Clinical-Interviewing-for-Herbal-Practitioners
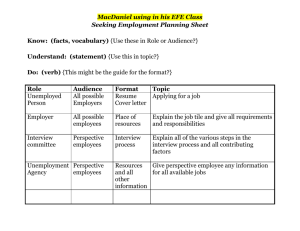
advertisement
Clinical Interviewing for Herbal Practitioners Student Questions about Client Interviewing & Evaluation: _ _ _ _ _ _ Seven Primary Goals of the Clinical Interview: 1. Understanding the nature of the primary complaint. o This is referring to understanding the primary complaint as a function of the balance, health, and vitality of the whole person (physically, emotionally, mentally, spiritually). 2. Determining the underlying imbalances relating to the primary complaint including their onset, history, and any related emotional trauma or stress. 3. Determining the primary sources of stress contributing to the underlying imbalances o (lifestyle, diet, sleep, environmental factors, emotionally stressful events or circumstances, work, family, social, relationships, finances, other health issues etc.) 4. Understanding any secondary complaints and how these may or may not relate to the primary complaint. 5. Determining any obstacles to life change - This refers to many factors, for instance: o Level of motivation for change, self-worth, lack of confidence in own ability to change and heal, emotional self-sabotage stories, past failures in taking care of health, fears related to family history, challenges with prioritizing health, loss of faith in possibility for health, high stress lifestyles, lack of support from family, loved one(s), work/boss (work culture of shaming self care), etc. 6. Defining Health Goals – Collaborative Regimen/Treatment Planning o Make sure to help client define positive ‘health goals’ rather than defining their goals in terms of the disappearance of their symptom (as is often done in conventional medicine). ie – “I would like an optimally functioning heart and cardiovascular system” vs. I want the heavy feeling in my arms, cold hands and feet, and my varicose veins to go away”. o We want to help the client expand their vision of what health could look like for them, not paint them into a box where the highest thing they can aspire to is the reduction of some specific symptom. 7. Developing the Protocol - Collaboratively developing a step by step herbal, food, and lifestyle protocol that helps the client to get moving in the direction of their defined health goals. o This protocol should address the client’s obstacles to life change and help the client take steps in the direction of health and wellbeing with regards to their overall health desires, their primary complaint, and general health. 1. Understanding the nature of the primary complaint In order to understand what is out of balance in the body we need to gather as much pertinent information as possible about the client’s subjective experience of their primary complaint along with the other holistic evaluation strategies. We may be using (visual observation, tongue, pulse, diet analysis, sleep analysis, energetic assessment, lab work, ) etc. The energetic and visual observation evaluation tools are crucial and invaluable. However, they are not enough, and ultimately what the client shares with us (their subjective experience) is the primary lens through which we can come to truly understand what is going on. After all, they are the ones the must engage with their life and body in a new way in order for their health to change. In order to get the information we need from a client it’s helpful to categorize their discomfort into qualitative categories. We want a rich and detailed understanding of someone’s discomfort and be able to relate it to the rest of the interpretation with have gathered from our evaluation of the client. The information we can get from a client’s self-report is arguably the most important piece of the pie, and also often the most difficult to get accurately represented. Example Interview questions to assess the client’s primary complaint OPQRST: (Paul Bergner’s Acronym) Onset (when did it start) Provoke/Palliate (what makes it better or worse) Quality (what qualities characterize the pain or discomfort) Referral/Radiating(does it radiate or refer to other areas) Severity (on a scale of 1-10 how severe is it: 10=unbearable) What level is it now? ___ Past month? ___Past two weeks?______ Timing (when, how long, how often does it occur, when did your first notice it, how long does it last). To get answers to these questions we don’t just go down the list and ask about onset and what provokes and palliates... We should gently weave these questions into the interview in a seamless way as we are encouraging the client to tell their story, as they are simultaneously feeling heard, seen, cared about, and validated in their experience. Not an easy task but you can all do it. Additional Questions – and you can add your own. These are just the basics 1. Location (where in or on the body is it located) – draw or point 2. Setting in which it occurs, environmental factors, activities, context, emotional setting or reactions, etc. 3. Associated symptoms or manifestations. Ask: “Is there anything else that seems to relate to it?” The Written Intake and getting ready for a consultation Client fills out written intake and returns to you a few days prior to the appointment. You research and evaluate all you can before the appointment and make notes in the margins about points you’d like more information about. You develop a working general hypothesis about what might be going on and review some categories of herbs you may want to think about if your hypothesis is correct. You write down other possibilities to rule out to see if your hypothesis seems correct. You get ready for your appointment using whatever centering, spiritual, contemplative practice you find works best for you. (explain heart focused breathing option) You may want to smudge the room you will be meeting with a client in, and/or take any herbs that help center you. You may also want to make a tea blend for your client. Interview Questions and Topics – and weaving the intake information into the Interview o Work in your intake questions into the history taking for each organ system in which the client indicated there was something going on. Consider how to phrase things in sensitive ways... o Examples: o “In addition to the constipation and bloating, you mentioned...(PMS with increased bloating and some other premenstrual symptoms)....”Let’s go over those in a little more detail...” – or substitute other questions you had from the intake. Emotional.... Quality of menstrual blood (color, clotting, heavy light etc..) Menstrual cycle – (regularity or lack thereof etc) Cramping – before, during, after, type of pain etc. (OPQRST if that is helpful) Musculoskeletal Mind ...(brain fog, sluggishness....or whatever) The first interview with a client: o At the beginning of the appointment you immediately begin the visual evaluation silently to yourself. o Start with client-appropriate small talk or light bantering (use your intuition and visual observation to get a sense for who this person is and make them feel comfortable) Stay attuned to what you experience in your own body. o Getting into the primary complaint conversation gently: (Our goal is for the client to feel safe and open to sharing the real story of what they are experiencing). Many practitioners recommend saying something like What brings you here today? But if you’ve already read the client’s intake, saying this can feel a bit awkward...since both the client and you know you already know the basics. Better would be saying something like. “You mentioned constipation and bloating as the primary reasons for your visit. Could we talk about that a little more right now?” And then... “can you tell me a little about when you first noticed it?” etc. If they don’t start talking after a few seconds or they don’t seem to know how to start you can help them out. “Would it be okay if I asked you some specific questions about that right now?” Saying something like “So, tell me about your uti, bacterial vaginosis, depression/constipation/hemorrhoids etc?” or something similar might be too abrupt and make them shut down a bit. Letting the Client Lead & Reflective Listening Supportive listening – nodding, saying things like ‘um-hmm’, and ...”and then what happened”, “okay”, “what was that like for you?” lets the client know you are being present and also encourages them to continue elaborating helpful information. Also practice leaning slightly forward with arms uncrossed, showing with body language you are staying connected. Most Importantly: Maintain moment-to-moment connection with client through disciplined attention. Keep working on not letting your thoughts drift off. Reflective Listening: Each time the client is done talking about their presenting complaint, you as the practitioner/herbalist reflects back to them a summary of what they have just said that includes the objective information they have shared as well as the emotional and experiential undertones the client may or may not have spelled out. Keep encouraging the client to continue exploring an answer until you can’t keep any more details in your mind. Then gently stop them and summarize for them to make sure you’ve understood everything up to that point. Example: (pay attention to how many facts and details you can remember at a time and don’t go beyond this before summarizing). 2-5 groupings of information is a good place to start. 1. “So, the constipation really seems like it got started when you were about 13 and that things were difficult at home while your parents got divorced and you were on antibiotics a lot because of strep throat and acne. 2. And if I remember correctly you were then constipated off and on in college but never really improved until it got a little bit better when you avoided gluten for a few months a couple of years ago. 3. Also, recently since you got back from travelling in India constipation has been really consistently difficult. 4. You’ve tried a lot of different approaches but recently it’s starting to feel more and more frustrating and even at times you’re starting to feel pretty discouraged (only if that’s really how they’re feeling)”. 5. Let me know if there was anything I missed.” 6. Is there anything more about that that seems like it could be related? o o Wait to hear client’s response. It’s important they feel completely understood, and that you didn’t miss anything significant. Listen for undertones... Short Encouraging Reflections: Reflective listening can also include shorter reflections of what they just said. This encourages the client to continue. o Client says: “My constipation is always bad in the morning when I’m running around trying to get ready for work”. –You might say...“So rushing seems to be making the constipation worse...”. Client says “yeah...definitely”. You might say “Anything else that seems to be making it worse?”.(they answer) ... and then “how about anything that seems to be making it better?” Here you are turning their story into an answer for O(P)QRST Each time your client finishes describing their concerns, ask is there anything else about that that could be related? Or...Is there anything else that seems important hat we haven’t talked about yet? Continue this as many times as it takes until your client can’t think of anything else that could be related. Reassure them there will be enough time to get to everything. Either this appointment or next time. Asking for clarification & getting the ‘Real’ subjective facts Often clients throw out terms describing their discomfort that they have been told by someone else, or a diagnosis they don’t understand. For instance: I’ve been feeling depressed, anxious, stressed out. Or I have stomach pain, acid reflux, diarrhea, or constipation. These answers seem pretty straightforward and self-explanatory, but you can have 10 clients with depression and diarrhea that all experience something very different. Ask for clarification “Can you tell me what you mean when you say ‘stomach pain’”? Could you point to where the pain is located? (Many people will point to their abdomen and not their stomach when they think they have stomach pain). “How do you feel when you are depressed, anxious, stressed out?” “What do you notice about yourself when you feel stressed out?” Empathy vs. Sympathy – What is the difference between sympathy and empathy? Sympathy: is the perception, understanding, and reaction to the distress or need of another human being. To express sympathy is to make it known that you are aware of another’s distress and that you have concern and care. Sympathy does not require the sharing of the same emotional state of another. Empathy: To express empathy takes things a step further by not only expressing awareness and concern or care but also showing a deeper level of understanding by entering into the other person’s experience. This is “understanding, being aware of, being sensitive to, and vicariously experiencing the feelings, thoughts, and experience of another of either the past or present”. We never suggest to clients how they should feel. Conveying excessive sympathy can feel to the client like you are feeling sorry for them and that we are telling them how they should feel. Maybe even that we’d judge them if they feel different than we suggest. Ex. Client says “My uncle died last week...”. If we say, “I’m so sorry, you must be feeling really sad”, then we are assuming what relationship they had with their uncle. It could have been a very complicated relationship. Instead it’s better to say something like “How are you doing with that?” Your goal is that they feel heard and understood at a deep level.... and to keep their story flowing. Your comments should be short and unbiased. To express you understanding comments like this can be helpful: “It feels like a lot of layers of emotion are involved in this. How does it feel to you when you think about it now?” “That was probably not an easy time for you” “You were in a lot of pain after that accident...”, ...they may start tearing up... “ it feels sad and painful to even think about it right now”,... “no one really got what you were going through at that time”,... “sounds like you may have felt kind of alone in that...” “doesn’t seem like you had the help you needed with...”, “It took a lot of courage to leave that relationship” Confrontation – be very careful with confrontation and use discernment. When we just talked about_________it seemed like some feelings were coming up for you. As you were talking about_________I noticed your shoulders tense up. Reflective Listening Exercise Use The Client Interview Form to guide the interview Talking about food, weight, and body image - choose language that makes the client feel comfortable and respected. Examples of questions: How to bring these kinds of topics up – with a lot of sensitivity... “You mentioned food cravings in the intake...is that something you want to talk about today?” “In the intake you mentioned weight gain since the birth of your daughter, is that something you want to address in our work together?” Or “is that something that feels related to the reason you came to see me?” “When we work holistically to support the body’s innate healing capacity, we often include diet and lifestyle recommendations specific to your constitution and specific needs. Is diet something you would be willing to explore today? What about lifestyle recommendations?” Talking about emotional trauma, grief, loss, etc. – Examples of questions: Have you experienced any particularly difficult time in your life that may relate to what we’ve been talking about today? You mentioned losing your father two years ago. Is that something you’d be willing to talk a bout a little right now. (if yes)...”How have you been doing with that? (not assuming it was good or bad or they feel sad etc) Would it be okay if we talked about your car accident a bit? Do you have any lingering injuries since the accident happened that are still bothering you? Was there any impact to your head? Were you hospitalized? Did it get evaluated? Tingling or numbness anywhere? Have you noticed any differences in how you feel day to day since your accident? Emotional variability or ups and downs? Any differences in memory or in how you process information? Anything else about the accident? Working with emotional/mental health issues “You listed depression, tearfulness, hopelessness, and panic attacks on your intake form. Would now be a good time to talk about that?” Explore all checked emotional symptoms (OPQRST) On a scale of 0-10 with 10 being the most hopeless you can imagine (or if they’ve mentioned something that sounds like suicidal ideation – with 10 being so hopeless you’re not sure if you want to continue living)...how have you been feeling the past couple of weeks? IMPORTANT – if they are experiencing ongoing depression or daily anxiety, or PTSD, or panic attacks, or severe mood swings, or HOPELESSNESS, or other unusual symptoms you’re not 100% sure about – they should be referred to a therapist and should ideally be in counseling while seeing you. Mental wellness issues need to be evaluated carefully – and just like giving someone a pharmaceutical med without ongoing counseling, giving someone herbs without the support they need can also be dangerous. PLEASE DONT give antidepressant herbs to someone reporting hopelessness or suicidal ideation or severe depression, or PTSD, delusions, or hallucinations, or other emotional/psychological/neurological issue you are not sure about without getting them established with a mental health therapist first. Challenges of working with mental health issues specifically unless you are experienced assessing for red flags and common mental health issues. For instance do you know if someone has dysthymia, major depressive disorder, bipolar disorder, PTSD, a phobia, an anxiety disorder. If you are unsure – consult Provide number to Multnomah county crisis line – if nothing else. If someone is actively suicidal – DO NOT let them leave your office without a safety plan. What is a safety plan? o o o o Assessing for mental health red flags - and need for referral to mental health provider. Getting the whole story Using your intuition Assessing energetic imbalances visual questions - from interview and intake tongue-Form pulse Exercise: Use the Interview form from yesterday to interview your client, taking into consideration the interviewing tools we just talked about. Start from the meeting and greeting in the beginning.