Oral Contraceptive Pill item
advertisement
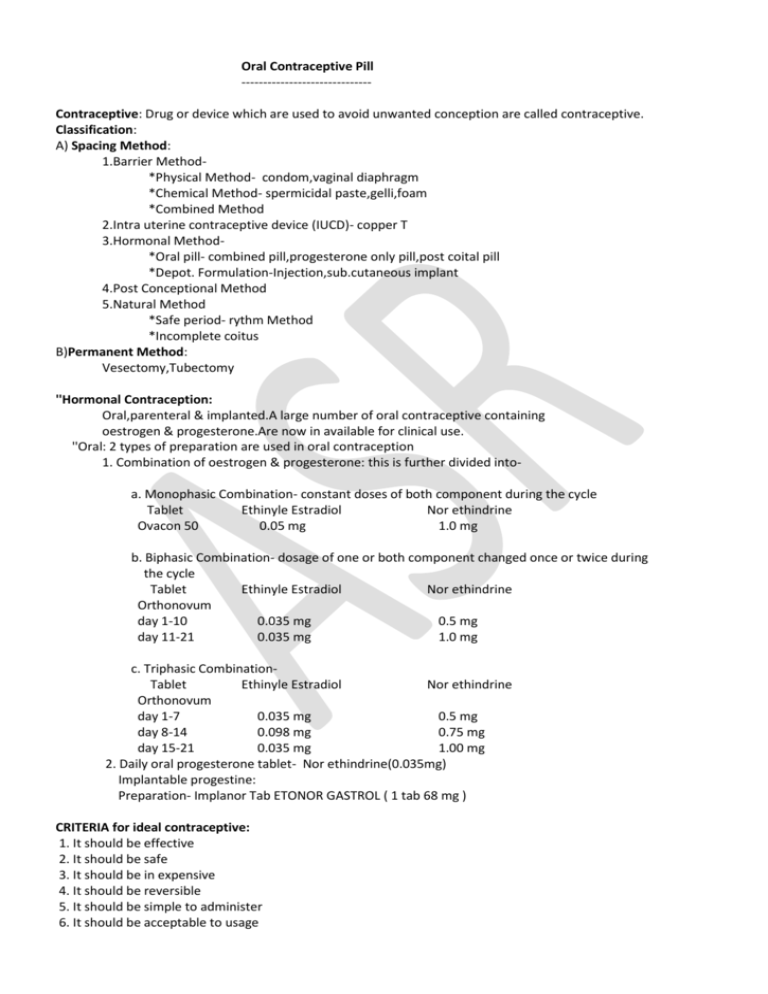
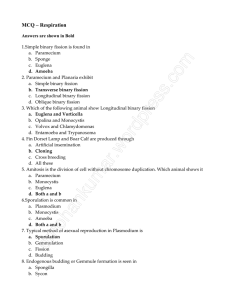
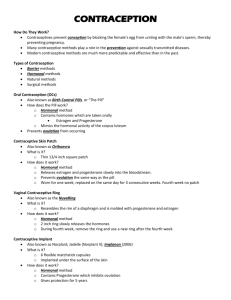
Oral Contraceptive Pill -----------------------------Contraceptive: Drug or device which are used to avoid unwanted conception are called contraceptive. Classification: A) Spacing Method: 1.Barrier Method*Physical Method- condom,vaginal diaphragm *Chemical Method- spermicidal paste,gelli,foam *Combined Method 2.Intra uterine contraceptive device (IUCD)- copper T 3.Hormonal Method*Oral pill- combined pill,progesterone only pill,post coital pill *Depot. Formulation-Injection,sub.cutaneous implant 4.Post Conceptional Method 5.Natural Method *Safe period- rythm Method *Incomplete coitus B)Permanent Method: Vesectomy,Tubectomy ''Hormonal Contraception: Oral,parenteral & implanted.A large number of oral contraceptive containing oestrogen & progesterone.Are now in available for clinical use. ''Oral: 2 types of preparation are used in oral contraception 1. Combination of oestrogen & progesterone: this is further divided intoa. Monophasic Combination- constant doses of both component during the cycle Tablet Ethinyle Estradiol Nor ethindrine Ovacon 50 0.05 mg 1.0 mg b. Biphasic Combination- dosage of one or both component changed once or twice during the cycle Tablet Ethinyle Estradiol Nor ethindrine Orthonovum day 1-10 0.035 mg 0.5 mg day 11-21 0.035 mg 1.0 mg c. Triphasic CombinationTablet Ethinyle Estradiol Nor ethindrine Orthonovum day 1-7 0.035 mg 0.5 mg day 8-14 0.098 mg 0.75 mg day 15-21 0.035 mg 1.00 mg 2. Daily oral progesterone tablet- Nor ethindrine(0.035mg) Implantable progestine: Preparation- Implanor Tab ETONOR GASTROL ( 1 tab 68 mg ) CRITERIA for ideal contraceptive: 1. It should be effective 2. It should be safe 3. It should be in expensive 4. It should be reversible 5. It should be simple to administer 6. It should be acceptable to usage 7. It should be require little or no Pharmacological Effect: 1. Selective inhibition of pituitary function that results inhibition of ovulation 2. The combination agent also produce change in cervical mucosa,uterine endometrium,sensation of uterine tube. All of which decrease conception & implantation. Beneficial effect of oral contraceptives: 1. reduce risk of ovarian cysts 2. reduce risk of ovarian & endometrial cancer 3. reduce risk of benign breast disease 4. treatment of endometriosis 5. lower incidence of ectopic pregnency 6. relief premenstrual symptoms 7. release dysmenorrhoea 8. disfunction of uterian bleeding prevent ADVERSE effect: Milda) nausea, mastalgia, break through bleeding, oedema b) headche is mild & often transient c) withdrawl bleeding sometimes fail to occur Moderatea) break through bleeding b) weight gain c) increase skin pigmentation, acne d) urethral dilation e) vaginal infection f) amenorrhoea Severea) Cardio vascular disorder- hypertension,myocardial infarction, venous thrombo embolic disorder b) cholestatic jaundice c) depression d) cancer e) atheros scoloris Contra Indication of combined oral pill: 1. Absolutea) Cardio vascular disorder b) past history of disphenomenon c) known or suspected tumour of breast 2. Relativea) family history of venous thrombo embolism b) diabetes mallitus c) hypertension d) obesity e) smoking f) breast feeding g) asthma progesterone only contraception:: 1. the progesterone used oralya) include- norgestrol,levogestrol,desogastrol b) it is less effective than combined OCP 2. intramuscular progesteronea) Depot medroxy progesterone acetate ( DMPA )= 150 mg 3 month by deep I.M b) nor ethisterone cnanmate = 200 mg 2 month by deep I.M Advantage: 1. progesterone doesn't interfear milk secration.so it is safe for lactating mother 2. it is ideal for women contraindicated for estrogen Contra indicationa) history for thrombo embolism b) diabetes c) smoker over 35 years Disadvantage: 1. delay in return of fertility 2. menstrual disterbance Mechanism of combined oral pill: 1. inhibiting ovulation 2. produce cervical mucous impenetrable to sperm Sub dermal Implantation: subdermal implantation of capsules containing progesterone 1. levonorgastrol ( nor plant ) = 36 mg for 5-6 years 2. etonorgastrol ( implantor ) = for 2-4 years **A flexible rod inserted into the flexor surface of upper arm Disadvantage of subdermal implantation: 1. surgical procedure 2. irregular bleeding 3. headche 4. visual disterbance Post menoposal hormone replacement therapy: HRT - hormone replacement therapy refers to the use of oestrogen & progesterone. in order to reverse of prevent symptom produce by absence of this 2 hormone, menopose or premenoposal sergical removal of ovary. Causes of cessation of normal ovarian function: 1. after menopose 2. oophorectomy 3. premature ovarian failure AIM of HRT: a) to reduce the symptoms of oestrogen loss1. hot flushes 2. sleep lessness 3. lethargy 4. depression b) to reduce the long term complication of oestrogen deficiency1. coronary heart disease Preparation of HRT: a) patient who has undergoes histectomy ( surgical removal of uterus ) b) in women who haven't undergoes histectomy require oestrogen combined with progesterone to prevent endometrial proliferation. 1. sequential regimen - women take oestrogen without break & add a progesterone from approximately 14-28 day of each. 2. contineous regimen - approximate only who have been amenorrhoea for more than 1 year. **Fixed doses of combination of oestrogen & progesterone taken without break. ADVERSE effect of HRT: 1. irregular or withdrawl bleeding 2. venous thrombo embolism 3. carcinoma of endometrium or breast 4. risk of gall stone Contra indication of HRT: 1. recent arterial or venous thrombo embolic disorder 2. history of oestrogen dependent neoplasm 3. diabetes, hypertension, gall stone, liver disease.