaphylactic reaction. Risk Minimisation Plan: a. a plan specific to the service that specifies each child’s allergies; b. the ways that each child at risk of anaphylaxis could be accidently exposed to the allergen while in care of the service; c. practical strategies to minimise those risks; d. who is responsible for implementing the strategies; e. if relevant to the child, practices and procedures regarding the safe handling, preparation, consumption and service of food, including but not limited to food sharing practices, hand washing and equipment cleaning; f. practice and procedures for ensuring that all parents or guardians of children being cared for or educated at the children’s service are notified of the known Printed copies of this document are uncontrolled. The controlled version is available on the computer network at Page 2 of 6 allergens that pose a risk to the child, the risks identified under paragraph (a) and the strategies for minimisation and management of those risks; g. practices and procedures to ensure that each staff member (including relief staff) , visiting early intervention staff member and volunteers can indentify the child and is familiar with – I. the child’s allergies; II. the child’s anaphylaxis medical management plan; III. the location of the child’s anaphylaxis medication and anaphylaxis medical management plan h. practices and procedures to ensure that the child does not attend the children’s service without the child’s anaphylaxis medication (if any) that has been prescribed by a registered medical practioner; i. the risk minimisation plan should be developed by families of children at risk of anaphylaxis and staff at the service and should be reviewed at least annually, but always upon enrolment or diagnosis of each child who is at risk of anaphylaxis. Communication Plan The communication plan must include practices and procedures to ensurea. that all staff members (including staff who are relief staff), visiting early childhood intervention staff members, volunteers and parents or guardians of children being cared for or educated by the children’s service are informed about anaphylaxis management in the children’s service and the anaphylaxis policy of the children’s service; b. that a parent or guardian of a child diagnosed as at risk of anaphylaxis who is being cared for or educated by the children’s service can communicate with the staff members at the children’s service caring for or educating the child, about any changes required to the risk minimisation plan and anaphylaxis medical management plan and how that communication can occur; c. that all staff members (including staff who are relief staff), visiting early childhood intervention staff members and volunteers are informed about and familiar with the child’s risk minimisation plan and anaphylaxis medical management plan 4. Procedures The licensee shall: conduct an assessment of the potential for accidental exposure to allergens while child/ren at risk of anaphylaxis are in the care of the service and develop a risk minimisation plan for the service in consultation with staff and the families of the child/ren. if applicable, a notice stating that a child who has been diagnosed as at risk of anaphylaxis is being cared for or educated at the children’s service. ensure all staff and parents of children with anaphylaxis are provided with a copy of the services anaphylaxis management policy. all staff (including relief staff) responsible for the child/ren at risk of anaphylaxis attend anaphylaxis management training, that is reinforced at yearly intervals. if it is not possible to find relief staff with the appropriate anaphylaxis management training, the child at risk of anaphylaxis is not permitted to attend the service. Printed copies of this document are uncontrolled. The controlled version is available on the computer network at Page 3 of 6 ensure that no child who has been prescribed an EpiPen® or Anapen® is permitted to attend the service or its programs without that EpiPen® or Anapen®. encourage ongoing communication between parents/guardians and staff regarding the current status of the child’s allergies, this policy and its implementation. display an ASCIA generic poster called Action plan for Anaphylaxis in a key location at the service. display an ambulance contact card by telephones. ensure health information to be kept in the child enrolment record contains details of anyI. special needs of the child; II. allergies, including whether the child has been diagnosed as at risk of anaphylaxis; III. other relevant medical conditions if the child is diagnosed as at risk of anaphylaxis, the current medical management plan for the child. It is a requirement that all staff working in Early Years attend Anaphylaxis Management training and adhere to the guidelines set out in this training. Anaphylaxis management training must include training in the followinga) nature of severe allergic conditions b) signs and symptoms and management of anaphylactic shock including administration of an adrenaline auto-injection device; c) risk minimisation and management strategies for allergic reactions and anaphylaxis appropriate for children Staff responsible for the child at risk of anaphylaxis shall: ensure a copy of the child’s anaphylaxis action plan is visible to all staff. follow the child’s anaphylaxis action plan in the event of an allergic reaction, which may progress to anaphylaxis. in the situation where a child who has not been diagnosed as allergic, but who appears to be having an anaphylactic reaction: - Call an ambulance immediately by dialling 0000. Commence first aid measures. Contact the parent/guardian. Contact the person to be notified in the event of illness if the parent/guardian cannot be contacted. practise EpiPen® and/or Anapen® administration procedures using an EpiPen® and Anapen® trainer and “anaphylaxis scenarios” on a regular basis and record the date each staff member undertook this training on the staff record form. ask all parents/guardians as part of the enrolment procedure, prior to their child’s attendance at the service, whether the child has allergies and Printed copies of this document are uncontrolled. The controlled version is available on the computer network at Page 4 of 6 document this information on the child’s enrolment record. If the child has allergies, ask the parents/guardians to provide a medical management plan signed by a Doctor. ensure that parents/guardians provide an anaphylaxis action plan signed by the child’s Doctor and a complete EpiPen® kit while the child is present at the service. ensure that the EpiPen® and/or Anapen® kit is stored in a location that is known to all staff, including relief staff; easily accessible to adults (not locked away); inaccessible to children; and away from direct sources of heat. ensure that the EpiPen® and/or Anapen® kit for each child at risk of anaphylaxis is carried by a trained adult on excursions that this child attends. regularly check the EpiPen® and Anapen® expiry date. (The manufacturer will only guarantee the effectiveness of the EpiPen® and AnaPen® to the end of the nominated expiry month.) provide information to the service community about resources and support for managing allergies and anaphylaxis. If medication is administered: a. the medication is administered from its original container bearing the original label and instructions and before the expiry or use by date; and b. if the medication has been prescribed for the child by a medical practitioner, the original container or original label bears the name of the child to whom medication is administered; and c. the dosage of the medication administered to the child is checked by a person other than the person administering the medication. Parents/guardians of a child at risk of anaphylaxis shall: inform staff, either on enrolment or on diagnosis, of their child’s allergies. provide staff with an anaphylaxis action plan and written consent to use the EpiPen® and/or Anapen® in line with this action plan. provide staff with a complete EpiPen® and/or Anapen® kit. regularly check the EpiPen® and Anapen® expiry date. assist staff by offering information and answering any questions regarding their child’s allergies. notify the staff of any changes to their child’s allergy status and provide a new anaphylaxis action plan in accordance with these changes. communicate all relevant information and concerns to staff, for example, any matter relating to the health of the child. Printed copies of this document are uncontrolled. The controlled version is available on the computer network at Page 5 of 6 7. comply with the service’s policy that no child who has been prescribed an EpiPen® or Anapen® is permitted to attend the service or its programs without that EpiPen or Anapen® Authorisation This policy was adopted by the Surf Coast Shire Early Years Service in August 2009. 8. Review date This policy shall be reviewed July 2011 Printed copies of this document are uncontrolled. The controlled version is available on the computer network at Page 6 of 6