How to Suture
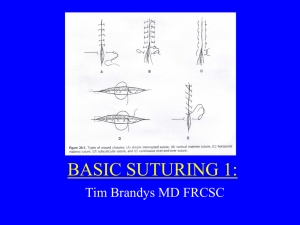
advertisement

How to suture General Principles: Avoid damaging the suture material while handing. Beware of the crushing of suture with surgical instruments. Using excessive tension while knot typing will cause the suture to break, and may even cause suture to tear through tissue. APPROXIMATE, DON’T STRANGULATE. o Sutures are intended to approximate tissues and should not be tied too tightly. Principles of knot tying: o The completed knot must be firm, and tied so that it will not slip. o The knot should be as small as possible to prevent tissue reaction or foreign body reaction (use small filament suture – aka thin suture) o While tying knots, avoid friction between the two strands, as this weakens the suture. o After the first loop of the knot is tied, you must maintain traction on one end to avoid loosening of the throw. o Tension on the knots should be horizontal and in the direction of the wound. o You can change position to place a knot securely and flat. o Extra ties do not strengthen the knot; they only add to the bulk. Loading the needleholder Always load the suture needle at a 90 degree angle to the needleholder. You should grasp the needle about 2/3 from the point (as shown) Always grasp the needle in the very tip of the needleholder. Types of suture Materials o There are a variety of suture types from which to select. Types are listed in the chart below. Suture Types Raw Material Tensile Strength Absorption Rate Contraindications Uses Determined by individual tissue characteristics 75% remains at 2 weeks; 50% at 3 weeks 55% remains at 1 week; 25% at 2 weeks Absorbed by proteolytic enzymes Not used for extended approximation of tissues under stress Soft tissue Absorbed by hydrolysis; complete by 5070 days Absorbed by hydrolysis; complete by 91119 days Not used for extended approximation of tissues Soft tissue Not used for extended approximation of tissues or for wound support >7 days Superficial soft tissue approximation of skin and mucosa only 70% remains at 2 weeks; 50% at 4 weeks; 25% at 6 weeks Absorbed by hydrolysis; minimal until 90 days and completely resorbed by 6 months Not used for extended approximation of tissues under stress Progressive degradation may result in gradual loss over time Indefinite Gradual encapsulation by fibrous connective tissue Nonabsorbable Patient allergy or sensitivity Soft tissues Sternal closure Progressive hydrolysis may result in gradual loss over time No degradation Gradual encapsulation by fibrous connective tissue Nonabsorbable Patient allergy or sensitivity Should not be used for permanent tensile strength None Soft tissue Absorbable Suture Surgical “Cat” Gut Plain or chromic Collagen derived from beef/sheep Vicryl Braided or monofilament Copolymer of lactide and glycolide Monocryl Monofilament Copolymer of glycolide and epsiloncaprolactone PDS II Monofilament Polyester polymer Nonabsorbable Suture Silk Braided Organic protein, fibroin Stainless steel Nylon Monofilament Stainless steel Long-chain aliphatic polymer Prolene Monofilament Monofilament or braided Stereoisomer of polyprolene Soft tissue Choosing the Suture: o Certain circumstances dictate which suture material is most appropriate. The following guidelines are useful: In a wound with maximal strength, sutures are no longer needed: Tissues healing slowly like skin, fascia and tendons should be closed with nonabsorbable sutures. Tissues that heal rapidly like stomach, colon, and bladder may be closed with absorbable sutures. Foreign bodies or potentially contaminated tissues may convert contamination to infection: Avoid multifilament sutures, which may increase risk of infection. Use monofilament or absorbable sutures in potentially contaminated tissues. When cosmetic results are important, close and prolonged apposition of wounds and avoiding irritants will produce the best results, thus: Use the smallest monofilament suture possible, such as nylon or polypropylene. Avoid skin sutures and close subcuticularly when possible. To secure close apposition of skin edges, a topical skin adhesive or skin closure tape may be used. Foreign bodies in the presence of fluids containing high concentrations of crystalloids may act as a nidus for stone formation. In the urinary and biliary tract, use rapidly absorbable sutures. Suture size o Ranges from 11-0 (smallest) to 6 (largest). Size 5-0 (“five-oh”) is best though of as 0.000001, and is smaller than 5. Smaller suture is used for more delicate tissue: Eye, blood vessels, skin of face, etc. Larger suture is used for structures with more tension: Bowel, muscle, fascia, tendon, joints, etc. Needle type o Taper (round) – used for soft tissue o Cutting (triangular) – used for skin. Simple Interrupted Load your suture on the needleholders. Take a “bite” ~1 cm from wound edge on both sides. (sometimes it helps to take this “bite” in two steps, reloading the suture from the center of the wound before the second “bite”) Tie knots (instrument or hand) to approximate tissues. Keep knots lateral to wound. Cut suture with ~2-3cm tails. Repeat to close wound, leaving ~1-1.5 cm between sutures. Simple Continuous Load the suture on needleholder. Take a “bite” identical to the simple interrupted suture. Tie the knot, but do NOT cut the suture. Instead of cutting the suture, continue taking evenlyspaced (~1 cm apart) bites of skin until you reach the end of the wound. To tie the simple continuous, leave a “loop” of suture on the final bite (do not pull the suture all the way to the skin). Then, use the loop as your tail and instrument or hand-tie the knots. Cut the suture with ~2 cm tails. Horizontal Mattress Load the suture on the needleholder. Take a “bite” like a simple interrupted (maybe a little larger; bigger bites are stronger). Instead of tying a knot, travel ~0.5 cm and make another “bite” towards your suture tail. Tie a knot using the two ends on the same side of the wound. Repeat with sutures ~1-2 cm apart until the wound closure is sufficient. **This particular suture type helps relieve wound tension. Vertical Mattress Load the suture on the needleholder. Take a large bite across the wound (at least 1.5 cm from the wound edge). On the same side as the suture exited, take small bites (0.5 cm) on both sides of the wound, finishing with the suture near your tail. Tie the suture , with the knot being on the same side of the wound. Repeat with sutures ~1-2 cm apart until the wound closure is sufficient. **This particular suture type helps relieve wound tension. Subcuticular Typically, a resident will begin this type suture for the student. (see below for instructions for starting subcuticular sutures) Travel horizontally across the wound, taking a “bite” that is parallel with the skin surface in the subcuticular tissue. **At the wound edges, take as small “bites” as possible!! Travel horizontally back across the wound, and repeat this motion in a zig-zag form until you close the entire wound. Tie a knot using the “loop” of your last bite of skin. Do NOT cut the suture. Bury the knot by taking a bite through the wound, bringing the needle up lateral to the wound. Often, subcuticular sutures are finished using a type of skin adhesive and gauze dressing. Be sure to ask the resident or attending how to dress the wound. Starting a subcuticular suture: *Always be sure to ask the surgeon’s preferences with technique before starting subcuticular suturing. Option 1: Take a small, deep bite of subcuticular tissue on ONE side only. Tie a knot and trim the tail. Push the point of the needle through the apex of the wound, coming out just under the skin in the subcuticular tissue. o Subcuticular sutures NEVER go through the skin. Option 2: Take a small, deep bite of subcuticular tissue and travel horizontally to take a second bite, much like a horizontal mattress. The suture tail should be in the center of the wound, and your second bite should come out in the wound. Tie these two ends together. Trim the tail, then push the point of the needle through the subcuticular tissue at the apex of the wound, coming out just under the skin.