IMPACT-ICU Project Summary April 2014 What is the IMPACT
advertisement

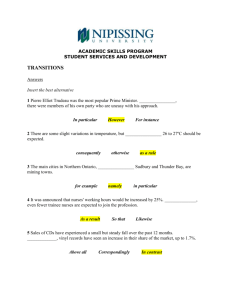
IMPACT-ICU Project Summary April 2014 What is the IMPACT-ICU Project? The IMPACT-ICU project is an quality improvement program designed to increase integration of palliative care into the ICU by training and supporting ICU bedside nurses to identify and address needs in 3 domains: 1) patient symptom management, 2) family support, and 3) multidisciplinary communication about prognosis and goals of care. Why was the IMPACT-ICU Project Developed? The IMPACT-ICU project was developed by a multidisciplinary and multi-specialty team at the University of California, San Francisco Medical Center, in response to requests from critical care nurses for training in communication and increased support from the palliative care consult team in the ICU When integrated into the ICU, palliative care can improve outcomes in all domains of the triple aim: patient and family health, experience of care, and resource utilization (Figure). Successful and sustained integration of palliative care into the ICU requires involvement of nurses, patients’ closest bedside provider. In a system-wide survey of 597 critical care nurses at the 5 University of California medical centers, lack of training was the most frequently cited barrier to nurses’ involvement in these discussions of prognosis, goals of care, and palliative care with families and other clinicians. What are the IMPACT-ICU Project Components? The IMPACT-ICU project has two main components: 1) a workshop to train nurses to facilitate communication about prognosis, goals of care and palliative care among families and physicians, and 2) rounding in the ICUs by advance practice nurses to support bedside nurses as they screen and address palliative care needs for their patients. Communicaiton workshop is 8-hours long, and uses learner-centered methods and role-play to practice core communication skills in palliative care. Role-plays help nurses practice addressing patient needs through conversations with families, physicians, and in family meetings to mimic their practice (Figure and Table). A reflection session teaches practices to address nurses’ distress & burnout. Wendy Anderson MD MS, Wendy.Anderson@ucsf.edu In the rounding component of the project, palliative and critical care advance practice nurses and educators round in target ICUs at each center. These nurse leaders support bedside nurses to identify palliative care needs, and work with ICU clinicians to address identified needs. Bedside nurses are trained to screen patients for uncontrolled symptoms, family distress, and communication needs. Nurse leaders provide direct access to specialty palliative nursing, to help bedside nurses troubleshoot challenges. Palliative care consult services are involved when the ICU clinicians require assistance with complicated cases. ICU & Medical Teams Palliative Care Consult Service ICU Bedside Nurse Advanced Practice Palliative Care Nurse Social Work Spiritual Care Service Where has the IMPACT-ICU Project Been Implemented? After being piloted at the University of California, San Francisco Medical Center, the IMPACT-ICU project was disseminated to all of the University of California (UC) Medical Centers: UC Irvine, UC San Diego, UC Los Angeles, and UC Davis. This dissemination was made possible by generous support from the UC Office of the President Center for Health Quality and Innovation Quality Enterprise Risk Management (CHQIQERM) program, a joint venture of the University of California Center for Health Quality and Innovation and Office of Risk Services. How has the IMPACT-ICU Project Been Received in the University of California System? The project has been very well received in the UC system. It has enjoyed broad support from the campus Chief Nursing, Medical, and Risk Officers, all of whose approval was required to implement the project. 250 nurses have completed the communication workshop. Evaluations show that after the workshop, nurses feel that they have a higher level of skill to engage in discussions with clinicians and families about prognosis, goals of care, and palliative care, compared to before completing the workshop (Figure). Figure: Workshop Evaluations. Participants rated their skill to engage in palliative care communication tasks before and after the workshop. Response options were: “Excellent”, “Very Good”, “Good”, “Fair”, “Poor”; the chart shows the percentage of nurses rating their skill as “Excellent” or “Very Good”. All differences before vs. after workshop are significant at p<0.001. Use self-care practices to prevent burnout and compassion fatigue 26% Communicate the value of a palliative care consultation to a physician 27% 71% 69% Elicit a family’s understanding of a patient’s goals of care 34% 71% Before Workshop Provide families with emotional support during family meetings 37% Ensure that a family member understands information presented in a family meeting 37% After Workshop 67% 75% Identify a family’s need for information about a patient’s illness and treatments 48% 78% % of nurses rating their skill as "Excellent" or "Very Good" Program evaluation is ongoing. Key processes and outcomes of care include support provided to nurses in the target ICUs, nurses’ confidence in communication, frequency of clinician-family discussions and documentation in the medical record, family satisfaction, and utilization including length of stay and costs. Is Training Available to Implement the IMPACT-ICU Project in Other Hospitals and Health Systems? Yes! In the process of implementing the program the UC campuses, we have developed a faculty development program that could be used to disseminate the program to other hospitals and systems. IMPACT-ICU Project Summary April 2014, Page 2 Wendy Anderson MD MS, Wendy.Anderson@ucsf.edu