Advisory A13/01 Notification of significant risk – 8 September 2015
advertisement

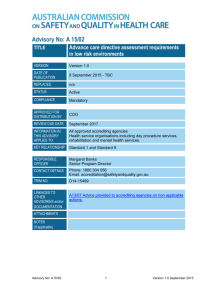
Advisory No: A13/01 (Amended) TITLE Notification of Significant Risk VERSION Version 3.0 DATE OF PUBLICATION 8 September 2015 REPLACES Version 2.0 issued 13 October 2013 STATUS Active COMPLIANCE Mandatory APPROVED FOR DISTRIBUTION BY COO REVIEW DUE DATE September 2017 INFORMATION IN THIS ADVISORY APPLIES TO: All approved accrediting agencies KEY RELATIONSHIP All NSQHS Standards RESPONSIBLE OFFICER Margaret Banks Senior Program Director CONTACT DETAILS Phone: 1800 304 056 Email: accreditation@safetyandquality.gov.au TRIM NO. D15-14936 LINKAGES TO OTHER ADVISORIES and/or DOCUMENTATION ATTACHMENTS NOTES (if applicable) Advisory No: A13/01 1) Significant Patient Risk – A paper and table outlining examples of major risks that result in significant harm to patients and may need to be reported Amended August 2015 1 Version 3.0 September 2015 Advisory No: A13/01 (Amended) Notification of Significant Risk PURPOSE: To describe the requirements for approved accrediting agencies to notify significant risks identified in health services to regulators and the Australian Commission on Safety and Quality in Health Care (the Commission). ISSUE: Accrediting agencies have sought clarification on the reporting of significant risks identified during an onsite assessment of a health service organisation. Approved accrediting agencies have signed agreements as part of the approvals process to liaise with health department contact officers. In particular, to notify regulators when a significant patient risk is identified during assessment of a health service. Ministers have tasked the Commission with the coordination of the Australian Health Services Safety and Quality Accreditation Scheme. This includes receiving information, including notification of significant risk. A definition of significant risk has been agreed and is at Attachment 1 and available on the Commission’s website at: http://www.safetyandquality.gov.au/publications/significant-patient-risk/ REQUIREMENTS: Approved accrediting agencies are to notify the regulator from the jurisdiction in which the health service organisation is located when a significant patient risk is identified during assessment. Notification should be made within 48 hours of a significant risk being identified and include an action plan developed by the health service organisation to mitigate the patient risk. The Commission also requires accrediting agencies to notifying the Commission when a significant patient risk is identified. Approved accrediting agencies are to inform their clients and include relevant clauses in any contractual arrangements that information on significant risk in the private sector will be provided to the regulators when it is required in regulation or policy of a government agency. Advisory No: A13/01 2 Version 3.0 September 2015 Attachment 1 (TRIM: 72918) Significant Patient Risk The Australian Health Services Safety and Quality Accreditation (AHSSQA) Scheme requires approved accrediting agencies to notify regulators if a significant risk of patient harm is identified during an onsite visit to a health service organisation. A significant risk is one where there is a high probability of a substantial and demonstrable adverse impact. In each case a significant risk will be sufficiently serious to warrant an immediate response to reduce the risks to patients. This may include interventions or changes to systems, clinical care or clinical practice. While the focus of reporting by surveyors will be on significant risks of patient harm, it will not necessarily exclude other significant risks. For each of the 10 NSQHS Standards examples of the risks that could be considered significant are detailed in Table 1 below. Few, if any Australian health service organisations pose an ongoing significant risk to patients, however from time to time, lapses and errors may occur that result in an increased risk to patients accessing care in that health service. Where a surveyor identifies one or more major risks in a health service organisation that could result in significant harm to patients the following actions are to be taken: 1. Surveyors are to notify both the health service organisation and their accrediting agency that a significant issue has been identified 2. Surveyors and / or an accrediting agency is to negotiate with the health service organisation a plan of action and timeframe to remedy the issues 3. An accrediting agency is to notify the relevant regulator that a significant issue has been identified and confirm the action being taken as soon as practical, usually within one working day. The following list provide examples only, it is not exhaustive and should not be used exclusively in identifying significant risks. Table 1: Examples of major risks that result in significant harm to patients and may need to be reported Standard 1: Governance for Safety and Quality in Health Service Organisation Risks Impact A process for credentialing staff does not Staff practicing outside of their exist and insufficient action is being taken competency and/or agreed scope of to address this issue. practice which leads to patient harm. Patient care records do not accurately Patients receive the wrong care, reflect care provided, notes are missing, inappropriate care, are misidentified or documentation is fragmented and no action care is not provided as directed or has been taken to address deficiencies in required. medical records Standard 2: Partnering with Consumers No significant risks of direct patient harm Advisory No: A13/01 3 Version 3.0 September 2015 Standard 3: Preventing & Controlling Healthcare Associated Infections Risks Impact Hand hygiene is not evident across the Preventable infections are transmitted to organisation patients. Single use invasive devices are being reused Multiple instances of aseptic technique is not being practiced in the health service Multiple instances of standard precautions and transmission based precautions are not being practiced in the health service Reusable medical devices are not decontaminated before reuse Standard 4: Medication Safety Risks A system to manage authorisations to prescribe, dispense and administer medications does not exist Patient medication histories are not taken or recorded in patients clinical records Adverse drug reactions are not recorded in patient clinical records or available at point of care Storage of medicines is unsafe or not secure. Impact Patients are given the wrong medication, do not receive the medication they require which leads to patient harm. Patients have adverse reactions to medicines which were preventable. Patient medicines can not be dispensed because they are not available, unsafe or ineffective resulting in harm. Standard 5: Patient Identification and Procedure Matching Risks Impact Lack of an organisation-wide system for Patients are misidentified and patient identification and procedure experience preventable harm. matching No evidence of action to address multiple near misses and/or incidents of mismatch between patients with their care Standard 6: Clinical Handover Risks Lack of a structured clinical handover system by the health service No evidence of action or the action taken is insufficient to address multiple clinical handover failures that have resulted in serious patient harm Advisory No: A13/01 Impact Patient information and/or accountability for care is not transferred and patients experience preventable harm. 4 Version 3.0 September 2015 Standard 7: Blood and Blood Products Risks No evidence of action or insufficient action to address risks of serious patient harm from the delivery of blood or blood products Major adverse events related to blood and blood products are not recorded, reported or analysed Use, storage, collection and transportation of blood and blood product is unsafe Impact Blood or blood products are not available for patients requiring care. Preventable harm occurs to patients receiving blood or blood products. Unnecessary wastage of blood products reduces patient access to product, delaying care and or resulting in harm from contamination. Standard 8:Prevention and Management of Pressure Injuries Risks Impact Failure to identify or monitor the risks of Patients develop preventable pressure developing a pressure injury by the health injuries. service Skin inspections are infrequent or not undertaken on ‘at risk’ patients Standard 9: Recognising and Responding to Clinical Deterioration in Acute Health Care Risks Impact No evidence of action or insufficient action Preventable patient harm occurs due to to address multiple instances of delayed or undetected or managed deterioration. failed escalation and/or response to clinical deterioration Multiple instances of the clinical workforce without basic life support skills No access to clinicians with advanced life support skills for deteriorating patients Standard 10: Preventing Falls and Harm from Falls Risks Impact Failure to identify or monitor patient falls Patients are at risk of being injured from and harm from falls by the health service a preventable fall. No evidence of action or insufficient action to address multiple instances of falls prevention plans that are not developed or not applied Advisory No: A13/01 5 Version 3.0 September 2015