Neurological assessment Neurological outcome as daily assessed
advertisement
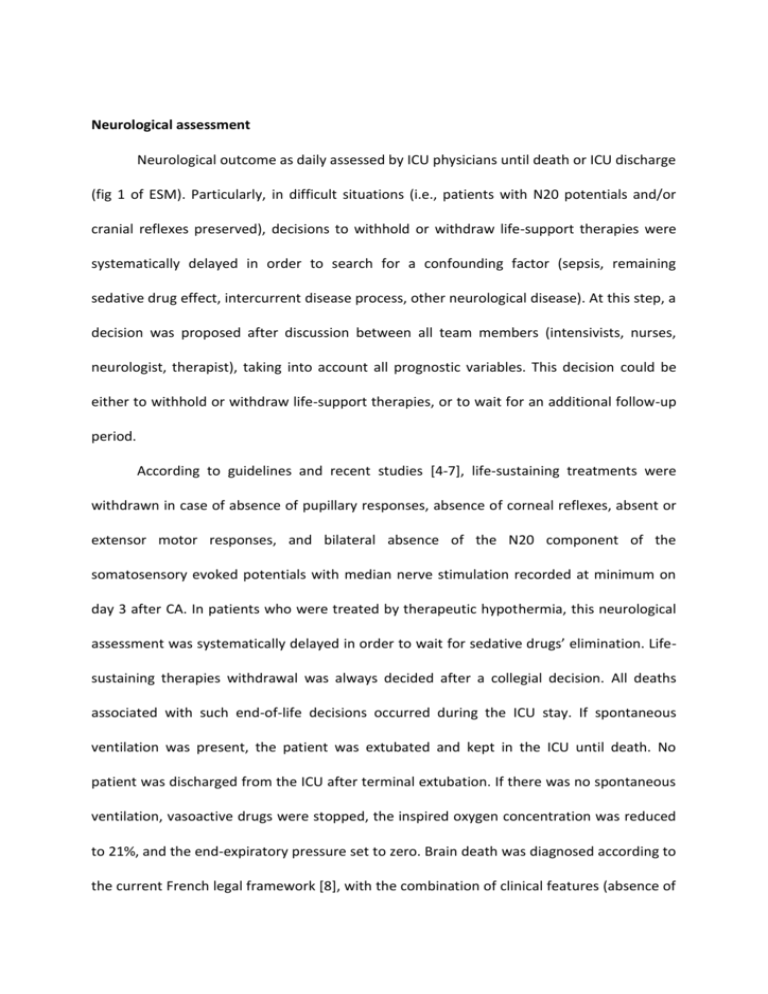
Neurological assessment Neurological outcome as daily assessed by ICU physicians until death or ICU discharge (fig 1 of ESM). Particularly, in difficult situations (i.e., patients with N20 potentials and/or cranial reflexes preserved), decisions to withhold or withdraw life-support therapies were systematically delayed in order to search for a confounding factor (sepsis, remaining sedative drug effect, intercurrent disease process, other neurological disease). At this step, a decision was proposed after discussion between all team members (intensivists, nurses, neurologist, therapist), taking into account all prognostic variables. This decision could be either to withhold or withdraw life-support therapies, or to wait for an additional follow-up period. According to guidelines and recent studies [4-7], life-sustaining treatments were withdrawn in case of absence of pupillary responses, absence of corneal reflexes, absent or extensor motor responses, and bilateral absence of the N20 component of the somatosensory evoked potentials with median nerve stimulation recorded at minimum on day 3 after CA. In patients who were treated by therapeutic hypothermia, this neurological assessment was systematically delayed in order to wait for sedative drugs’ elimination. Lifesustaining therapies withdrawal was always decided after a collegial decision. All deaths associated with such end-of-life decisions occurred during the ICU stay. If spontaneous ventilation was present, the patient was extubated and kept in the ICU until death. No patient was discharged from the ICU after terminal extubation. If there was no spontaneous ventilation, vasoactive drugs were stopped, the inspired oxygen concentration was reduced to 21%, and the end-expiratory pressure set to zero. Brain death was diagnosed according to the current French legal framework [8], with the combination of clinical features (absence of motor response, spontaneous ventilation and brainstem reflex) and the absence of electroencephalographic activity or cerebral perfusion during cerebral CT scan. References 1. Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, Bossaert L, Delooz HH, Dick WF, Eisenberg MS, et al. (1991) Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 84:960-75. 2. Nolan JP, Morley PT, Vanden Hoek TL, Hickey RW, Kloeck WG, Billi J, Böttiger BW, Morley PT, Nolan JP, Okada K, Reyes C, Shuster M, Steen PA, Weil MH, Wenzel V, Hickey RW, Carli P, Vanden Hoek TL, Atkins D; International Liaison Committee on Resuscitation. (2003) Therapeutic hypothermia after cardiac arrest: an advisory statement by the advanced life support task force of the International Liaison Committee on Resuscitation. Circulation. 108:118-21. 3. Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT Jr, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez-Nunez A, Sellke FW, Spaulding C, Sunde K, Vanden Hoek T. (2008) Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 118:2452-83. 4. Morley PT, Atkins DL, Billi JE, Bossaert L, Callaway CW, de Caen AR, Deakin CD, Eigel B, Hazinski MF, Hickey RW, Jacobs I, Kleinman ME, Koster RW, Mancini ME, Montgomery WH, Morrison LJ, Nadkarni VM, Nolan JP, O'Connor RE, Perlman JM, Sayre MR, Semenko TI, Shuster M, Soar J, Wyllie J, Zideman D. (2010) Part 3: Evidence evaluation process: International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 122:S283-90. 5. Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL. (2010) Part 9: postcardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 122:S768-86 6. Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S. (2006) Quality Standards Subcommittee of the American Academy of Neurology. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 67:203-10. 7. Booth CM, Boone RH, Tomlinson G, Detsky AS. (2004) Is this patient dead, vegetative, or severely neurologically impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA. 291:870-9. 8. [No authors listed] (1968) A definition of irreversible coma. Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death. JAMA. 205: 337-40. 9. Décret no 96-1041 du 2 décembre 1996 (1996) relatif au constat de la mort préalable au prélèvement d'organes, de tissus et de cellules à des fins thérapeutiques ou scientifiques et modifiant le code de la santé publique (deuxième partie : Décrets en Conseil d'Etat). JORF 282 : 17615 Figure 1 ESM : decision algorithm for post-CA patients. EEG: electro-encephalogram; ICU: Intensive Care Unit.