Afrouzian M1, Thomas P2, Kadambi P3, Solez K4
advertisement

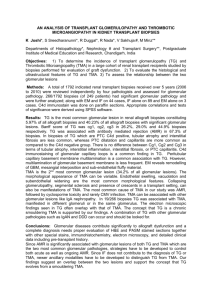
Afrouzian M1, Thomas P2, Kadambi P3, Solez K4 1 Department of Pathology, University of Texas Medical Branch, Galveston, USA 2 Department of Surgery, Transplantation surgery, University of Texas Medical Branch, Galveston, USA 3 Department of Internal Medicine, Division of Nephrology, University of Texas Medical Branch, Galveston, USA 4 Department of Pathology, University of Alberta, Edmonton, Canada Role of peritubular capillary thrombosis in renal allograft rejection Background: Microthrombus formation in peritubular capillaries (Ptcs) is a phenomenon that has not been fully explored in renal transplantation pathology. The only study on human allografts that addresses the presence of thrombi in Ptcs of rejecting kidneys has been published by Meehan and Haas in 2003 and since then, this subject has remained untouched. In an earlier animal study, we have reported the presence of microthrombi in Ptcs of rejecting grafts in the ϒInterferon and the ϒ-Interferon Receptor knock out model. In these mice models of transplantation, microthrombi appear in Ptcs before the grafts undergo hemorrhagic/ coagulative necrosis. The significance of this phenomenon is not known: Whether or not it is associated with ABMR in human allografts or with other lesions such as bacterial infection, drug toxicity, polyoma virus nephropathy, are questions that deserve attention. Objectives: The primary goal of this study was to determine the incidence of this lesion in human allografts. The secondary goal was to explore its relationship with antibody- mediated rejection (ABMR), T cell-mediated rejection (TCMR), thrombotic microangiopathy (TMA), Polyoma virus nephropathy (PVN) and drug toxicity (CNI tox). Material and Methods: A total of 84 renal transplant biopsies with renal allograft dysfunction, reported between January 2012 and April 2013 at the UTMB Department of Pathology were reviewed by a single pathologist. Thirteen native kidney biopsies with no evidence of coagulopathy were used as control. To detect fibrin, all biopsies were stained with Martius-Scarlet –Blue (MSB) and assessed for presence of microthrombi in Ptcs and in glomeruli. Immunofluorescence and electron microscopy material were reviewed on all biopsies in search of intraluminal and sub-endothelial fibrin tactoids, platelet aggregates, and signs of endothelial injury, including sub-endothelial widening, loss of endothelial cell fenestration, cytoplasmic swelling, or fragmentation and apoptosis. All allograft biopsies were studied for the presence of C4d in peritubular capillaries. Finally, using the Banff diagnostic categories for renal allograft biopsies (2009), findings were correlated with the following diagnoses: ABMR, TCMR, Borderline changes (Brd), TMA, CNI tox, PVN, interstitial fibrosis and tubular atrophy (IFTA), Transplant glomerulopathy (TG), and bacterial pyelonephritis (Pyelo). Results: Ptc thrombosis was present in: 25/71 (35%) of allograft biopsies; 7/17 cases with Acute AMR; 9/25 cases with TCMR; 1/5 cases of Brd; 10/13 cases of TMA; one case of atypical HUS; 3/4 cases with PVN; 2/7 cases with IFTA; 2/4 cases of pyelonephritis and in none of the two cases diagnosed as TG. None of the native kidney biopsy (controls) showed evidence of thrombosis in ptcs. Presence of microthrombi in peritubular capillaries strongly correlated with only 3 parameters: the presence of fibrin in glomeruli (p<0.0001), the diagnosis of TMA (p<0.0001); and the diagnosis of CNI tox (p = 0.045). Conclusion: Ptc thrombosis is a lesion that has been overlooked in renal transplant pathology, despite the fact that it is not a rare finding: We demonstrated the presence of Ptc thrombosis in one third of our allograft biopsies. Our results show that Ptc thrombosis has a strong association with endothelial cell injury in both peritubular capillaries and glomeruli. Diagnoses of TMA, proven by electron microscopy, and CNI tox, also have significant association with Ptc thrombosis. We suggest that Ptc thrombosis is a sign of endothelial cell injury in the microvasculature and should be considered as an important lesion for the detection of TMA, possibly related to CNI tox. To our surprise, Ptc thrombosis did not show any association with ABMR which also affects both glomerular and peritubular capillary endothelium and causes TMA.