Christiane Thienelt, MD
advertisement

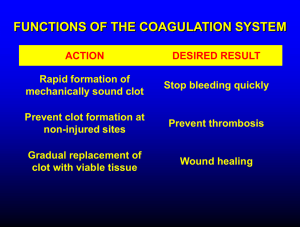
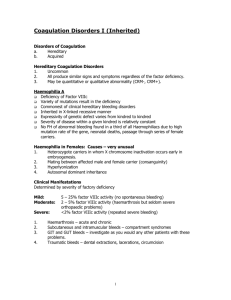
Christiane Thienelt, MD Introduction to CoagulationBleeding disorders and Thrombotic disorders Objectives A. Hemostasis 1. Physiology of coagulation -Define primary and secondary hemostasis -Understand the basic concept of intrinsic vs. extrinsic pathway -Know basic Laboratory tests to measure hemostasis (PTT, PT, INR, Bleeding time/PFA-100) 2. Abnormal coagulation=Bleeding disorders -Name 3 congenital bleeding disorders -Describe the basic process and components of obtaining a bleeding history -Describe typical bleeding symptoms in von Willebrand disease -Understand the physiologic function of the von Willebrand protein n coagulation -Describe typical bleeding symptoms in Hemophilia A and B -Know the inheritance pattern of von Willebrand disease and the hemophilias -Know basic principles of treatment of von Willebrand disease and for hemophilias -Explain the mechanism of action for the drug aminocaproic acid and how it can be helpful in dental patients 3. Thrombocytopenia -Name 3 mechanisms that can lead to low platelet counts -Know at least 2 medications that inhibit platelet function B. Thrombosis 4. Pathophysiology of arterial and venous thrombosis -Know typical risk factors for development of deep venous thrombosis versus arterial thrombosis -Know at least 3 symptoms of venous thrombosis (DVT and pulmonary embolism) 5. Hypercoagulable states =clotting disorders -Name 3 congenital clotting disorders -Know at least 2 acquired hypercoagulable states -Describe the typical treatment of an acute thrombotic event -Describe the mechanism of action for heparin (unfractionated and Low molecular weight heparin=LMWH) -Know how unfractionated heparin is monitored -Describe the mechanism of action for warfarin, understand half-life, monitoring and side effects -Describe the process of “bridging” patients with heparin Introduction to CoagulationBleeding disorders and Thrombotic disorders Hemostasis is the process whereby an injury to a blood vessel triggers a series of enzymatic reactions resulting in the formation of platelet and fibrin plugs at the site of the injury which then stems the loss of blood. This process is tightly controlled so that a clot remains at the site of the injury and is not pathologically propagated throughout the vascular system. After the clot is formed, then other enzymatic processes will dissolve the clot gradually as wound healing advances. A. Components of Hemostasis 1. Coagulation factors 2. Platelets 3. Endothelium – vessel wall Role of Platelets in Coagulation. Platelets adhere to the site of vessel injury where collagen is exposed. A plasma protein, von Willebrand factor and a platelet membrane protein, are involved with the adherence. The platelets become activated by the generation of thrombin at the site of the injury and as the platelets are stimulated receptors for fibrinogen are exposed. These activated platelets change shape and release ADP, vasoactive amines and form thromboxane A2. Thromboxane contracts smooth muscle and causes vasoconstriction of the vessel at the site of the injury which also helps stop the leakage of blood. The platelet has receptors for some of the coagulation proteins and forms the surface for the coagulation cascade with the end result in increasing the production of thrombin. Tissue factor from injured endothelium activates factor VII (Extrinsic pathway) and the phospholipid complex expression on the platelets and the vessel walls leads to activation of the Intrinsic pathway. Clot formation. The coagulation cascade is activated when sub-endothelial components (collagen, tissue factor or negatively charged surfaces) are exposed at the injured site. The procoagulant proteins circulate in excess concentration in the plasma in an inactive form or zymogen. Only a small percentage of the pro-enzymes need to be activated by proteolytic cleavage to form the clot. The goal of the series of reactions known as the coagulation cascade is to produce thrombin (Factor IIa). The thrombin converts fibrinogen, a soluble protein, to fibrin which makes a fibrous network in the clot. Thrombin also promotes platelet aggregation so that at the same time fibrin is being formed a firm mass of aggregated platelets and fibrin together make a plug that seals the injury in the vessel. Thrombin is also important in activating the cofactors in the coagulation cascade (Factors V and VIII), as well as activating the factors responsible for lysing the clot (fibrinolytic factors) and activates protein C which helps prevent uncontrolled thrombosis. The coagulation cascade is shown in the schema below. These factors (enzymes) do not act on each other individually, but actually come together to form complexes on phospholipid surfaces at the site of the injury. The surface could be the platelet membrane or the vessel wall. In each complex, there will be a large molecular weight cofactor which orients the enzyme and substrate molecules. Examples of this are tissue factor, Factor VIII, and Factor V. The next component would be one of the vitamin K dependent factors which are serine proteases. These are Factors X, IX, VII, and II, which is also known as prothrombin. The third component is calcium. When all of these components combine on the phospholipid surface, the relative efficiency of the production of activated factors is enormously increased. In this way thrombin (activated Factor II) is generated by Factor Xa. Xa itself is generated by Factors IXa and VIIIa or by tissue factor and VIIa. The thrombin that is produced by these reactions then converts fibrinogen to a clottable derivative called fibrin monomer, which assembles to form an infinite branching network of fibrin. Thrombin also activates a factor, Factor XIII, which is an enzyme that crosslinks the fibrin and hardens the fibrin clot. PT (protime) is affected by VII, X, II and fibrinogen. aPTT (activated Partial Thromboplastin time) is affected by XII, XI, IX, VIII, and X. TT (thrombin time) is affected by deficient or abnormal fibrinogen. Control of Coagulation. It is very important that the coagulation process be controlled, since uncontrolled pathologic clotting, also called thrombosis, can result in great morbidity. The activation of the clotting cascade and of platelets is inhibited by an intact vascular endothelium and by continuous blood flow which washes away platelets and any activated factors. In addition, there are a number of natural anticoagulant proteins. Anti-thrombin III is a protein that binds with high affinity to heparin and to thrombin and inactivates it. It also inactivates some other Factors XII, XI, IX, and X. Thrombin can activate another regulatory protein called protein C, which cleaves Factors Va and VIIIa, which are the cofactors of coagulation. Another protein, protein S, acts as a cofactor to protein C. Tissue factor pathway inhibitor inhibits Xa and the VIIa-TF complex. Physiologic Anticoagulants Antithrombin III Protein C and S Tissue Factor Pathway Inhibitor Thrombomodulin Fibrinolysis Fibrin is degraded by an enzyme called plasmin. The pro-enzyme plasminogen is activated by tissue plasminogen activator (TPA). Fibrin split products are formed. Fibrinolysis is inhibited by plasminogen activator inhibitors (PAIs) and alpha 2- antiplasmin. Role of Vitamin K in Coagulation. The serine proteases (Factors II, VII, IX, and X and the anticoagulant proteins C and S) all require a post translational modification of some of their glutamatic acid residues which requires vitamin K. The function of these factors is thus dependent upon both a source of vitamin K and on adequately functioning liver. The most common clinical disorders of coagulation result from inadequacies of these reactions. In addition, one of the most widely used anticoagulants, is a drug that interferes with this vitamin K dependent reaction – Warfarin (Coumadin). Evaluation of the Bleeding Patient One of the more important aspects of evaluating the bleeding patient, is to determine whether they have a congenital or an acquired abnormality. Therefore, the history of whether they have bled in the past or have a family history of bleeding, is very important. Bleeding after tonsillectomy or other surgical procedures and/or after teeth extraction is very suggestive of a congenital coagulopathy. Determining whether there is a history of exposure to agents that cause liver disease, other serious medical illness and medications will help determine whether there are causes for an acquired coagulopathy. There are specific assays for each of the factors, however, it would be very laborious and expensive to assay each of the factors individually in every person presenting with bleeding problems. Therefore, a number of screening tests have been devised which help pinpoint which part of the coagulation cascade is the most abnormal. Prothrombin Time (protime, PT). The protime (PT) measures the procoagulant activity of the factors VII, X, V, II and fibrinogen. This is the extrinsic pathway and the lower part of the coagulation cascade. The protime normal range is generally between 9 and 12 seconds, however this value is based on the potency of the material (thromboplastin) that is used to start the reaction in the laboratory. Therefore, the results are also reported as compared to an international normalized ratio (INR). An INR of 1.0 would be a normal value. The protime can be long because of a deficiency of any of the above mentioned factors, but the most common situation results from a deficiency of the vitamin K dependent factors, VII, X, and II either because of a lack of vitamin K or inadequate liver function. The drug, Warfarin, because of its affect in inhibiting the vitamin K dependent reactions, also results in a prolonged protime. The protime is used to monitor Warfarin therapy. Activated Partial Thromboplastin Time (APTT or PTT). The activated partial thromboplastin time (PTT) measures the procoagulant activity of the entire pathway. However, it is most sensitive to deficiencies of the higher numbered factors, especially XI, VIII and IX. It is not affected by deficiencies of Factor VII. The PTT can be prolonged also by anticoagulant drugs such as heparin or acquired anticoagulants such as fibrin split products. The normal range in most laboratories is usually 25-32 seconds. The PTT is used to monitor heparin therapy. Patients with hemophilia will have a prolonged PTT. Thrombin Time (TT). The thrombin time measures the procoagulant activity of fibrinogen and is also very sensitive to the anticoagulant affect of heparin or fibrin split products. The normal range is usually 12-18 seconds, if there is heparin contamination, fibrinogen deficiency or an abnormal fibrinogen it will be prolonged. Bleeding Time (BT). The bleeding time measures the platelet and vessel interaction, as well as the number and the function of platelets. It is performed by making a standardized cut with a simplate bleeding time device on the forearm. The time to clotting is then measured. This test is very operator dependent and takes meticulous attention to detail. In addition, it is affected by abnormalities in the skin. The normal bleeding time is generally between 2 and 9 minutes. A severe decrease in platelet count (less than 20,000-30,000) will cause a prolongation of the bleeding time, as will von Willebrand disease or abnormalities in platelet function. Other factor deficiencies do not prolong the bleeding time. PFA-100. A new device, the Platelet Function Analyzer, can perform a in vitro bleeding time. It also can determine platelet response to agonists. Congenital Disorders of Coagulation A deficiency of each factor shown in the Figure has been described, but most of these are extremely rare and they are outside the scope of this handout. Emphasis will be placed on the most common congenital coagulopathies which are the hemophilias and von Willebrand disease. Hemophilia A and B (Factors VIII and IX Deficiencies) Hemophilia A (Factor VIII deficiency) is the most common cause of a severe bleeding tendency. Hemophilia B (Christmas Disease or Factor IX deficiency) is ten times less common than Factor VIII deficiency. These two syndromes cause identical clinical problems and specific factor assays must be done to distinguish the two disorders. These two disorders are X-linked. This means that females are carriers and with rare exceptions, it is only the male offspring that are severely affected. The deficiency of Factor VIII or IX results in a prolonged PTT. In general, the longer the PTT, the more severe the hemophilia is. Assuming that pooled plasma from a normal population would give a value of 100%, we classify the hemophilia patients as to the residual percentage of factor activity they have. Many centers now offer genetic testing. Less than 1% factor activity – Severe Hemophilia. These patients suffer from spontaneous hemorrhaging into their joints, their muscles, soft tissues, retroperitoneal space and unfortunately, sometimes the central nervous system. Prior to specific factor replacement therapy this illness results in early death. If repeated bleeding in the joints is uncorrected in these hemophiliacs, very severe arthritis and eventual total destruction of the joints results. Current treatment with recombinant or purified factor products is very effective in preventing or stopping bleeding. 2% to 5% - Moderate Hemophilia. It usually takes some degree of trauma to cause bleeding in these patients. > 10% - Mild Hemophilia. Mild hemophiliacs only bleed after trauma and do not develop the chronic joint disease that the more severely affected patients do. However, when they do sustain trauma and develop joint or soft tissue bleeding, they need specific factor therapy just as urgently as the more severely affected patients in order to get resolution of the bleed. The absolute minimum levels of factor required for surgery are somewhere above 50%. Therefore, these patients will have hematoma formation, wound breakdown and prolonged disability if not replaced with factor aggressively during surgery. Because mild hemophiliacs do not present with spontaneous hemorrhage, in general they are diagnosed after a bad traumatic event or after a bad result from surgery. Once one mild hemophiliac is discovered, a vigorous attempt to screen all possibly involved family members should be made, since the other affected individuals may not come to medical attention until they have developed a serious bleed. 30% to 100% - Carrier Females. Because of lyonization of the x chromosome, the carriers of hemophilia A or B can be mildly affected themselves (30% factor level) or can be completely normal. Carrier females with bleeding are called symptomatic carriers and require life-long hemophilia follow-up. All potential carriers should be tested both for genetic counseling and also because those who have low factor levels will also require factor replacement after trauma and during surgery in order to get optimal results. Because factor levels cannot be solely used to determine carrier status, there are various molecular genetics methods available and families are encouraged to be evaluated. Factor XI Deficiency. Another congenital bleeding disorder is Factor XI deficiency. The levels are usually greater than 10% of normal so that spontaneous bleeding is quite rare in these persons. This deficiency is autosomal recessive so that both men and women can be affected. It is quite common in Ashkenazi Jews in the United States and in various populations in the Middle East. The classic presentation is post-operative hemorrhage since most people do not have spontaneous bleeding. The PTT will be prolonged and a specific factor assay for Factor XI must be done to make the diagnosis. von Willebrand Disease. von Willebrand disease is the most common mild congenital bleeding disorder. The von Willebrand protein is an extremely large protein that circulates in the plasma in a series of multimeric forms, that has two functions. One function is to adhere platelets to exposed collagen at the site of a wound. Therefore, von Willebrand protein is necessary for adequate platelet function and in von Willebrand disease, the bleeding time will be prolonged. The second function of von Willebrand protein is to carry Factor VIII. Without von Willebrand factor, Factor VIII has a very short half-life in the plasma. Therefore, if von Willebrand protein is decreased, the Factor VIII level will also be decreased. If the Factor VIII level is decreased severely, then the PTT will be prolonged. When we screen a patient for von Willebrand disease, we evaluate both functions of the von Willebrand protein. A standard screen would include: a bleeding time performed with the simplate bleeding device or PFA-100, a PTT, Factor VIII activity level, a level of the von Willebrand antigen (which describes how much of von Willebrand protein is present) and a test of the function of the von Willebrand protein known as the von Willebrand activity or ristocetin cofactor. See Table below. In addition, we can determine the pattern of multimeric forms of the protein in the plasma. von Willebrand disease can result as either a deficiency of normal von Willebrand protein (type I) or the presence of an abnormal protein (type II). Treatment with DDAVP (arginine vasopressin) is very effective in type I and less effective in type II, which is why we are interested in classifying the patients. von Willebrand disease is an autosomal dominant disease, therefore, both men and women are affected. Because of the abnormality in platelet function, patients often bleed from mucosal membranes, and nose bleeds, GI bleeds and menorrhagia are major clinical problems. In general, they have high enough Factor VIII levels to prevent joint or muscle bleeding, although they bleed after surgery if not corrected with DDAVP or factor concentrates. Tests for vWD 1. Bleeding time or PFA-100 – assess platelet function 2. vWF antigen – assess amount of factor present 3. vWF activity – assess function of factor to aggregate platelets with ristocetin 4. Factor VIII activity – assess ability of vWF to carry VIII 5. Multimeric analysis by electrophoresis – determine loss of large forms or abnormal bands 6. RIPA – (Ristocetin-induced-platelet-aggregation) – determine hyperaggrebility to ristocetin to diagnose Type 2b Type 1 Type 2 2b Type 3 Classification of vWD Partial quantitative deficiency Qualitative deficiency Abnormal clearance by platelets Severe or total quantitative deficiency Typical Results of Tests Type Assay vWF antigen vWF activity Factor VIII activity 1 2 40% 60% 30% 30% 50% 70% 3 <10% <5% 3% Bleeding time (min.) Multimers 7-15 10-30 >30 NL no large none seen Acquired Bleeding Disorders Acquired bleeding disorders are common. We use the screening coagulation tests to suggest diagnoses. Causes of a Prolonged PTT Heparin in Sample Hemophilia A and B (Factor VIII or IX Deficiency) Factor XI Deficiency Factor XII Deficiency* Acquired Hemophilia von Willebrand Disease Lupus Anticoagulant* *Patients do not bleed Causes of a Prolonged Protime ± PTT 1. Protime relatively more prolonged than PTT Liver disease Vitamin K deficiency Warfarin or rat poison ingestion 2. PTT more prolonged than protime Disseminated intravascular coagulation (DIC) Liver Disease. Most of the coagulation factors are synthesized by the liver. Therefore, abnormalities in hepatic function can cause deficiencies of the clotting factors. This is especially true for Factor V and for the vitamin K dependent Factors, II, VII, IX, and X. In very severe liver disease, the fibrinogen can be low also. Because the factors that are usually decreased affect the protime more than the PTT, the usual pattern of coagulation tests in a patient with liver disease, will be a prolonged protime with a relatively less prolonged PTT. The longer the protime is, the more severe the deficiency and the more likely that the PTT will also be slightly prolonged. If the fibrinogen level is decreased, the thrombin time may also be prolonged. These patients may also have consumption of platelets by their spleen due to portal hypertension, in which case they may have a decrease in platelet count as well. In patients with a prolonged protime due to liver disease, it is important to make sure that there is not a component of vitamin K deficiency exacerbating the problem thus, frequently trials of vitamin K therapy are done. Severe liver disease also causes abnormalities of the fibrinolytic system. There may be deficiencies of the endogenous anticoagulants also, such as antithrombin III and protein C and S. Vitamin K Deficiency and Warfarin Administration. Vitamin K deficiency and warfarin administration which interfere with the vitamin K utilization, are very common causes of a prolonged protime with normal or slightly prolonged PTT. Three of the vitamin K dependent Factors II, VII and X affect the protime mostly. Vitamin K is readily obtained from the diet so that in general vitamin K deficiency is a disease of patients who have no oral intake and have their gut flora (which can make vitamin K) killed by broad spectrum antibiotics. Unless vitamin K is replaced in a patient in the intensive care unit, who is NPO, on antibiotics and critically ill, he will become deficient, with increasingly prolonged protime in approximately five days. Since warfarin (Coumadin) interferes with vitamin K utilization, vitamin K deficient hospitalized patients are much more sensitive to small doses of warfarin than a normal patient and over-anticoagulation can quickly occur. Long acting fat soluble rat poisons are used in suicide attempts. These patients present with extremely prolonged protime and PTT and require very intensive vitamin K therapy for months, until the poison is eliminated. Disseminated Intravascular Coagulation (DIC). Massive trauma, hemorrhagic or septic shock, amniotic fluid embolism, burns, acute leukemia or transfusion and drug reactions can all cause disseminated intravascular coagulation. In this situation the coagulation cascade is activated in the vascular system with the result that fibrin and platelet microthrombi form and plug capillaries and cause tissue infarction. At the same time, some factors and platelets are consumed so that the patient develops multiple coagulation factor deficiencies and often hemorrhage results. The most consistent laboratory findings are that the fibrinogen level has decreased markedly and the platelet count is low. Because the fibrinolytic system is activated in order to try and remove the fibrin-platelet microthrombi, fibrin cleavage products are released into the circulation, and these are known as fibrin split products, (FSP) and can be measured in the laboratory. These fibrin split products inhibit the PTT assay, as well as the thrombin time, with the result that both of these tests will be markedly prolonged. In addition, Factor VIII and Factor V, which are the cofactors of coagulation, can be consumed. The usual pattern of laboratory abnormalities is shown in the Table below. Note that the PTT is increased relatively much more than the protime. This pattern of abnormalities is best distinguished from liver disease abnormalities in that the protime is usually the least affected (in contrast to liver disease) and the fibrinogen level is much lower in DIC than in the usual case of liver disease. When the underlying illness which caused the DIC is corrected, the fibrinogen will return quickly to normal and the platelet count will rise. Abnormalities in DIC Prolonged PT Greatly prolonged PTT Prolonged thrombin time Low platelet count Low fibrinogen level Increased fibrin split products Thrombosis Thrombosis is the formation and propagation of clot within the vasculature; this term refers to an abnormal or pathologic process with imbalance in the hemostatic system. This generally occurs when some combination of stasis (slowed blood flow), inflammation and/or vessel wall injury is present in a person with an increased baseline propensity for thrombosis (e.g. inherited or acquired hypercoagulable state). Hereditary and Acquired Thrombotic Disorders Thrombosis of the veins and arteries is among the most important causes of sickness and death in the developed countries of the world, with deaths from myocardial infarction and thrombotic stroke numbering >800,000 people annually. Between 500,000 and 2 million venous thromboembolic events are estimated to occur annually in the US alone. Massive pulmonary embolism accounts for 5 to 10% of all hospital deaths. The mortality rate for untreated PE is about 30% but can be reduced to 8% or less with optimal therapy. A substantial portion of patients (20-40%, depending on the population) with recurrent arterial or venous thrombosis are now known to have a hereditary or acquired defect that promotes thrombosis. It is important to identify patients with these abnormalities so that they can be protected during periods of thrombotic stress (such as around the time of a surgical procedure), so that affected family members can be identified, and so that specific therapy can be initiated when indicated. Virchow’s triad In 1854, German pathologist Rudolph Virchow postulated that vascular obstruction due to thrombosis resulted from three interrelated factors: 1. Decreased blood flow (venous stasis) 2. Inflammation of or near the blood vessels (altered vessels) 3. Intrinsic alterations in the nature of the blood itself (altered coagulability) While much more is understood about the nature and causes of thrombosis today, these three factors (“Virchow’s triad”) remain relevant and instructive today, when considering both arterial and venous thromboses. Arterial vs. Venous Thrombosis Arterial thrombi occur under conditions of high shear stress, a condition where von Willebrand factor is critical for platelet adhesion. They are composed primarily of aggregated platelets, containing small amounts of fibrin and few red cells, making them appear white in color (“white thrombi”). If they become large enough to lead to complete arterial occlusion, ischemia and infarction of the downstream tissues occurs. Clinical manifestations are dependent upon the organ involved (heart attack with coronary artery occlusion, stroke with cerebral artery occlusion, gut ischemia with mesenteric artery occlusion, etc). Abnormalities of blood flow which can contribute to development of thrombi include hypertension and turbulent blood flow at arterial branch points and at sites of focal atherosclerosis. Abnormalities of the blood vessel can include intraluminal vascular endothelial cell injury, atherosclerotic plaque rupture, hyperhomocysteinemia, aneurysm formation, and vessel dissection. Altered coagulability can be due to platelet activation, hyperviscosity such as may occur with certain malignancies, and thrombocytosis. In contrast, venous thrombi typically develop under conditions of slow blood flow (low shear stress). They are primarily composed of large amounts of fibrin containing numerous red cells (“red thrombi”). Stasis can be due to numerous factors, such as right-sided heart failure, pre-existing venous thrombosis, extrinsic vascular compression by tumor, immobility, obesity, and chronic venous insufficiency. Vascular factors contributing to venous thrombosis can include direct trauma or surgery, extrinsic compression, presence of a foreign body such as an IV catheter, and vascular endothelial cell injury due to exposure to toxins or excess levels of homocysteine. Altered coagulability can be due to inherited or acquired disorders of procoagulant proteins, deficiency of anticoagulant proteins, deficient fibrinolysis, and other factors such as use of oral contraceptives, pregnancy, malignancy, hyperhomocysteinemia, hyperviscosity, and the presence of antiphospholipid antibodies. Increased age also contributes to increased risk for thrombosis, likely due to multiple factors. Clinical Presentation of Venous Thromboembolic Disease Symptoms of deep vein thrombosis (DVT) and pulmonary embolus (PE) can be vague and nonspecific, making it difficult to make a diagnosis at times and making it important to have a high index of suspicion. It is estimated that up to 50% of DVT and PE are asymptomatic or undetected. The clinical signs and symptoms of DVT reflect the obstruction by clot of the deep veins in an extremity. On the severe end of the spectrum, complete obstruction of a proximal vein, such as a massive iliofemoral thrombosis, can produce nearly complete obstruction of venous outflow from an extremity, leading to a condition called phlegmasia ceruleans dolens (an extremely swollen, blue, painful leg). Lesser degrees of obstruction can produce pain, pitting edema of the distal extremity, and a warm, dusky, reddishblue discoloration of the skin caused by enhanced superficial venous blood flow. Sometimes these physical signs can be very subtle, requiring good light and asking the patient to stand for a few minutes to appreciate differences in size, warmth, color, or edema between normal and involved legs. One consequence of extremity DVT can be postthrombotic syndrome due to chronic venous insufficiency and chronic venostasis. Affected extremities become chronically swollen and painful and show dark skin discoloration. Cutaneous ulcers can develop, usually around the ankle when a leg is affected. Recurrent bouts of leg pain and swelling can occur due to intermittent obstruction of blood flow in the absence of formation of new thrombi. Another dreaded complication of DVT is PE, which occurs when part of a thrombus breaks off and travels through major veins, past the right heart, and into the pulmonary artery circulation until it becomes lodged. Lung tissue past the thrombus cannot participate in gas exchange and can infarct. If a clot involves both pulmonary arteries (saddle embolus) cardiovascular arrest and death can occur. DVT restricted to the calf veins uncommonly results in clinically important PE and is rarely associated with a fatal outcome. In contrast, inadequately treated DVT involving the popliteal or more proximal leg veins is associated with a 20 to 50% risk of clinically relevant recurrence and is strongly associated with both symptomatic and fatal PE. Classic signs and symptoms include sudden chest pain, dyspnea, anxiety, cough, syncope, and cyanosis. Hemoptysis can occur uncommonly, and patients can present with cardiac arrest and sudden death. Patients with small but recurrent PE can develop chronic dyspnea and chronic pulmonary hypertension with elevated right heart pressures. Significant mortality can occur if an unrecognized PE goes untreated. Diagnosis of DVT and PE A very useful screening test in these algorithms is the D-dimer assay. D-dimers can only be formed when cross-linked fibrin has been degraded by plasmin through fibrinolysis. So, in order for D-dimers to be formed, there must be formation of a clot, making the D-dimer assay an indirect measure of clot formation. D-dimer is a very sensitive but not specific test with high negative predictive value for DVT (i.e., a negative results rules out DVT – a positive result, however, doesn’t rule it in). With a positive Ddimer screening test, further studies should be performed. Venous ultrasound +/- US-Doppler (which can measure blood flow and pressure in blood vessels) has >95% sensitivity and specificity in patients with symptomatic DVT. For diagnosis of PE, spiral CT scan of the chest and ventilation/perfusion (V/Q) scans are the most commonly performed studies. An embolus in the pulmonary artery circulation can be directly visualized on CT scan. For the V/Q scan, two types of imaging are done. A gaseous radionuclide is inhaled to evaluate which parts of the lungs are being aerated with breathing. Then, another radionuclide is injected to assess how well blood circulates through the lungs. Mismatch between ventilation and perfusion (i.e., a localized area that ventilates well but is not perfused) may indicate a pulmonary embolus. Treatment of arterial thrombosis For arterial thrombi, in the acute setting, heparin (to prevent further clot formation) and a fibrinolytic agent such as tPA (to lyse the existing clot) are indicated. Time is of the essence due to the risk for tissue ischemia and infarction with delay in initiation of treatment. With arterial thrombi the pathophysiology of thrombus formation is primarily related to platelet activation and aggregation. Thus, in the more long-term setting where prevention is the main goal of therapy, antiplatelet agents are indicated in most situations. These can include aspirin (inhibits cyclooxygenase), the thienopyridines such as ticlopidine (Ticlid) and clopidogrel (Plavix)(ADP receptor antagonists), and the glycoprotein IIb/IIIa inhibitors such as abciximab (Reopro). Treatment of DVT and PE For venous thrombi, since activation of the coagulation cascade and formation of a fibrin clot is the main pathophysiologic mechanism, agents that inhibit coagulation are indicated. In the acute setting, unfractionated or low molecular weight heparin are used initially. These drugs act as cofactors to potentiate the activity of antithrombin III. In the long-term, low molecular weight heparin can be continued (requiring twice daily subcutaneous injections), or the patient can be switched to oral anticoagulation with warfarin (Coumadin). Warfarin acts by inhibiting the activity of vitamin K dependent enzymes (Factors II, VII, IX, X, Protein C, Protein S). Because it doesn’t affect the coagulation factors that have already been synthesized and released into the circulation, warfarin is not effective until enough time has passed to allow turnover of the factors. Of those factors, factor VII has the shortest half-life (5 hours) while the other factors have half-lives of 24 to 48 hours. Because factor VII will have the greatest effect on the PT/INR, the PT/INR will be prolonged before full anticoagulation has taken place. For that reason, it is important to maintain patients on heparin anticoagulation therapy at least 5 days after starting the warfarin to insure that full anticoagulation has taken place. Warfarin has a long half-life which is affected by many drugs and foods, so careful and regular monitoring of the PT/INR in patients taking warfarin is necessary to prevent under- or overdosing. Duration of anticoagulation therapy is determined on an individual basis based on a number of factors. The goal of treatment is prevention of DVT recurrence or clot extension and prevention of PE. Key in the decision-making process is determining if the DVT occurred due to transient risk factors (such as surgery, temporary immobilization, trauma, or pregnancy) or if the patient has an underlying hypercoagulable disorder or ongoing risk factors that require longer treatment. The location and severity of the clot also influences clinical decision making. The table on the following page shows one recommended approach. Hypercoagulable States The table below summarizes the prevalence of selected inherited and acquired hypercoagulable states. Patients often have a combination of defects. Not everyone with an inherited hypercoagulable state will develop an overt thrombosis, and not everyone with a thrombosis will have an identifiable hypercoagulable state. >60% of patients presenting with idiopathic venous thrombosis will be found to have an inherited hypercoagulable state. Many of the remaining 30-40% may have an acquired condition such as cancer or antiphosphlipid antibodies. Prevalence of selected inherited and acquired hypercoagulable states in different patient populations Hypercoagulable State Factor V Leiden Prothrombin G20210A Protein C deficiency Protein S deficiency Antithrombin deficiency Mild hyperhomocysteinemia Elevated factor VIII Lupus anticoagulant Elevated anticardiolipin antibodies General Population (%) 3-7 1-3 0.2-0.4 Unknown 0.02 5-10 11 0-3 2-7 Patients with First Venous Thromboembolism (VTE) 20 6 3 1-2 1 10-25 25 5-15 14 Hypercoagulable states exist when there is chronic damage to vessel walls, excess of procoagulant factors or a deficiency of anticoagulant factors or fibrinolytic activity. Thrombosis is often associated with interaction of multiple risk factors. Clues for the presence of an underlying hypercoagulable state: 1. a thrombotic episode in the absence of a defined precipitating condition (recent surgery, trauma, neoplasm, pregnancy, or prolonged immobilizing illness, etc.) or 2. recurrent episodes of thrombosis, or thrombosis at an early are and is otherwise healthy, or 3. a severe, life threatening thrombosis, or thrombosis at an unusual site (e.g. mesenteric or cerebral venous thrombosis), or 4. a family history of thrombosis, Inherited Thrombotic disorders Factor V Leiden (Activated Protein C Resistance) Due to an autosomal dominant mutation of the factor V gene that leads to partial resistance to inactivation through proteolytic cleavage by protein C. Factor V Leiden is inactivated 10 times more slowly than normal factor Va. Resistance to inactivation leads to increased risk for thrombosis. Factor V Leiden is the most common inherited predisposition to hypercoagulability in Caucasian populations of northern European background (up to 15%). Heterozygotes have a 4- to 7-fold increased lifetime relative risk of developing venous thromboembolism, and homozygotes are estimated to have an 80fold increased lifetime relative risk. Long-term anticoagulation therapy is not necessary for heterozygotes unless they experience more than one thrombotic event or life-threatening thromboembolism. Asymptomatic patients should not be treated but should be informed of increased thrombotic risk associated with other risk factors such as surgery, oral contraceptive use, or pregnancy. Prothrombin G20210A gene mutation This is the second most common inherited predisposition to hypercoagulability and has an autosomal dominant inheritance pattern. The mutation appears to lead to elevated concentrations of plasma prothrombin. Heterozygotes have a 2-6-fold increased lifetime relative risk of VTE. Indications for treatment are similar to those for factor V Leiden. Heterozygotes for both mutations (factor V Leiden and prothrombin G20210A) should have long-term anticoagulation following a first thrombotic event. Protein C Deficiency Protein C is a vitamin K-dependent plasma protein that, when activated, inactivates factors Va and VIIIa to inhibit coagulation. Deficiency is inherited in an autosomal dominant fashion. Most affected patients are heterozygotes with ~50% of normal protein C levels. The estimated increased lifetime relative risk of VTE is up to 31-fold. Homozygous deficiency of protein C leads to neonatal purpura fulminans, an often fatal disease associated with extensive venous or arterial thrombosis at birth and levels of protein C <5% of normal. Heterozygotes can also develop warfarin-induced skin necrosis. This problem typically occurs in patients started on large doses of warfarin in the absence of concomitant heparin therapy. Warfarin decreases the already low protein C levels more rapidly that the vitamin K-dependent procoagulant factors, leading to exacerbation of the basal hypercoagulable state. Asymptomatic patients should not receive anticoagulation but should avoid other risk factors and should receive prophylaxis for high-risk procedures such as surgery. Those with a single thrombotic event should receive 6-12 months of anticoagulation and those with more than one event, a single life-threatening event, or a strong family history of thrombosis should receive long-term anticoagulation. Protein C concentrates are available for those with homozygous deficiency. Protein S Deficiency Protein S is another vitamin K-dependent plasma protein that facilitates the anticoagulant activity of activated protein C. As with protein C, deficiency is inherited as an autosomal dominant trait. Patients can present with VTE or with arterial thrombosis, including stroke. Risk for thrombosis is higher when combined with other risk factors. Neonatal purpura fulminans and warfarin-induced skin necrosis can be seen. The estimated lifetime increased relative risk of thrombosis is up to 36-fold. Treatment principles are the same as those for protein C deficiency. Antithrombin Deficiency Antithrombin III regulates coagulation by inactivating thrombin as well as factors Xa, IXa, XIa and XIIa. AT-III deficiency is inherited in an autosomal dominant fashion. Most patients are heterozygous, having ~50% of normal activity levels. Homozygous deficiency is usually fatal in utero. The estimated increased lifetime relative risk of thrombosis is up to 40-fold. Deficiency of AT-III can sometimes lead to heparin resistance, since heparin acts as a cofactor for AT-III and, thus, lack of AT-III limits the therapeutic effectiveness of heparin. Asymptomatic patients should not be treated. Patients with a single thrombotic event should receive at least 3-6 months of anticoagulation. Patients with massive VTE or PE should be considered for thrombolytic therapy. Pregnant patients or patients undergoing surgery should receive prophylaxis, including AT concentrate administration. Other risk factors Hyperhomocyteinemia can be inherited or acquired. The mechanism underlying increased risk for thrombosis may be enhanced platelet activation and adhesiveness due to endothelial cell injury. Increased factor VIII activity (>150%) can lead to a 3-6 fold greater relative risk of VTE. The risk increases to 11-fold with activity levels >200%. Impaired fibrinolysis (plasminogen deficiency, tPA deficiency, etc) can lead to increased risk for thrombosis. Oral contraceptives have been a well-recognized acquired risk factor for thrombosis since their introduction in the 1960’s. The likely mechanism is alteration in levels of coagulation factors leading to a net increased risk for thrombosis. The risk is greatly increased in combination with other risk factors. For example, factor V Leiden alone leads to a 4-7 fold increased relative risk for thrombosis while factor V Leiden in combination with oral contraceptive use leads to a 30-35 fold increased risk. The Lupus Anticoagulant. The lupus anticoagulant is a very common acquired abnormality which results in a hypercoaguable state. The anticoagulant is an IgG antibody, which reacts against phospholipid in the platelet membrane or endothelial cell. The syndrome caused by the lupus anticoagulant is called the Antiphospholipid Antibody Syndrome or APL. The lupus anticoagulant is detected because it prolongs the PTT since the antibody binds up the phospholipid which is added to the test tube in order to start the reaction. Even though the PTT is prolonged in vitro, the patients do not have a bleeding tendency, instead they have a thrombotic syndrome which includes deep vein thrombosis, pulmonary embolism, thrombotic strokes and recurrent miscarriage due to thrombotic disease of the placental blood vessels. When normal plasma is mixed with the plasma from a patient with the lupus anticoagulant, the PTT does not correct. If, however, the patient’s plasma is first mixed with a source of phospholipid such as platelets, the antibody will be absorbed out of the plasma by the phospholipid and a repeat PTT will show partial correction. There are other methods also of detecting the lupus anticoagulant such as the dilute Russell’s Viper Venom Test (RVVT). It is extremely important to diagnose the lupus anticoagulant because these patients with thrombotic tendency must be distinguished from other patients with prolonged PTT’s who have a bleeding tendency, since treatment is entirely different. Although, it is named the lupus anticoagulant, a minority of the patients have lupus. They may have other autoimmune illness, malignancy, a recent infection or it may be drug induced by antibiotics or anti-psychotic drugs. Sources: 1. Wintrobe’s Clinical Hematology, 12th Edition. Ed. JP Greer et al. 2009. 2. Disorders of Hemostasis and Thrombosis, 2nd Edition. Ed. SH Goodnight and WE Hathaway. 2001. 3. Hematology for the Medical Student. Ed. AH Schmaier and LM Petruzzelli. 2003.